Increased aortic or central arterial stiffness (CAS) is a major factor in cardiovascular morbidity and mortality in patients with vascular risk factors. Decreased glomerular filtration rate (GFR) and increased urinary albumin excretion (uALB) are associated with lethal and non-lethal cardiovas-cular events. The pathophysiological mechanisms of this association are not fully defined. The aim of this study was: 1.- To analyse the CAS, comparing several markers, in subjects with arterial hypertension (HTN), diabetes mellitus (DM), chronic kidney disease (CKD) and their combination. 2.- To study the possible association of CAS with renal dysfunction (decrease in GFR and increase in uALB).
Material and methodsA total of 286 subjects were included, divided into several groups: Control (n:38); HTN (n:51); DM without CKD (n:26); CKD without DM (n:77); CKD with DM (n:94). Several indices obtained by applanation tonometry were used to determine the CAS: carotid-femoral pulse velocity (VPc–f); central pulse pressure (cPP); augmentation index standardised to a cardiac frequency of 75 L/min (IA75); peripheral/aortic arterial stiffness gradient (ASGp-a). As a marker of peripheral arterial resistance, the carotid-radial pulse velocity (PVc-r) was determined. The ASGp-a was calculated from the PVc-r/PVc–f ratio. The subendocardial viability index (iBuckberg) was obtained from the aortic pulse wave.
Multiple regression, binary logistic regression, and multinomial regression were used to study the association between arterial stiffness markers and renal function.
ResultsThe adjusted values of the PVc–f [(median (interquartile range) (m/s)] were significantly higher in subjects with DM [(9 (1.2)], CKD [(9.4 (0.7)] and DM with CKD [(10.9 (0.7)] than in the control group [(8.2 (1.3)] and group with HTN [(8.3 (0.9)], (p: 0.001). Patients with DM with CKD had higher PVc–f values than all other groups (p: 0.001). The ASGp-a of the patients was significantly lower than that of the controls, and the group with DM with CKD had significantly lower values than the other groups. The cPP in the DM with CKD group was significantly higher than in the other groups. All patients had an AI75 higher than the control group.
When all aortic stiffness markers were introduced together in the regression, PV c–f was the only one that, after multivariate adjustment, was independently and inversely associated with GFR (β; −4, p: 0.001) and predicted the presence of GFR decrease (<60 mL/min/1.73 m2), [(OR (95%CI): 1.50 (1.17−1.92; p: 0.001]. The PVc–f was the only index directly associated with albuminuria (β: 0.15, p: 0.02) and predicted the existence of abnormal albuminuria (>30 mg/g), [(OR; 1.66 (1.25−2.20), p: 0.001)]. The PVc–f was also associated with the iBuckberg (β: −2.73, p: 0.01).
Multinomial regression confirmed that PVc–f is a significant determinant of GFR and uALB. On the other hand, the increase in PVc–f and the presence of DM contribute significantly to the magnitude of albuminuria.
ConclusionsAortic stiffness increases in the presence of vascular risk factors such as hypertension, DM and CKD. This increase is greater when DM and CKD coexist. Increased aortic stiffness is inversely associated with GFR and directly with uALB, and is predictive of decreased GFR and abnormal uALB. The VPc–f is the parameter of aortic stiffness that is most consistently associated with renal dysfunction. Increased aortic stiffness could be one of the pathomechanisms linking renal dysfunction to cardiovascular events.
El aumento de la rigidez arterial central (RAC) participa en la morbimortalidad cardiovascular de los enfermos con factores de riesgo vascular. El descenso del filtrado glomerular (FG) y el aumento de la excreción urinaria de albúmina (uALB) se relacionan con eventos cardio-vasculares. Los mecanismos fisiopatológicos de esta asociación no están completamente definidos.
El objetivo de este estudio fue analizar la RAC, comparando varios marca-dores, en sujetos con hipertensión arterial (HTA), diabetes mellitus (DM), enfermedad renal crónica (ERC) y su combinación, y estudiar la posible asociación de la RAC con la disfunción renal.
Material y métodosSe incluyeron 286 sujetos distribuidos en varios grupos: Control ; HTA ; DM sin ERC; ERC sin DM ; ERC con DM. Para la determinación de la RAC se usaron varios índices obtenidos por tonometría de aplanamiento: velocidad de pulso carótida-femoral (VP c-f ) y gradiente de rigidez arterial periférica/aórtica (GRAp-a),entre otros. De la onda del pulso aórtico se obtuvo el índice de viabilidad subendocárdica (íBuckberg).
Para el estudio de la asociación entre los marcadores de rigidez arterial y la función renal se usaron la regresión múltiple, la regresión logística binaria y la multinomial, todas con ajuste multivariante.
ResultadosLos valores ajustados de la VP c-f [(mediana (rango intercuartílico) (m/seg)] fueron significativamente mayores en los sujetos con DM [(9 (1,2)], ERC [(9,4 (0,7)] y DM + ERC [(10,9 (0,7)] que en el grupo control [(8,2 (1,3)] y grupo con HTA [(8,3 (0,9)], (p:0,001). Los enfermos con DM + ERC tenían valores de VP c-f superiores a todos los demás grupos (p:0,001). El GRAp-a de los enfermos fue significativamente inferior al de los controles, y el grupo con DM + ERC tenía valores significativamente inferiores al de los otros grupos.
La VP c-f era el único marcador de rigidez aórtica que se asociaba de forma independiente e inversa con la magnitud del FG (β; -4, p:0,001) y predecía la presencia de disminución del FG [( OR (95%IC): 1,50 (1,17−1,92; p:0,001]. La VP c-f era el único índice asociado de forma directa con la cuantía de la uALB ( β: 0,15, p:0,02) y predecía la existencia de una uALB anormal [(OR;1,66(1,25−2,20),p:0,001)]. La VP c-f también se asociaba con el iBuckberg ( β: -2,73, p:0,01).
En la regresión multinomial se confirmó que la VP c-f es un determinante significa-tivo del FG y de la uALB. Por otra parte, el aumento de la VP c-f y la presencia de DM contribuían de forma significativa a la magnitud de la uALB.
ConclusionesLa rigidez aórtica aumenta en presencia de factores de riesgo vascular y es mayor cuando coexisten DM y ERC. El aumento de la rigidez aórtica se asocia de forma inversa con el FG y directamente con la magnitud de la albuminuria, y tiene capacidad predictiva de una disminución del FG y de una albuminuria anormal. La VP c-f es el parámetro de rigidez aórtica que se asocia de forma más consistente con la disfunción renal. El aumento de la rigidez aórtica podría ser uno de los patomecanismos que vinculan la disfunción renal con los eventos cardiovasculares.
In arterial hypertension (HTN), diabetes mellitus (DM) and chronic kidney disease (CKD), there is an increase in aortic stiffness that is involved in the pathogenesis of target organ lesions and cardiovascular morbidity and mortality.1,2 Multiple factors (including haemodynamic, metabolic, inflammatory, endothelial dysfunction and vascular calcification) are involved in increased aortic stiffness.3–5 In these situations, early vascular ageing (EVA) occurs, characterised by the loss of elasticity of the vascular wall and an increase in arterial stiffness.
Preserving vascular elasticity is crucial, since the distension and recovery of the calibre of the arteries in systole and diastole, respectively, acts as a buffer for blood flow, allowing continuous perfusion of the target organs. In young individuals, vascular wall elasticity decreases sequentially from the aorta to the peripheral muscular arteries. Physiologically, there is a gradient between peripheral and aortic stiffness (peripheral-aortic arterial stiffness gradient [paASG]). This gradient facilitates a delayed reflex wave returning to the ascending aorta during diastole, which maintains diastolic blood pressure and mitigates pulsatile pressure in microcirculation.
With vascular senescence, the elasticity of the vascular wall decreases and aortic stiffness increases. Increased aortic stiffness promotes an accelerated return of the reflex wave during systole, which leads to an increase in central systolic blood pressure (cSBP) and central pulse pressure (cPP). Furthermore, attenuation or reversal of the paASG may occur, facilitating the conversion from physiological continuous blood flow in the microcirculation to pulsatile flow. Pulsatile flow in microcirculation induces damage in low-resistance organs such as the kidney and brain.4
There is a close relationship between aortic stiffness and carotid-femoral pulse wave velocity (cfPWV), considered the gold standard for determining aortic stiffness. Carotid-radial pulse wave velocity (crPWV) reflects the stiffness of the muscular arteries (peripheral stiffness) and the crPWV ratio/cfPWV has been used as an index of the paASG.6 Other parameters derived from the morphology of the central pulse wave, such as cPP and augmentation index (AI), which expresses which part of the cPP corresponds to the reflex wave, have been proposed as surrogate markers of aortic stiffness.7
There are studies that have evaluated, in isolation in subjects with HTN, DM or CKD, the association of some of the arterial stiffness parameters with renal function.8–11 The results of the association between aortic stiffness and glomerular filtration rate (GFR) are not consistent. While some studies show a significant association,9,10 in others the relationship between aortic stiffness and GFR disappears after multivariate adjustment.11 The mechanism by which increased aortic stiffness causes renal dysfunction is not fully understood.
To the best of our knowledge, there are no studies that jointly analyse and use the different markers of aortic arterial stiffness and the possible association between aortic stiffness and renal function in subjects with different vascular risk factors (HTN, DM, CKD and their association). Since the various central arterial stiffness (CAS) indices are influenced by different but haemodynamically related variables,7,12 the analysis of their possible association with renal function could help clarify the pathophysiological mechanisms of this relationship.
Our objective was twofold: on the one hand, to describe the behaviour of CAS in subjects with different vascular risk factors; and, on the other hand, to analyse the impact of aortic stiffness on renal function assessed by GFR and albuminuria.
MethodsSubjectsIn total, 286 subjects were evaluated and reviewed in the nephrology outpatient clinic of a university hospital. Subjects previously diagnosed with HTN, DM, CKD or a combination of them were included. To be included in the study, subjects must not have had any cardiovascular events in the previous six months, kidney function must have been stable in the previous three months and there must have been no changes in antidiabetic, antihypertensive or lipid-lowering therapy during this time. Subjects with immunological diseases requiring immunosuppressive therapy, those diagnosed with malignancies, HTN of endocrine origin or aortic aneurysm, and those with atrial fibrillation that made it difficult to capture the pulse wave by tonometry were excluded.
Data on cardiovascular disease (CVD) requiring hospital admission and peripheral arteriopathy diagnosed by symptoms and/or an ankle-brachial index less than 0.9 were collected from the medical records. Smoking habits were investigated, considering both active smokers and those who had stopped smoking to be smokers, as opposed to those who had never smoked (non-smokers).
Haematological and biochemical parameters were measured in blood, including complete blood count, creatinine, lipids, uric acid, blood glucose, glycated haemoglobin (in DM), calcium-phosphorus metabolism with parathyroid hormone (PTH), and vitamin D (in CKD). Estimated glomerular filtration rate (eGFR) was calculated using the chronic kidney disease, epidemiology (CKD-EPI) formula. In all subjects, the albumin-creatinine ratio was determined in the first morning urine.
In total, 38 healthy, non-smoking subjects with no history of CVD or other diseases and normal renal function were used as controls for arterial function parameters. In these subjects only renal function lab test parameters were determined.
CKD was defined as a urine albumin/creatinine ratio greater than 30 mg/g and/or eGFR less than 60 mL/min/1.73 m2. Since there may be a higher risk of cardiovascular morbidity and mortality in subjects with albuminuria values in the normal range, a subgroup of albuminuria (normal-high) was added and categorised as follows: normal 0−10 mg/g; high-normal: 11−29 mg/g; moderate increase: 30−299 mg/g; major increase: more than 300 mg/g. The subjects were distributed into five groups: control, HTN, DM, CKD and CKD plus DM.
All subjects gave informed consent and the study met all ethical requirements of the study site.
Study of aortic and peripheral arterial stiffnessAfter resting for 15 min, the average of three brachial blood pressure (BrBP) measurements was taken, using an Omron M3 oscillometric device (Omron electrónica Iberia, S.A.U., Madrid). Central blood pressure (cBP) and cfPWV were studied by applanation tonometry using a SphygmoCor device (AtCor Medical, Sydney, Australia). The central aortic pressure wave and its different components (the cSBP, the central diastolic blood pressure [cDBP] and central pulse pressure [cPP]) were obtained from the pulse wave obtained by tonometry on the radial artery and using a generalised transfer function. In the generated aortic pressure wave, the junction point of the anterograde incident wave and the reflected wave (inflection point) was identified. Augmentation pressure (AP) was the maximum cSBP minus the pressure at the inflection point. The AI was defined as the AP divided by the cPP and is expressed as a percentage. Given the influence of heart rate (HR) on the AI, the SphygmoCor device standardises the AI to a HR of 75 L/min (AI75). To determine the carotid-femoral pulse wave velocity (representative of aortic or central stiffness), the pulse wave was obtained sequentially over the common carotid artery and the femoral artery, calculating the travel time between the two points from the difference between the R wave of the simultaneous electrocardiographic recording and the start of the pulse wave at the respective arterial sites. The crPWV, which is representative of peripheral arterial stiffness, was determined using the same technique, but on the radial artery. The paASG was calculated from the crPWV/cfPWV ratio.
The subendocardial viability ratio or Buckberg index was also derived from the aortic pulse wave, which results from the diastolic pressure-time integral/systolic pressure-time integral, and which represents a resting measure of myocardial oxygen supply and consumption.13 In 44% of subjects with CKD and in 42% of the group with CKD + DM, the degree of abdominal aorta calcification was studied by lateral X-ray of the lumbar spine, determining the Kauppila index.14
Statistical analysisQualitative variables are expressed as relative frequencies. Continuous variables are expressed as mean ± standard deviation (x ± SD) when the distribution was normal, and as median (interquartile range [IQR]) for non-normal distribution. Some of the variables with a highly skewed distribution, such as the urine albumin/creatinine ratio, were converted to their natural logarithms. The Shapiro-Wilk and Kolmogorov-Smirnov tests were used to establish the normality of the distribution of the variables, depending on the sample size.
Qualitative variables between groups were compared using the χ2 test, while quantitative variables were compared using one-way analysis of variance (ANOVA) with adjustment for covariates (ANCOVA) that could affect the results. Two-way ANOVA was used to analyse the possible effect of two qualitative variables and their possible interaction on the dependent variable of interest. To maximise possible differences in kidney function between groups, and when the requirement of equality of covariance matrices was met, multivariate analysis of variance (MANOVA) was used, introducing eGFR and albuminuria as dependent variables.
The relationship between variables was studied using the Pearson or Spearman correlation coefficient, depending on their distribution. The independent relationship between variables was investigated using multiple linear regression by selecting potential covariates that demonstrated significant correlation. Binary logistic regression was used to assess the independent effects and predictive value of arterial stiffness parameters on kidney function (eGFR and albuminuria). For greater precision in the predictive capacity of arterial stiffness markers on kidney function and their possible interaction with DM, multinomial logistic regression was used employing four possible classes of kidney function as categorical dependent variables: normal (normal albuminuria and eGFR); albuminuria (urine albumin/creatinine ratio greater than 30 mg/g); reduction in eGFR (eGFR less than 60 mL/min/1.73 m2); and reduced eGFR and albuminuria (eGFR less than 60 L/min/1.73 m2 and urine albumin/creatinine ratio greater than 30 mg/g), and the four categories of albuminuria (normal, high-normal, moderate and major). In these analyses, normal kidney function (eGFR ≥60 mL/min/1.73 m2 and albuminuria ≤30 mg/g) and normal albuminuria (≤10 mg/g), were used as reference categories, respectively.
In the statistical results, a p-value <0.05 was considered significant. All statistical analyses were performed using the IBM SPSS (Statistical Package for the Social Sciences) statistical program, version 25 for Windows.
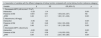
ResultsIn total, 286 subjects were studied, who were distributed into five groups: 1) control group, 2) patients with essential hypertension without CKD, 3) patients with DM without CKD, 4) patients with CKD without DM, and 5) patients with CKD plus DM. Table 1 shows the clinical characteristics and laboratory data of the groups. There were significant differences between the groups in terms of age, body mass index (BMI), percentage of females, history of CVD and therapy with renin-angiotensin system (RAS) inhibitors and statins. The duration of DM, the presence of retinopathy, and insulin therapy were longer and more frequent in subjects who had CKD in addition to DM. The underlying nephropathy in the CKD group was nephroangiosclerosis: 58.4%; chronic glomerulonephritis (CGN): 24.7%; other (polycystic kidney disease, chronic pyelonephritis, undetermined): 16.9%. In the group with CKD + DM, the following nephropathies were recorded: nephroangiosclerosis: 42.6%; diabetic nephropathy (DN): 56.4%; and CGN:1%.
Clinical and laboratory data.
| Group | ||||||
|---|---|---|---|---|---|---|
| no. | Control | HTN | DM | CKD | CKD + DM | p |
| 1 | 2 | 3 | 4 | 5 | ||
| 38 | 51 | 26 | 77 | 94 | ||
| Clinical data | ||||||
| Age (years) | 42 (15) | 56 (12) | 55 (15) | 64 (19) | 66 (11) | 1 vs 2,3,4,5:0.001 |
| 2 vs 4.5:0.03 | ||||||
| 3 vs 5:0.01 | ||||||
| BMI (kg/m2) | 26 (5) | 31 (6) | 31 (7) | 29 (4) | 31 (6) | 1 vs 2,3,4,5:0.001 |
| 3 vs 4:0.03 | ||||||
| Females (%) | 39 | 20 | 38 | 40 | 28 | 2 vs 1,3,4,5:0.04 |
| Duration of DM (years) | N/A | N/A | 2 (4) | N/A | 13 (12) | 3 vs 5:0.001 |
| Smoking (%) | 0 | 47 | 46 | 34 | 47 | NS between 2,3,4,5 |
| History of CVD (%) | 0 | 12 | 35 | 26 | 43 | 2 vs 3,4,5:0.03 |
| Diabetic retinopathy (%) | N/A | N/A | 8 | N/A | 30 | 3 vs 5:0.001 |
| RAS inhibition (%) | 0 | 80 | 78 | 92 | 93 | 2.3 vs 4,5:0.04 |
| Statins (%) | 0 | 25 | 48 | 48 | 71 | 5 vs 2,3,4: 0.001 |
| Vit D therapy (%) | 0 | 0 | 03 | 10 | ||
| Kauppila index | ND | ND | ND | 2 (10) | 8 (7) | 4 vs 5:0.008 |
| Laboratory data | ||||||
| eGFR (ml/min/1.73 m2) | 95 (18) | 95 (21) | 95 (23) | 32 (26) | 38 (25) | 1,2,3 vs 4,5:0.001 |
| 4 vs 5:0.07 | ||||||
| Alb./creat. log. | 1.1 (0.7) | 1.9 (0.8) | 2.3 (1.1) | 4.3 (2.7) | 4.9 (2.6) | 1 vs 3:0.01 |
| 1,2,3 vs 4,5:0.001 | ||||||
| 4 vs. 5:0.1 | ||||||
| Triglycerides (mg/dL) | ND | 139 (97) | 150 (116) | 143 (100) | 163 (93) | NS |
| LDL-C (mg/dL) | ND | 136 (59) | 105 (44) | 120 (56) | 107 (48) | NS |
| HDL-C (mg/dL) | ND | 50 (19) | 41 (16) | 47 (22) | 44 (12) | NS |
| Uric acid (mg/dL) | ND | 5.8 (3) | 5.1 (2) | 7 (2) | 7 (2) | 4.5 vs 3:0.01 |
| Calcium (mg/dL) | ND | ND | ND | 9.6 (0.6) | 9.5 (0.7) | NS |
| Phosphorus (mg/dL) | ND | ND | ND | 3.4 (1) | 3.6 (0.8) | NS |
| PTH (pg/mL) | ND | ND | ND | 127 (111) | 132 (95) | NS |
| 25(OH) vit. D (ng/mL) | ND | ND | ND | 24 (9) | 23 (9) | NS |
Data expressed as median (interquartile range) or percentage (%); Alb./creat. log.: albumin/creatinine ratio logarithm; BMI: body mass index; CKD: chronic kidney disease; CVD: cardiovascular disease; DM: diabetes mellitus; eGFR: estimated glomerular filtration rate; HTN: arterial hypertension; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; N/A: not applicable; ND: not determined; NS: not significant; PTH: parathormone; RAS: renin-angiotensin system.
The eGFR was significantly lower and albuminuria higher in the CKD groups (Table 1). Although the ANOVA revealed quantitative but not statistically significant differences in eGFR and albuminuria between the groups with CKD and CKD + DM, the multivariate analysis of variance showed significant differences in the eGFR and the albumin/creatinine ratio logarithm (alb./creat. log.) ([CKD: eGFR: 39{2}; CKD + DM: eGFR: 48{3} ml/min/1.73 m2, p = 0.015]; [CKD: alb./creat. log 4.43{0.2}; CKD + DM: alb./creat. log 5.05, p = 0.021]). When cfPWV and paASG were entered into the MANOVA as covariates, the difference in eGFR persisted (36 vs 50 mL/min/1.73 m2, p = 0.001), but disappeared in the alb./creat. log. (4.6 vs 4.9, p = 0.3).
The percentage and intensity of abdominal aortic calcifications were significantly higher in the group with CKD + DM compared to the group with CKD (87% vs 65%, p = 0.02 and Kauppila index 8 [7] vs 2 [10], p = 0.008), respectively.
The percentage of subjects with stage 1 CKD + 2 and 3a + 3b was higher in subjects with CKD + DM than in those without DM (24.5% and 58.1% vs 14.3% and 41.6%, respectively, p = 0.04), while in the group with CKD without DM, the percentage with stage 4 CKD was higher (41.6% vs 25.8%, p = 0.04). There were no significant differences in the percentage of subjects with stage 5 CKD (1% vs 2.6%).
Table 2 shows the values of BrBP and cPP, and the parameters of arterial stiffness and the subendocardial viability ratio after multivariate adjustment. Pulsatility marker values were significantly higher in the group with CKD and DM. The CKD groups with and without DM had higher cfPWV values. paASG values were significantly lower in the CKD and DM groups. The Buckberg index of patients with CKD + DM was significantly lower than that of the other groups.
Haemodynamic and arterial stiffness parameters.
| Group | ||||||
|---|---|---|---|---|---|---|
| no. | Control | HTN | DM | CKD | CKD + DM | p |
| 1 | 2 | 3 | 4 | 5 | ||
| 38 | 51 | 27 | 77 | 93 | ||
| Variable | ||||||
| Adjusted for age, sex | ||||||
| bSBP (mmHg) | 127 (15) | 142 (9) | 137 (11) | 140 (9) | 149 (9) | 1 vs 2,4,5: 0.006;1 vs 3:0.03 |
| 3 vs 5:0.001; 4 vs 5:0.002 | ||||||
| bDBP (mmHg) | 69 (9) | 80 (5) | 75 (8) | 79 (5) | 77 (4) | 1 vs 2,4,5:0.001; 1 vs. 3:0.02 |
| bPP (mmHg) | 56 (13) | 62 (10) | 62 (13) | 61 (7) | 71 (7) | 5 vs 1,2,3,4: 0.005 |
| AI75 (%)a | 17 (8) | 27 (5) | 27 (7) | 25 (4) | 25 (11) | 1 vs 2,3,4,5:0.004 |
| Buckberg index (%) | 157 (22) | 151 (18) | 149 (23) | 149 (14) | 134 (13) | 5 vs 1,2,4: 0.001; 5 vs 3:0.02 |
| Adjusted for age, sex, height and HR | ||||||
| cSBP (mmHg) | 111 (43) | 131 (51) | 128 (42) | 130 (25) | 145 (23) | 1 vs 5:0.01 |
| cPP (mmHg) | 43 (11) | 50 (8) | 50 (11) | 49 (6) | 58 (7) | 5 vs 1,2,4:0.007; 2 vs 1:0.04 |
| Values adjusted for age, sex, MAP, height, BMI and HR | ||||||
| cfPWV (m/s) | 8.2 (1.3) | 8.3 (0.9) | 9.0 (1.2) | 9.4 (0.7) | 10.9 (0.7) | 4 vs 1.2: 0.001 |
| 5 vs 1,2,3,4: 0.001 | ||||||
| 3 vs 1,2:0.07 | ||||||
| crPWV (m/s) | 7.6 (1.0) | 7.8 (0.8) | 8.0 (1.0) | 8.3 (0.6) | 8.4 (0.6) | NS |
| paASG | 1.04 (0.1) | 0.99 (0.1) | 0.89 (0.1) | 0.92 (0.1) | 0.81 (0.1) | 1 vs 3,4,5: 0.005; 2 vs 3,4:0.02;2 vs 5:0.001 |
| 5 vs 3:0.04;5 vs 4:0.001 | ||||||
AI75: heart rate augmentation index of 75 L/min; BMI: body mass index; bPP: brachial pulse pressure; bSBP: brachial systolic blood pressure; cfPWV: carotid-femoral pulse wave velocity; CKD: chronic kidney disease; cPP: central pulse pressure; crPWV: carotid-radial pulse wave velocity; cSBP: central systolic blood pressure; DM: diabetes mellitus; HR: heart rate; HTN: arterial hypertension; MAP: mean arterial pressure; NS: not significant; paASG: peripheral-aortic arterial stiffness gradient.
The age-adjusted and mean arterial pressure (MAP)-adjusted cfPWV of the subjects without nephropathy (8.47 ± 0.2) was significantly lower than that of those diagnosed with nephroangiosclerosis (9.73 ± 0.2), CGN (9.65 ± 0.3) (p = 0.003) and DN (11.30 ± 0.2) (p = 0.001). The cfPWV of the latter was significantly higher than that of subjects with nephroangiosclerosis and CGN (p = 0.001).
Considering all subjects, a significant direct correlation was observed between cfPWV and age, a correlation that was inverse for paASG (Fig. 1). A direct and significant correlation was found between eGFR and paASG and Buckberg index, and a significant and inverse correlation between eGFR and cfPWV, AI75 and cPP (Table 3 and Fig. 2). The correlation between these parameters and albuminuria was also significant, but in the opposite direction (Table 3 and Fig. 2). The prevalence of abnormal albuminuria and a fall in eGFR progressively increased with the higher quartiles of cfPWV (Fig. 3).
Correlation between arterial stiffness parameters, renal function and subendocardial viability index (Buckberg index).
| Age | eGFR | Alb./creat. log. | ||
|---|---|---|---|---|
| cfPWV | r | 0.648 | –0.502 | 0.301 |
| p | 0.001 | 0.001 | 0.005 | |
| paASG | r | –0.625 | 0.419 | –0.451 |
| p | 0.001 | 0.001 | 0.001 | |
| AI75 | r | 0.406 | –0.261 | 0.239 |
| p | 0.001 | 0.001 | 0.001 | |
| cPP | r | 0.452 | –0.265 | 0.282 |
| p | 0.001 | 0.001 | 0.001 | |
| Buckberg index | r | –0.241 | 0.261 | –0.204 |
| 0.001 | 0.001 | 0.001 | ||
| cfPWV | paASG | cPP | AI75 | Buckberg index | ||
|---|---|---|---|---|---|---|
| cfPWV | r | 1 | −0.753 | 0.536 | 0.315 | –0.319 |
| p | 0.001 | 0.001 | 0.001 | 0.001 | ||
| paASG | r | −0.753 | 1 | –0.434 | –0.284 | 0.302 |
| p | 0.001 | 0.001 | 0.003 | 0.001 | ||
| cPP | r | 0.452 | –0.434 | 1 | 0.328 | –0.281 |
| p | 0.001 | 0.001 | 0.001 | 0.001 | ||
| AI75 | r | 0.315 | –0.284 | 0.328 | 1 | –0.265 |
| p | 0.001 | 0.003 | 0.001 | 0.001 | ||
| Buckberg index | r | –0.319 | 0.302 | –0.281 | –0.265 | 1 |
| p | 0.001 | 0.001 | 0.001 | 0.001 | ||
AI75: heart rate augmentation index of 75 L/min; alb./creat. log.: albumin/creatinine ratio logarithm; cPP; central pulse pressure; cfPWV: carotid-femoral pulse wave velocity; eGFR: estimated glomerular filtration rate; paASG: peripheral-aortic arterial stiffness gradient.
Considering the subjects in whom PTH was measured, a direct and significant correlation was found between PTH and cPP (r = 0.232; p = 0.02).
An inverse correlation was observed between the Buckberg index, age and albuminuria and a direct correlation with eGFR. All aortic stiffness indices were significantly correlated with the Buckberg index. In the multiple regression, after multivariate adjustment, the only aortic stiffness marker independently and negatively associated with the magnitude of Buckberg index was cfPWV (β = −2.76; p = 0.014).
In the multiple regression analysis with multivariate adjustment for a history of CVD, smoking, presence of DM, MAP and urine alb./creat. log., the only aortic stiffness parameters independently and inversely associated with the eGFR value were cfPWV and AI75 (Table 4A). When arterial stiffness markers were individually introduced into the adjusted model, all were significantly associated, but cfPWV had the strongest relationship with eGFR (highest R2 and highest standardised β coefficient).
Multiple linear regression of arterial stiffness markers associated with eGFR value after multivariate adjustment.a
| Variable | F | R2 | β | SE | Std β | p |
|---|---|---|---|---|---|---|
| Constant | 27.12 | 0.47 | 77.33 | 16.32 | 0.001 | |
| cfPWV | –4.00 | 1.01 | –0.32 | 0.001 | ||
| AI75 | –0.38 | 0.13 | –0.14 | 0.006 | ||
| paASG | 4.58 | 8.92 | 0.03 | NS | ||
| cPP | –0.08 | 0.10 | –0.04 | NS |
Adjustment to mean arterial pressure, albumin/creatinine log, presence of DM, smoking, history of cardiovascular disease. AI75: augmentation index to 75 L/min; cfPWV: carotid-femoral pulse wave velocity; CI: confidence interval; cPP: central pulse pressure; eGFR: estimated glomerular filtration rate; NS: not significant; OR: odds ratio; paASG: peripheral-aortic arterial stiffness gradient; SE: standard error; std β: standardised β coefficient.
Similar findings were observed when the variables that predicted the decrease in eGFR (values lower than 60 mL/min/1.73 m2) were analysed in binary logistic regression. cfPWV was the only marker with significant predictive capacity for decreased eGFR (Table 4B).
Binary logistic regression. OR of arterial stiffness markers after multivariate adjustmenta predictors of decreased eGFR (<60 mL/min/1.73 m2).
| Variable | β | SE | OR (95% CI) | p | R2 of the model (Nagelkerke) |
|---|---|---|---|---|---|
| 0.37 | |||||
| cfPWV | 0.41 | 0.02 | 1.50 (1.17−1.92) | 0.001 | |
| AI75 | 0.03 | 0.01 | 1.03 (0.99−1.06) | NS | |
| paASG | –0.06 | 1.05 | 0.94 (0.12−7.40) | NS | |
| cPP | 0.06 | 0.01 | 1.00 (0.98−1.03) | NS |
Adjustment to mean arterial pressure, albumin/creatinine log, presence of DM, smoking, history of cardiovascular disease. AI75: augmentation index to 75 L/min; cfPWV: carotid-femoral pulse wave velocity; CI: confidence interval; cPP: central pulse pressure; eGFR: estimated glomerular filtration rate; NS: not significant; OR: odds ratio; paASG: peripheral-aortic arterial stiffness gradient; SE: standard error; std β: standardised β coefficient.
In multiple regression, after multivariate adjustment, the only arterial stiffness marker with a significant and positive association with the magnitude of albuminuria was cfPWV (Table 5A). cfPWV was also the only index of aortic stiffness with predictive capacity for abnormal albuminuria (odds ratio [OR]: 1.66; 95% confidence interval [CI]: 1.25−2.20) (Table 5B). When the stiffness markers were introduced individually, only cfPWV showed a significant predictive capacity for abnormal albuminuria.
Multiple linear regression of arterial stiffness markers associated with albuminuria value after multivariate adjustment.a
| Variable | F | R2 | β | SE | Std β | p |
|---|---|---|---|---|---|---|
| Constant | 28.31 | 0.53 | 3.35 | 1.43 | 0.02 | |
| cfPWV | 0.15 | 0.06 | 0.19 | 0.02 | ||
| AI75 | 0.00 | 0.00 | 0.02 | NS | ||
| paASG | –0.17 | 0.56 | –0.02 | NS | ||
| cPP | 0.00 | 0.00 | 0.00 | NS |
Adjustment to mean arterial pressure, albumin/creatinine log, presence of DM, smoking, history of cardiovascular disease. AI75: augmentation index to 75 L/min; cfPWV: carotid-femoral pulse wave velocity; CI: confidence interval; cPP: central pulse pressure; eGFR: estimated glomerular filtration rate; NS: not significant; OR: odds ratio; paASG: peripheral-aortic arterial stiffness gradient; SE: standard error; std β: standardised β coefficient.
Binary logistic regression. OR of arterial stiffness markers after multivariate adjustmenta predictors of increased albuminuria (albumin/creatinine >30 mg/g).
| Variable | β | SE | OR (95% CI) | p | R2 of the model (Nagelkerke) |
|---|---|---|---|---|---|
| 0.54 | |||||
| cfPWV | 0.51 | 0.14 | 1.66 (1.25−2.20) | 0.001 | |
| AI75 | 0.01 | 0.01 | 1.01 (0.97−1.04) | NS | |
| paASG | 0.49 | 1.16 | 1.64 (0.16−15.9) | NS | |
| cPP | 0.00 | 0.02 | 1.00 (0.98−1.02) | NS |
Adjustment to mean arterial pressure, albumin/creatinine log, presence of DM, smoking, history of cardiovascular disease. AI75: augmentation index to 75 L/min; cfPWV: carotid-femoral pulse wave velocity; CI: confidence interval; cPP: central pulse pressure; eGFR: estimated glomerular filtration rate; NS: not significant; OR: odds ratio; paASG: peripheral-aortic arterial stiffness gradient; SE: standard error; std β: standardised β coefficient.
Table 6 shows the variables with predictive value of kidney function and the various categories of albuminuria in the multinomial regression. cfPWV was the only arterial stiffness parameter that was significantly associated with decreased eGFR (OR [95% CI]: 1.63 [1.31−2.02]; p = 0.001), increased albuminuria (OR: 1.61 [1.29−2.03]; p = 0.001) and their combination (OR: 2.33 [1.90−2.85]; p = 0.001) (Table 6A). DM was significantly associated with increased albuminuria (OR: 3.34 [1.33−8.36]; p = 0.01) (Table 6A). No interaction was observed between DM and arterial stiffness parameters. Both the presence of DM and cfPWV were significantly associated with all grades of albuminuria (Table 6B).
Multinomial regression.
| A. Association of variables with the different categories of kidney function compared with normal kidney function (reference category) | ||||
|---|---|---|---|---|
| Variable | β | SE | OR (95% CI) | p |
| 1. Decreased eGFR (<60 mL/min/1.73 m2) | ||||
| Intersection | –5.33 | 1.14 | 0.001 | |
| Presence of DM | 0.051 | 0.01 | 1.05 (0.43−2.57) | NS |
| cfPWV | 0.49 | 0.11 | 1.63 (1.31−2.02) | 0.001 |
| 2. Albuminuria (>30 mg/g) | ||||
| Intersection | –5.95 | 1.04 | 0.001 | |
| Presence of DM | 1.20 | 0.46 | 3.34 (1.33−8.36) | 0.01 |
| cfPWV | 0.48 | 0.11 | 1.61 (1.29−2.03) | 0.001 |
| 3. Decreased eGFR + albuminuria | ||||
| Intersection | –8.06 | 0.96 | 0.001 | |
| Presence of DM | 0.10 | 0.38 | 1.10 (0.52−2.32) | NS |
| cfPWV | 0.84 | 0.10 | 2.33 (1.90−2.85) | 0.001 |
| B. Association of variables with the different categories of albuminuria compared with normal albuminuria (reference category) | ||||
|---|---|---|---|---|
| Variable | β | SE | OR (95% CI) | p |
| 1. High-normal | ||||
| Intersection | –4.57 | 0.92 | 0.001 | |
| Presence of DM | 1.46 | 0.43 | 4.30 (1.83−10.1) | 0.001 |
| cfPWV | 0.37 | 0.10 | 1.44 (1.17−1.78) | 0.001 |
| 2. Moderate | ||||
| Intersection | –6.58 | 0.91 | 0.001 | |
| Presence of DM | 1.05 | 0.39 | 2.86 (1.32−6.19) | 0.001 |
| cfPWV | 0.65 | 0.10 | 1.92 (1.58−2.34) | 0.001 |
| 3. Major | ||||
| Intersection | –9.24 | 1.12 | 0.001 | |
| Presence of DM | 1.21 | 0.45 | 3.35 (1.38−8.11) | 0.008 |
| cfPWV | 0.85 | 0.11 | 2.35 (1.88−2.94) | 0.001 |
cfPWV: carotid-femoral pulse wave velocity; CI: confidence interval; DM: diabetes mellitus; eGFR: estimated glomerular filtration rate.
NS: not significant; OR: odds ratio; SE: standard error.
Our results demonstrate that CKD is associated with an increase in CAS and a decrease in paASG; changes that are more marked when CKD coexists with DM. cfPWV is the CAS marker most independently associated with renal function and with the greatest predictive power of a decrease in eGFR and an increase in albuminuria.
Indicators of aortic stiffness in the presence of cardiovascular risk factors (arterial hypertension, diabetes mellitus, chronic kidney disease)Arterial stiffness is the expression of the effect that the interaction between haemodynamic and metabolic factors has on the arterial wall. Consequently, structural alterations occur in the vascular wall, resulting in an increase in the ratio between collagen and elastin, among other effects. There are many underlying mechanisms for increased arterial stiffness: molecular alterations induced by mechanotransduction between the extracellular matrix and vascular smooth muscle cells, phenotypic changes in these cells, endothelial dysfunction, oxidative stress, calcification of the vascular middle layer, metabolic abnormalities, inflammatory phenomena, perivascular adipose tissue, sex hormones and genetic and epigenetic factors.15–17 All of these mechanisms participate to varying degrees in the increase in arterial stiffness observed in the presence of different vascular risk factors, such as age, hypertension, DM and CKD.18
Similar to the normal ageing process, in the presence of these vascular risk factors, EVA occurs resulting in an increase in arterial stiffness.19
More than 90% of the subjects in our study were hypertensive. Hypertension is associated with increased arterial stiffness and, in turn, its increase leads to higher blood pressure.20 In addition to the structural modifications of the arterial wall caused by hypertension that induce a long-term increase in arterial stiffness, when blood pressure is raised acutely, the load supported by the vascular wall is transferred from the elastic fibres to the collagen fibres, increasing arterial stiffness. As has been shown in our study and others,4 there is a significant correlation (with quadratic function morphology) between age and cfPWV. Other factors such as sex and obesity can modify arterial stiffness.20,21 For all these reasons, it is necessary to consider these variables when analysing cfPWV.
In our study, cfPWV values in all subject groups were higher than in controls. However, after adjustment for age, blood pressure, sex and BMI, the significant difference between the control group and the group with hypertension disappeared. Despite the adjustment, subjects with DM, CKD and CKD + DM presented cfPWV values higher than those of the other groups. The largest contribution to the variance of the cfPWV was the group to which they belonged (27.7%), age (22.9%) and MAP (20.3%).
The cause of a similar marginal cfPWV value (after adjustment) in the control and HTN groups is unclear. It is possible that the criteria used to classify the groups, excluding from group 2 (HTN) those with albuminuria and decreased eGFR, generated a selection of subjects with better vascular health. It has been proven that, despite the presence of vascular risk factors, there are subjects with a vascular age (measured by cfPWV) lower than their chronological age (supernormal vascular ageing [SUPERNOVA]), with fewer vascular events. In the prospective study that validated the clinical significance of the concept of supernormal vascular age, 59.7% in the SUPERNOVA group had HTN.22 In our study, 27.5% of subjects in the HTN group had cfPWV values lower than the cut-off point of the 10th percentile of the European Society of Cardiology reference values for cfPWV.23 In this subgroup of our study, the cfPWV value, adjusted for age, sex and MAP, was 5.8 (1) m/s, and none had a history of CVD.
Another fact that could contribute to a lower cfPWV in all patient groups is treatment with RAS inhibitors: these drugs have the capacity to reduce arterial stiffness beyond their antihypertensive effects.24
As described in other studies, the presence of DM and CKD is associated with metabolic and inflammatory alterations, oxidative stress and vascular calcification, to name but a few, which induce an increase in arterial stiffness measured by cfPWV.25 In our research, groups 3 (DM) and 4 (CKD) had higher cfPWV values than the HTN group, although this difference was at the limit of statistical significance (p = 0.07) in the group that only had DM. The smaller number of subjects in this group may have limited significance. The duration of DM, which in this group was only two years, is an important determinant of aortic stiffness in DM. The role of DM in vascular damage and in the increase in arterial stiffness determined by cfPWV is reinforced by the fact that cfPWV was higher in the group with DN compared to subjects with non-diabetic glomerular nephropathy, despite a higher albuminuria value in the latter.
The higher cfPWV observed in the group with CKD + DM compared to the group with CKD can be attributed to the additive effect of metabolic and inflammatory alterations and oxidative stress that occur when the two processes simultaneously occur, and to the greater number and intensity of abdominal aortic calcifications that were observed in the group with CKD + DM. In subjects with CKD and DM, abdominal aortic calcification has been shown to be associated with elevated cfPWV values.26
Our study yielded similar results in arterial stiffness in the different groups using another arterial stiffness parameter; paASG. Applying this arterial stiffness index, the DM group had significantly lower values than the control and HTN groups. The difference in the cfPWV value between these groups was, however, at the limit of significance. During ageing or in the presence of vascular risk factors, aortic stiffness (measured by cfPWV) increases; however, the stiffness of the peripheral muscular arteries (measured by crPWV) hardly changes. Consequently, the paASG decreases progressively. Our study identified a significant correlation between age and cfPWV, a correlation that was not evident in the case of crPWV. One advantage of using the paASG is its independence from the MAP value.6 In fact, in our study, 20% of the variance of the cfPWV was dependent on the MAP. This percentage fell to 1% for paASG.
cPP is considered an indirect indicator of CAS. The loss of arterial elasticity reduces its distensibility and increases the speed of pulse wave transmission, producing an early return of the reflex wave that adds to the anterograde wave generated by ventricular systole, which translates into an increase in cSBP and, consequently, in cPP. Our study found that, after a multivariate adjustment, all subjects had a higher cPP than the control group, which was significant when CKD and DM both presented. Despite this, the percentage of subjects with a cPP greater than 50 mmHg, a value that has been shown to be predictive of cardiovascular events,27 was significantly higher in all subject groups. Other studies have shown that, in subjects with HTN and in patients with DM, increased cPP was associated with greater impedance of the proximal aorta and greater aortic stiffness12,28 and, in subjects with CKD,29 a direct correlation between cPP and PTH values, as we also observed in our research.
When arterial stiffness increases, the reflex wave propagates more quickly, joining the anterograde wave in systole with the consequent increase in the AI, which has been considered a marker of the reflex wave and, therefore, of arterial stiffness.30 In our research, the AI75 was significantly higher in all patients than in controls. Unlike the other markers of aortic stiffness, there were no differences in AI75 between the groups with HTN, DM and CKD, although cfPWV was higher in the groups with CKD, a finding also observed in other studies.10 Other research in subjects with DM verified the coexistence of an elevated cfPWV with AI75 and reflex wave values similar to or lower than the control group.28,31 An increase in aortic stiffness with a smaller increase or decrease in the reflex wave could suggest a greater penetration of pulsatile energy into the cerebral and renal microcirculation. However, this is inconsistent with the significant negative correlation between AI75 and paASG observed in our research. AI75 may not be a good marker of aortic stiffness and reflex wave. The limitations of AI75 as a measure of the magnitude of the reflex wave derive from the fact that it is influenced not only by the velocity of the pulse wave but also by other cardiac factors.32–34
It can be deduced from our findings that aortic stiffness increases in the presence of vascular risk factors such as HTN, DM and CKD. This increase is especially notable in subjects with CKD and in subjects with both CKD and DM. cfPWV and paASG are the most consistent markers for analysing CAS when the vascular risk factors studied here coexist.
The relevance of an increase in aortic stiffness will be determined by its possible impact on target organ damage that occurs in the presence of vascular risk factors, damage that may contribute to cardiovascular morbidity and mortality.
Indicators of aortic stiffness and kidney functionIndicators of aortic stiffness and estimated glomerular filtration rateThe other objective of our research was to analyse the possible association between aortic stiffness and two parameters of kidney function: GFR and albuminuria.
Analysing all subjects together, we observed a significant correlation between all the studied markers of aortic stiffness and the eGFR (direct correlation in the case of paASG and inverse correlation in the other indicators), and between these indicators and albuminuria (inverse correlation in the case of paASG and direct correlation in the others).
When all the aortic stiffness markers were entered into the multiple regression, cfPWV and AI75 were the only ones that, after multivariate adjustment, were independently and significantly associated with the magnitude of the eGFR, while in the logistic regression only cfPWV was a predictor of subnormal eGFR. Entered individually and after multivariate adjustment, all stiffness markers were significantly associated with eGFR and predicted its decline, but cfPWV was the most robust marker associated with eGFR.
The highest eGFR value of the group with CKD + DM compared to the CKD group persisted when the MANOVA was adjusted for cfPWV. In light of the above, in our research, the negative effect of aortic stiffness on the eGFR value seems to be overcome by DM-induced hyperfiltration.
There are few studies that analyse the association between GFR and albuminuria with various arterial stiffness parameters. The results of some studies on GFR and aortic arterial stiffness have not been consistent. A progressive increase in cfPWV with CKD stage and an independent association between cfPWV and GFR has been demonstrated even in very early stages of kidney failure.35–37 Another study found an association between aortic stiffness determined by cfPWV and eGFR in subjects with and without HTN and DM.9
Other studies, however, have failed to demonstrate an association between central arterial stiffness and GFR. Upadhyay et al.11 found in a Framingham cohort that, in mild-moderate CKD, GFR was not independently associated with aortic stiffness assessed by several indices (cfPWV, cPP, AI). The cause of this discrepancy is unclear. The use of cystatin to estimate GFR and a highly rigorous multivariate adjustment for cardiovascular risk factors in the Upadhyay study may have contributed to the different results. These risk factors may have significant effects on arterial stiffness in subjects with CKD. In our research, we continued to observe a significant association between cfPWV and eGFR when the lipid profile was added to the other adjustment variables.
It can be concluded that there is an inverse association between aortic stiffness and eGFR, and a significant predictive value of the former for a decrease in eGFR in subjects with vascular risk factors. cfPWV is the most robust index of aortic stiffness compared to other central stiffness markers.
Indicators of aortic stiffness and albuminuriaIn our research, aortic stiffness determined by cfPWV, after multivariate adjustment, was directly and significantly associated with the magnitude and prevalence of albuminuria. As in the case of eGFR, all other stiffness markers disappeared from the model when cfPWV was incorporated. However, taken individually, all were associated with albuminuria, although much less strongly than cfPWV.
Other studies have shown a relationship between aortic stiffness and albuminuria. In a study carried out in the Framingham cohort,37 an independent association between cfPWV and cPP, and the prevalence of albuminuria, was observed with a quantitatively higher OR for cfPWV. In other population studies, both eGFR and albuminuria were independently associated with aortic stiffness,9 identifying an inverse correlation with eGFR and a direct correlation with albuminuria. The direct association between arterial stiffness and albuminuria was observed, even with albuminuria values considered normal.38 In some publications, the direct relationship between arterial stiffness and albuminuria is stronger and more consistent than the inverse relationship between aortic stiffness and GFR.11,35
In our study, the association between a decrease in eGFR and an increase in albuminuria with cfPWV was not substantially modified when both were included in the regression. This raises the possibility that the mechanisms linking these variables with cardiovascular risk are, at least in part, independent of each other, even though they may share factors such as hypertension and DM.
Our research shows that increased arterial stiffness, assessed by cfPWV, is a crucial determinant of the two parameters of kidney function: eGFR and albuminuria. DM and increased arterial stiffness contribute significantly to the presence and magnitude of albuminuria without observing a significant interaction between them. The significant association of both variables with albuminuria, when included together in the model, suggests that their effect on albuminuria is exerted through different processes.
The mechanism by which increased aortic stiffness contributes to kidney dysfunction is unclear. Woodard et al. demonstrated an inverse relationship between GFR determined by iohexol clearance and aortic stiffness. With a mediation analysis, they showed that aortic stiffness can contribute to decreased GFR by transmitting excessive pulsatility to the renal microcirculation that promotes dynamic vasoconstriction and vascular rarefaction.39 In another sense, an increase in the aortic retrograde/antegrade flow ratio, observed in cases of increased aortic stiffness and which is inversely correlated with intrarenal blood flow, may be the mediator of the association between increased aortic stiffness and decreased GFR.40 Renal microvascular damage and haemodynamic alterations promoted by increased aortic pulse pressure secondary to increased aortic stiffness can also cause albuminuria.41
The presence of a normal peripheral-aortic arterial stiffness gradient contributes, on the one hand, to maintaining coronary perfusion and avoiding cardiac overload and, on the other, limits the transmission of pulsatile energy to the periphery and protects the microcirculation of organs with normal low resistance, such as the kidney and the brain.42 Considering the pathophysiological consequences of a decrease in the gradient, it has been proposed that the stiffness gradient, assessed by the crPWV/cfPWV ratio could be better than cfPWV for assessing the possible association of aortic stiffness with target organ damage and morbidity and mortality. In dialysis-treated CKD subjects, paASG has greater predictive power for mortality than cfPWV.43 This finding has not been confirmed in population studies.44 On the other hand, in subjects with HTN, the paASG has shown a significant association with GFR similar to the cfPWV, but in the opposite direction.45 In our study, paASG, like the other markers of aortic stiffness (although in the opposite direction), was associated with the magnitude of the eGFR and albuminuria when entered in isolation in the regression model, but its significant association disappeared when cfPWV was included in the model, which was the marker of stiffness most consistently associated with kidney dysfunction. From our findings it can be deduced that the decrease in paASG is fundamentally attributable to an increase in cfPWV (which should continue to be considered the most important marker of aortic stiffness) rather than to a decrease in crPWV.
Cardiac consequences of increased aortic stiffnessIn addition to its impact on renal function, increased aortic stiffness also has cardiac effects. An increase in cfPWV favours the arrival of the reflex wave in the ascending aorta during systole, increasing the cSBP with the consequent cardiac overload and, on the other hand, decreases the aortic diastolic blood pressure, compromising coronary perfusion, which occurs mainly in diastole. Experimental studies have shown that a stiff proximal aorta is associated with a reduction in coronary perfusion, especially at the subendocardial level.46 In our study, we observed a direct correlation between the Buckberg index, a non-invasive estimate of oxygen delivery and subendocardial perfusion, with eGFR, and an inverse correlation with albuminuria, as well as an inverse correlation with aortic stiffness parameters (except for a direct relationship with paASG). However, in multiple regression, after multivariate adjustment, the only aortic stiffness marker independently and inversely associated with Buckberg index magnitude was cfPWV.
It has been shown that, both in the general population and in high vascular risk populations, eGFR and albuminuria, independently of other traditional vascular risk factors, predict cardiovascular morbidity and mortality.47 The association observed in our study of aortic stiffness with eGFR, albuminuria and subendocardial perfusion raises the possibility that increased aortic stiffness may be the link between kidney dysfunction and cardiovascular events.
ConclusionsIt can be concluded from our findings that aortic stiffness increases in the presence of vascular risk factors such as HTN, DM and CKD. This increase is particularly notable in subjects with CKD, and in subjects with both CKD and DM. Greater aortic stiffness is inversely and independently associated with the magnitude of eGFR, and directly correlated with the amount of albuminuria. On the other hand, increased aortic stiffness predicts decreased eGFR and abnormal albuminuria. cfPWV is the aortic stiffness parameter that is most significantly and consistently associated with kidney dysfunction. Although cfPWV depends fundamentally on the thickness and elasticity of the aortic wall and the iliofemoral arteries, it can integrate the different, but haemodynamically related variables that determine the other markers of aortic stiffness.
Our study has limitations. It is a cross-sectional study, owing to which a causal relationship between aortic stiffness and kidney dysfunction cannot be established. In reality, it is a two-way association. An increase in aortic stiffness can cause renal alterations while, in CKD, there are multiple pathophysiological alterations that can lead to an increase in aortic stiffness. Additionally, there are independent variables that simultaneously affect the elasticity of the vascular wall and cause kidney damage. In our study, not all laboratory tests were performed on all subjects, which may limit the effect of these variables on the observed associations. However, the inclusion of available laboratory variables in our regression analyses did not substantially alter the results.
Our research also has relevant aspects. The cfPWV was used, which is considered the gold standard for the study of aortic stiffness. A significant number of subjects were gathered and distributed into groups representative of different vascular risk factors. To the best of our knowledge, there are no studies analysing aortic stiffness in such a diverse group of patients. Finally, the use of a rigorous statistical methodology allows us to analyse the association of the various variables with adjustments to minimise the effects of age differences and comorbidities between the different groups.
Prospective studies are required to analyse the true involvement of CAS and peripheral alterations in target organ lesions and cardiovascular morbidity and mortality in subjects with vascular risk factors.
FundingNo funding was received for this paper.