Introducción: se analizan los resultados de la Superficialización (Spf) de venas autólogas para establecer sus posibilidades reales en nuestro medio. Métodos: la Spf se realizó en 48 pacientes. El tiempo medio de seguimiento fue de 18,8 (0,2-75,7) meses. Se calculó la tasa de fallo primario, la Supervivencia (SV) primaria y la SV secundaria, y se estudiaron las posibles asociaciones con distintas variables. Resultados: la tasa de maduración fue del 97,9%, y la tasa de fallo primario, del 2,0%. El tiempo medio de SV primaria tras la superficialización fue de 65,5 ± 4,8 meses, y el de SV secundaria, de 66,7 ± 4,3 meses. Ninguna de las variables preintervención estudiadas (edad, sexo, Diabetes Mellitus [DM], presencia de catéter ipsilateral, número de Acceso Vascular (AV) u obesidad) tuvieron un impacto sobre las mismas. Se detectaron cuatro trombosis. Conclusión: la Spf de venas autólogas puede ser un método alternativo aceptable a la colocación de una prótesis vascular o un catéter.
Introduction: We review our experience with autologous veins Superficialization (Spf), to establish the actual possibilities of this kind of vascular access in our area. Methods: Between January/2001 and January/2008, Spf was performed in 48 patients. Mean follow-up time was 18.8 (0.2-75.7) months. Primary failure rate was recorded; primary and secondary survival were estimated using the Kaplan–Meier method; and its possible associations with several variables were analyzed. Results: the maturity rate was 97.9%; and the rate of primary failure 2.0%. After Spf, mean time of primary and secondary survival were 65 months and 67 months, respectively. Four vascular thromboses were observed. None of the presurgery variables analyzed (age; sex; diabetes mellitus; ipsilateral central catheter; the number of previous VA attempts; and obesity) were significantly associated with maturity rate, primary or secondary survivals. Conclusion: the Spf can be a good option alternative to the use of prosthetic grafts or permanent central vascular catheters.
INTRODUCTION
The use of autologous veins seems to have a more favourable prognosis than prosthetic implants or permanent catheters , which is why initiatives promoting these have been introduced in the US, with renewed interest in superficialization and/or the transposition of autologous VAs.2-4 The purpose of the present study is to analyse the experience of Spf in this hospital, compared with data in the literature, and evaluate the real possibilities of this type of VA.
METHOD
Retrospective observational study. Spf of the Basilic Vein (BV) or Cephalic Vein (CV) was performed in 48 patients between January 2001 and January 2008.
Before considering inserting a Permanent Catheter (PC) or a vascular prosthesis, attempts were made to preserve or perform an autologous VA. Spf of the BV or CV was used as a back-up method and not as a primary alternative to surgery in all cases in which, despite the fact that the vein was permeable and adequately developed, the depth of the vein made it impossible and therefore punctures on a short section were necessary, which in the long run would lead to VA failure. Although this was more frequent in the case of the BV, it did occasionally occur in the CV.
The first option was a radiocephalic Arteriovenous Fistula (AVF) and if an AVF at the elbow was required, the surgical technique favoured was mid-humeral AVF, which allowed the development of both veins (BC and CV.) In cases where a brachiobasilic (BB) fistula was performed de novo, since there was no permeable CV, the intervention was carried out in two sessions to allow the vein to develop before Spf (suitable after 4mm.) The following was calculated: survival (SV) of the VA from its creation (counting the period following Spf), primary survival (SV1) of the Spf (from Spf until some type of intervention is performed aimed at maintaining or re-establishing permeability), secondary survival (SV2) of Spf (from Spf until its permanent abandon for any reason) and the maturity rate and primary failure rate. The following variables were recorded: age, gender, DM; period of HD when Spf was performed; Body Mass Index (BMI); number of previous VAs; PC inserted; as well as post-surgical complications (haematoma, oedema of the hand, infection) and interventions (angioplasty and the insertion of stents.) The failure of fistula was considered an event.
STATISTICAL ANALYSIS
The Kaplan-Meier method was used to calculate SV1 and SV2. The chi-square test was also used to evaluate the association between the different variables and the existence of thrombosis. The influence of the different variables on the access SV was analysed using the logrank test. P < 0.05 was considered statistically significant.
RESULTS
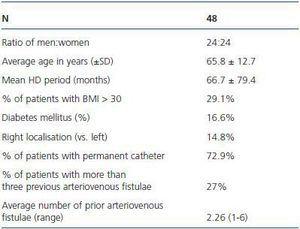
Spf was performed in 48 patients (43 BV and 5 CV). The population characteristics are shown in table 1. During the study, nine patients died, three received a transplant and one was transferred to another centre. All had functioning fistulae. The follow-up period was 18.8 months (0.2-75.7.) The indication of Spf was: Spf of the CV due to obesity preventing the vein from being located in 5 patients; Spf of the BV due to complete or partial thrombo-thrombosis of the CV which was used as return in 17 patients; and Spf of the BV due to a BB fistula since there was no permeable CV in 26 patients. Spf was only performed on the first VA in 22.9% of the patients. In 44 patients, Spf was performed once HD had started (mean: 66.1 months [2.75-115.1].) In four patients this was performed before inclusion in HD: due to development of the BV only in two cases and due to obesity in the other two, which meant that Spf of the CV was required to puncture the vein.
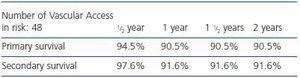
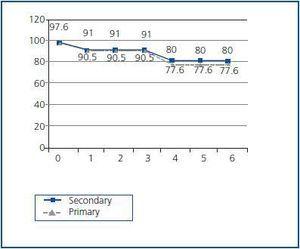
The survival of the VA from its creation, counting the period following Spf, was 155.4 ± 13.3 months. SV1 following Spf was 65.5 ± 4.8 and SV2 was 66.7 ± 4.3 months (table 2, figure 1.) The rate of maturity was 97.9% and the primary failure was 2.0%.
The mean time elapsed from the VA to Spf was 4.52 months (P25-P75: 1.85-13.76). Spf was performed at the same time as the fistula in only one patient. The mean time elapsed between Spf and the puncture was 32.3 ± 27.9 days.
Complications in the immediate post-operative period included four haematomas. No infectious episodes were recorded. In the medium term, oedema of the hand developed in eight patients (16.6%) and stenosis was detected in six of these (five angioplasties and the insertion of a stent.) There was once case of AVF thrombosis following an attempt at revascularization. Four events were detected (loss of functioning VA): one primary failure during Spf (the only case in which Spf was performed at the same time as the creation of the VA), three delayed thrombosis complications (5.8, 10.2 and 12.3 months following Spf) and one AVF closure due to steal syndrome and ischaemia of the hand 34.7 months after Spf.
None of the variables studied (age, gender, DM, CP, number of previous VAs or obesity [BMI > 30]) were associated with a greater risk of thrombosis, except the presence of oedema of the hand (RR 10.4; CI 95% 1.9-263; p < 0.01), or had a significant impact on the rate of maturity or SV1 and 2.
DISCUSSION
The present study shows the experience of this hospital in the Spf of autologous VA. Although this is a retrospective observational study, with no control group for comparisons, it serves as a reminder, although not a significantly extensive one, of a surgical technique, which could encourage the performance of autologous VA rather than the insertion of prostheses and PCs.5
The advantage of this alternative is based on data from the literature, which show a 41% increase in the risk of primary failure and 91% more revisions of prostheses than fistulae, with greater possibility of thrombosis and infection, as well as greater mortality and morbidity associated to the use of catheters.6,7 Several recent studies8,9 have demonstrated improved SV in Spf of the BV compared with prostheses and a fewer number of interventions and complications. This study does not allow for this type of comparison, given the low proportion of prostheses (0.6-1.6%), since this was the first option from the beginning. However, it does provide useful data on the survival of this type of VA, which are similar10,11 or even better12 than other data published.
Most of the patients had PCs inserted with multiple failed fistulae and had been ruled out for autologous VA by other surgeons. This technique facilitated the removal of the PC and preservation of an autologous VA. In a lower percentage, performing this technique in the early stages prevented the use of PCs and extended the life of the AVF,13 since the BV could be used despite thrombosis of the CV. The problem of using the BV is that is becomes deep very quickly, leaving only a small area accessible for the puncture, therefore requiring repeated punctures in a short section with the danger of recirculation and repeated damage to the neointima. Spf facilitates an extension of the puncture area thus avoiding both problems and provides an “autologous” solution to CV failure.
One of the disadvantages of Spf is the greater risk of the Spf of the BV failing to mature in comparison with prostheses,14 given that fibrosis of the scar could prevent adequate dilatation of the vein. In our experience, Spf performed in two sessions, once the vein undergoing superficialization is thick enough, facilitates good results in terms of maturity, up to 97%. Another problem related to this technique is the time required for vascularisation, which is greater than in cases of prostheses or PCs. However, it does allow autologous VA with good survival rates.
Complications were similar to those described in any other type of vascular surgery and no infections were detected.
None of the factors studied had a significant impact on the maturity rate or survival in the long term, with the exception of oedema of the hand. This was probably due to the fact that it showed the existence of underlying stenosis and the need for revision and subsequent action. In comparison with fistulae, SV2 for Spf is similar, however it has been shown that it requires more revisions.15 In this study, 12.5% required a subsequent revision via fistulography with the detection of stenosis, requiring an angioplasty in five patients and the insertion of a stent.
In conclusion, in our experience, the survival of this type of VA was good, with a low rate of complications and better survival than that described in other studies. It may therefore be considered as an alternative to the insertion of a vascular prosthesis or catheter in those patients that have a VA that may be punctured.
Table 1. Clinical characteristics of the patients
Table 2. Primary and secondary survival of 48 basilic superficializations
Figure 1.