Introducción: Las estenosis yuxtaanastomóticas son la causa más frecuente de disfunción en las fístulas radiocefálicas (FAV RC) para hemodiálisis. Estas estenosis provocan bajo flujo de la fístula con mala calidad de la diálisis y pueden evolucionar a la trombosis del acceso. El tratamiento de estas lesiones puede ser radiológico o quirúrgico; la elección de uno u otro es tema de discusión. En nuestro centro se utilizó por consenso el tratamiento quirúrgico de forma sistemática. Método: Hemos realizado un estudio prospectivo desde 1998 hasta 2009. Se incluyeron todas las FAV RC con disfunción o trombosis secundaria a una estenosis yuxtaanastomótica. El diagnóstico se realizó mediante fistulografía, salvo en los casos de trombosis, en los que fue clínico. El tratamiento en todos los casos fue quirúrgico, realizándose una nueva anastomosis radiocefálica proximal a la estenosis (RC PROX). Se analizó la permeabilidad (primaria y secundaria) tanto para las FAV RC iniciales como para las RC PROX utilizando curvas de Kaplan-Meier. Resultados: En el período de estudio se repararon 96 FAV RC con disfunción o trombosis, realizándose en todos los casos una nueva anastomosis RC PROX. El tiempo medio de seguimiento fue 57,27 meses (intervalo de confianza 95%: 47,53-67,02). La edad media de los pacientes fue de 67 años, con un mayor porcentaje de varones (68,7%). Las intervenciones (RC PROX) se realizaron de forma programada en 68 casos (70%) y de forma urgente por trombosis en el resto, evitándose el ingreso hospitalario del paciente en el 92%. La permeabilidad inmediata se consiguió en el 100% de los procedimientos. La permeabilidad primaria de este tipo de reparación (RC PROX) a 1, 2, 3, 4, 5 años fue respectivamente de 89,4%, 75%, 70,4%, 65% y 56%. En el seguimiento se realizaron 16 procedimientos quirúrgicos adicionales, alcanzando la intervención RC PROX una permeabilidad secundaria del 93,7%, 92,1%, 89,6%, 87% y 82,6% respectivamente. Con este tipo de mantenimiento la permeabilidad secundaria a los 1,2,3,4 y 5 años de la FAV RC iniciales fue respectivamente del 95%, 95%, 93,2%, 89,1% y 86,6%. Conclusiones: En nuestra experiencia, una nueva anastomosis proximal prolongó significativamente la permeabilidad de las FAV RC que presentaron estenosis yuxtaanastomóticas.
Introduction: The juxta-anastomotic stenosis is the most frequent cause of dysfunction in radiocephalic fistulas for haemodialysis. This adversity can cause low flow or thrombosis. The appropriate treatment of these lesions is under debate. Method: A prospective study was performed from 1998 to 2009. All dysfunctional radiocephalic fistulas due to juxta-anastomotic stenosis were included (n=96). The diagnosis was made by fistulografy in low flow cases and clinical evidence in cases of thrombosis. The repair was performed using a new proximal radiocephalic anastomosis in all cases. Patency following surgical intervention was estimated with the Kaplan-Meier method. Results: A total of 96 proximal radiocephalic anastomoses were performed during the study period. Mean surveillance time was 57.27 months (95% CI: 47.53-67.02). Sixty-six patients were male, and the mean age was 67 years. Scheduled surgery was performed in 70.5% of cases and 29.5% were emergency procedures, 92% of which were ambulatory. Technical success was achieved in 100% without any complications. Mean primary patency at 1, 2, 3, 4, and 5 years was 89.4%, 75%, 70.4%, 65%, and 56%, respectively. Additional procedures (n=16) were required in 14 cases (twelve new proximal anastomoses and four cases of arteriovenous graft placement), resulting in mean secondary patency at 1, 2, 3, 4, and 5 years of 93.7%, 92.1%, 89.6%, 87%, and 82.6%, respectively. Mean secondary patency of initial dysfunctional radiocephalic fistulas at 1, 2, 3, 4, and 5 years was 95%, 95%, 93.2%, 89.1%, and 86.6%, respectively. Conclusions: In our experience the proximal radiocephalic anastomosis can significantly extend fistula functionality in patients with juxta-anastomotic stenosis.
INTRODUCTION
In Spain, the incidence and prevalence of patients with chronic kidney disease requiring renal replacement therapy have increased by more than 100% in the last 15 years1 (from 61 and 392 patients per million population [pmp] in 1991 to 132 pmp and 1009 pmp in 2007, respectively). The age group with the highest percentage increase is that of patients older than 75 years (8.5% of prevalent patients in 1992 vs 40% currently). In this group, the majority of patients are treated with haemodialysis (94% of incident patients) and few switch between different dialysis techniques over the course of their lives.2
From the first description of the surgical technique for radiocephalic autogenous arteriovenous fistulas (RC AVF) by Cimino and Brescia in 1966,3 and in accordance with the clinical guidelines of the National Kidney Foundation (Guideline for Vascular Access No. 2.1), this type of fistula is proposed as the first choice for vascular accesses whenever possible,4-6 since this is the type of vascular access with the lowest associated morbidity and mortality rates. The drawback of this technique is the high rate of early failure and the low patency rates after the first year.7
The primary cause of RC AVF dysfunction is juxta-anastomotic stenosis, which can secondarily cause thrombosis. The origin of these stenoses is intimal hyperplasia of the vessel and is apparently multifactorial (flow turbulence and devascularisation of the vessel walls).8 These lesions can be treated radiologically or surgically, and each hospital must develop the appropriate protocol based on their available resources and pertinent experience in an attempt to meet the standards established by international guidelines (primary patency >50% after 6 months for radiological treatments, and after 1 year for surgical treatments).
Since our hospital has a greater level of experience and availability of resources for the treatment of these stenoses in the surgery department, this is the approach taken in our treatment protocol. The aim of this study was to examine the patency results for this type of repair (PROX RC), as well as its impact on initial vascular access patency (RC AVF).
METHOD
Hospital: Our study was carried out at a tertiary hospital in the region of Madrid, which serves a population of approximately 550 000 inhabitants. In addition to its assigned health area, this hospital is a reference centre for haemodialysis vascular accesses for a population of 250 000 inhabitants in the region of Castilla y Leon.
Patients: We reviewed the cases of all patients with juxta-anastomotic stenoses in RC AVF that were treated at the Hospital Universitario Fundación Alcorcón between 1998 and 2009. We only included those cases that developed this type of dysfunction.
We collected all data regarding the procedure in a specific vascular access protocol from the clinical histories held in a database at our hospital.
Surgical technique: In all patients, a new latero-lateral proximal anastomosis was created (PROX RC) using local anaesthesia (mepivacaine at 1%). The thrombosis of the fistula was treated in an emergency context (within the first 24 hours of occurrence) using the same surgical technique (PROX RC). The associated thrombus was removed when needed.
Follow-up: We monitored each patient until either the death of the patient or the end of the vascular access. A diagnosis of dysfunction was confirmed using fistulography in all cases, whereas the diagnosis of thrombosis was strictly clinical. The only requirement for making this diagnosis was a physical examination of the affected access site by an expert nephrologist or surgeon. The cephalic vein was well-developed and percussible along its entire length, with pulse absent or present only in the peri-anastomotic area. An examination of pulse in the cephalic vein up to an area proximal to the forearm suggested a proximal stenosis as the cause of the thrombosis.
Definitions
- Initial RC AVF: Radiocephalic fistula. This was the initial surgical technique.
- PROX RC: Proximal radiocephalic fistula. This was the repair method of choice for juxta-anastomotic stenoses of the initial RC AVF.
- Vascular access dysfunction: RC AVF with haemodynamically significant stenosis. In the case of RC AVF, this involves low flow rates, difficult puncture, vein collapse, and negative blood pressure. Any of these symptoms was cause for a diagnostic fistulography.
- Functionally significant stenosis: A reduction in vessel diameter >50% associated with haemodynamic or clinical abnormalities.
- Juxta-anastomotic stenosis: Stenosis affecting the anastomosis, or the radial artery and cephalic vein in the region of the anastomosis, and/or a combination of them, not affecting the puncture areas.
- Primary patency: Time interval between the primary procedure and any subsequent intervention performed to maintain patency. In our study, this was measured for both the initial RC AVF and for the new PROX RC, and was the primary objective of the study.
- Secondary patency: Time interval between the initial procedure and abandonment of the vascular access for any cause, including manipulation and intervention for maintaining patency. This was also measured for both initial RC AVF and PROX RC AVF.
Statistical analysis: For the analysis of probability of patency (primary and secondary) we used SPSS statistical software to calculate Kaplan-Meier curves
RESULTS
During the study period, a total of 858 patients underwent dialysis using 1414 vascular accesses (including catheters), 465 of which (33%) were autogenous arteriovenous fistulas (AVF), and 297 of these (64%) were radiocephalic. Of the 297 RC AVF, 165 had some type of dysfunction (55.55%). Of these initial RC AVF, 96 (58.8%) developed dysfunction due to a juxta-anastomotic stenosis, requiring a PROX RC.
Most stenoses appeared during the first 2 years following AVF creation (38% in the first year and 26% in the second one). Only 9.6% of stenoses appeared after the 5th year of follow-up.
The mean patient age was 67 years and the majority of patients (68.7%) were male.
The mean patient follow-up time was 57.27 months (95% confidence interval: 47.53-67.02).
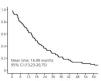
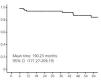
Primary patency after 1, 2, 3, 4, and 5 years with the initial RC AVF requiring repair due to dysfunction or thrombosis secondary to a juxta-anastomotic stenosis was 62.7%, 36.1%, 21.7%, 13.3%, and 9.6%, respectively (Figure 1).
The RC PROX AVF were scheduled due to low flow in 70.5% of cases, and the other 29.5% of procedures were performed on an emergency basis for thromboses. The initial patency of the procedure was 100%. Repairs were made in an ambulatory basis in 92% of cases.
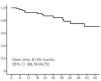
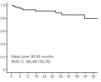
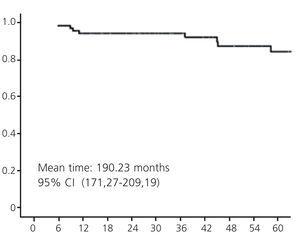
Primary patency after 1, 2, 3, 4, and 5 years for the PROX RC was 89.4%, 75%, 70.4%, 65%, and 56%, respectively (Figure 2). Fourteen patients required a total of 16 new surgical procedures during the study period (12 new proximal anastomoses and 4 cases of prosthetic graft placement) in order to maintain fistula patency (0.035 procedures per at-risk vascular access and follow-up year). Taking into account these repair interventions, the secondary patency of PROX RC after 1, 2, 3, 4, and 5 years was 93.7%, 92.1%, 89.6%, 87%, and 82.6%, respectively (Figure 3).
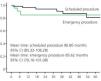
The patency of the PROX RC was higher if repairs were scheduled, reaching 96.5%, 94.5%, 91.5%, 88.4%, and 83.5% after 1, 2, 3, 4, and 5 years, respectively, versus 91.5% after 6 months and 84.7% after one year in the case of emergency procedures. However, the difference between scheduled and emergency repair surgery in terms of long-term patency was not significant (Figure 4).
During the follow-up, 37 patients died with a patent AVF.
Secondary patency (including repairs) after 1, 2, 3, 4, and 5 years of initial RC AVF was 95%, 93.2%, 93.2%, 89.1%, and 86.6%, respectively (Figure 5).
DISCUSSION
The most common cause of RC AVF dysfunction is juxta-anastomotic stenoses.8,9 The treatment of theses stenoses remains a topic of debate because of the variety of options available. According to the international clinical guidelines, each centre must develop a treatment protocol based on resource availability and staff experience. The results of these protocols must be monitored and adjusted in order to reach the outcomes recommended by international guidelines (primary patency >50% after 6 months for radiological treatment, and after 1 year for surgical treatment).6
In our experience, the majority of stenoses appeared during the first 2 years following creation of the AVF, and very rarely after the 5th year (9.6% in our cohort). Our results (38% in the first year and 26% in the second one) are similar to those observed in other studies.10,11
The use of interventional techniques for this situation was first described in 1989 by Gmelin12 and involves dilating the stenosed area with different types of balloons (standard, high pressure, or cutting balloon). In general, radiological treatment has worse results in terms of primary patency, as we “work” on the affected vessel and a higher number of procedures is necessary in order to reach similar secondary patency results to those obtained through surgery.10-16
The use of stents in this type of stenosis is more debatable because this may affect the area surrounding puncture sites and the results from this treatment are not clearly superior to those of angioplasty alone.16
Much less has been published on the surgical treatment of these stenoses. However, the most commonly standardised treatment is a proximal re-anastomosis using the healthy vessels located closest to the stenosis, which preserves the puncture area. The available literature involves mainly short studies including mixed vascular access types.17-19
The studies by Tessitore20 and Napoli21 are of enormous interest, since they compared the two approaches. In the article by Tessitore, the rate of restenosis was 0.168 events/fistula/year for surgery, and 0.519 events/fistula/year for angioplasty (P=.009). In the Napoli study, a greater primary patency was obtained using the surgical technique, with no differences in terms of assisted primary patency. Both studies concluded that any approach is reasonable, with similar assisted patency rates for both approaches, and that the two treatments can be complementary, although the radiological treatment does involve a higher number of re-interventions.
In our experience, following a PROX RC, the rate of re-interventions was very low (0.035 procedures per at-risk access and year of follow-up). In the majority of cases, a new proximal anastomosis was possible, and in two cases an arterial prosthesis was placed in order to carry out the repair.
Our hospital is a reference centre for creating and maintaining vascular accesses for several health areas in the regions of Madrid and Castilla y Leon. We work as a multidisciplinary team including members from the nursing staff and the nephrology, radiology, and surgery departments. However, the availability of continued care depends on the surgery department and our hospital has a greater level of experience dealing with emergency complications of vascular accesses.22-24 We consider radiological treatment as a first choice for those cases of stenoses proximal to the autogenous fistula and stenosis of prosthetic fistulas.
The difficult access to this technique in many centres is often due to the scarcity of resources in surgical departments to repair or create AVFs, as was shown in the article published by the Madrid Society of Nephrology (Sociedad Madrileña de Nefrologia; SOMANE) in 2010.25
In our experience, the treatment of juxta-anastomotic stenoses in radiocephalic AVF using a new proximal anastomosis is a good treatment option since it provides:
- Very high rates of initial patency, avoiding the use of catheters.
- Primary patency rates superior to those recommended by international guidelines (89% vs 50%), even in emergency surgery.
- A low rate of maintenance procedures (0.035 procedures/patient/year).
We believe that the key to these positive results lies in properly establishing indications for the procedure and a new anastomosis in healthy, well-developed vascular sections (which is more complicated in emergency surgeries), after ruling out other proximal causes of dysfunction.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Figure 1. Primary patency of the initial radiocephalic arteriovenous fistula
Figure 2. Primary patency of the proximal radiocephalic arteriovenous fistula
Figure 3. Secondary patency of the proximal radiocephalic arteriovenous fistula
Figure 4. Secondary patency of the proximal radiocephalic arteriovenous fistula according to the type of surgery (emergency or scheduled)
Figure 5. Secondary patency of the initial radiocephalic arteriovenous fistula