Spontaneous rupture of tendons (STR) is not frequent. The pathogenesis is unclear but there are a number risk factors involved: secondary hyperparathyroidism (HPTH), diabetes mellitus, obesity, rheumatoid arthritis, gout, statins, steroids, fluorquinolones and the presence of B and/or C hepatitis virus. In patients with chronic renal failure (CKD) the most frequent cause of tendon rupture is secondary hyperparathyoridims, which is present in most of these patients.1,2
There is no consensus about the treatment. Thus the objective of this study is to analyze the clinical features, risk factors, treatment and clinical evolution of STR in CKD patients.
The study includes end stage renal disease patients on renal replacement therapy that had STR during the years 1994 to 2013. Patients had a complete clinical history and they had a least one-year of follow up. Patient with tendon rupture caused by trauma or those with of the lost follow up were excluded.
There were six patients (0.23%) with STR. Mean age was 46.6±11.8 years, 4 were males (66.7%). Before the episode of STR all patients had been on hemodialysis for an average of 9.1±4.2 years. In 4 cases (66.7%) the STR affected the extremity of one body side and in 2 cases (33.3) they were bilateral.
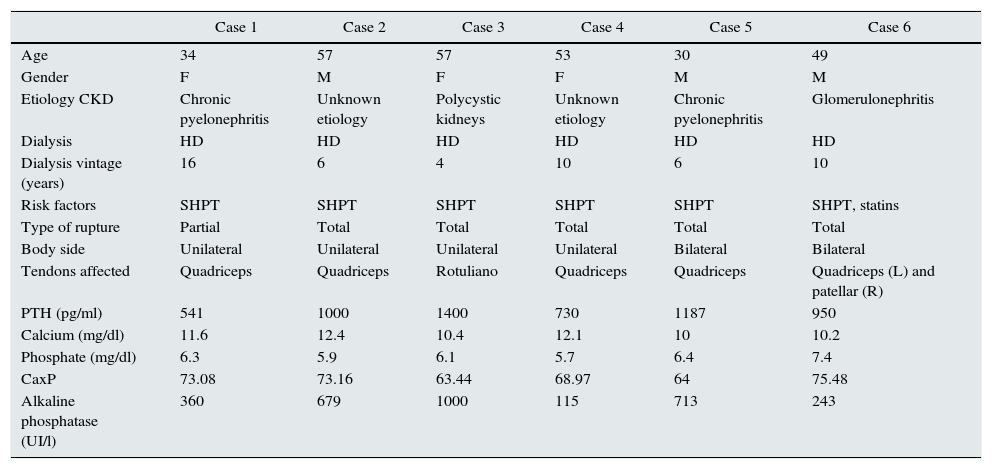
In six patients there was a rupture of the femoral quadriceps tendon and in 2 cases the patellar tendon was affected. All patients had SHPT and one patient (16.6%) also receive statins to treat hypercholesterolemia (Table 1).
Clinical features of spontaneous tendon rupture.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | |
|---|---|---|---|---|---|---|
| Age | 34 | 57 | 57 | 53 | 30 | 49 |
| Gender | F | M | F | F | M | M |
| Etiology CKD | Chronic pyelonephritis | Unknown etiology | Polycystic kidneys | Unknown etiology | Chronic pyelonephritis | Glomerulonephritis |
| Dialysis | HD | HD | HD | HD | HD | HD |
| Dialysis vintage (years) | 16 | 6 | 4 | 10 | 6 | 10 |
| Risk factors | SHPT | SHPT | SHPT | SHPT | SHPT | SHPT, statins |
| Type of rupture | Partial | Total | Total | Total | Total | Total |
| Body side | Unilateral | Unilateral | Unilateral | Unilateral | Bilateral | Bilateral |
| Tendons affected | Quadriceps | Quadriceps | Rotuliano | Quadriceps | Quadriceps | Quadriceps (L) and patellar (R) |
| PTH (pg/ml) | 541 | 1000 | 1400 | 730 | 1187 | 950 |
| Calcium (mg/dl) | 11.6 | 12.4 | 10.4 | 12.1 | 10 | 10.2 |
| Phosphate (mg/dl) | 6.3 | 5.9 | 6.1 | 5.7 | 6.4 | 7.4 |
| CaxP | 73.08 | 73.16 | 63.44 | 68.97 | 64 | 75.48 |
| Alkaline phosphatase (UI/l) | 360 | 679 | 1000 | 115 | 713 | 243 |
R: right; M: male; HD: hemodialysis; SHPT: secondary hyperparathyroidism; L: left; CKD: chronic renal failure; F: female.
All patients underwent urgent (within 5 days) surgical intervention to repair the tendon fracture. In five cases the tendon was detached with respect to the patella and it was reinserted using nonabsorbable suture through transosseous tunnels in the patella. In 3 cases there was a rupture of the tendon and it had to be repaired by end-to-end suture with a material that is not absorbable. Thereafter, the knee had to be immobilized for 8 weeks followed by a rehabilitation period of up to six months after surgery
With respect to the SHPT, all patients had bone pain and one patient (16.6%) complained of pruritus that was refractory to treatment. Mean serum concentration of PTH was 968±308.2pg/ml, the CaxP was 69.6±17.6 and the mean value of alkaline phosphatase was 518.3±334.4UI/l. All patients underwent total parathyroidectomy after a mean period of 3.6±1.7 months.
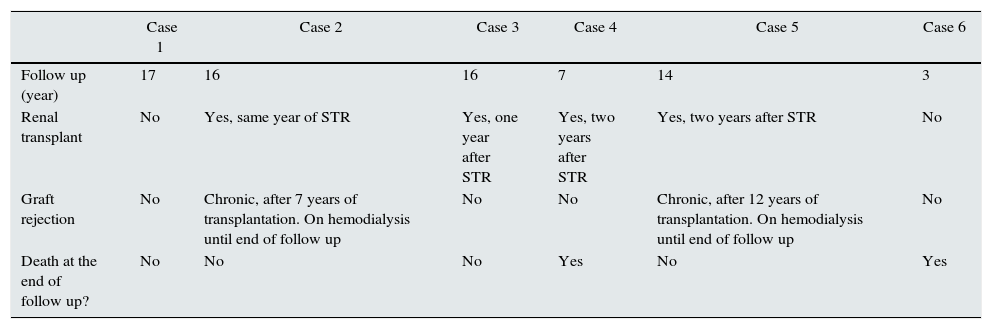
After 12.5±5 year of follow up there was no further evidence of STR or SHPT and 4 patients (66.7%) underwent renal transplantation (Table 2).
Clinical follow up.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | |
|---|---|---|---|---|---|---|
| Follow up (year) | 17 | 16 | 16 | 7 | 14 | 3 |
| Renal transplant | No | Yes, same year of STR | Yes, one year after STR | Yes, two years after STR | Yes, two years after STR | No |
| Graft rejection | No | Chronic, after 7 years of transplantation. On hemodialysis until end of follow up | No | No | Chronic, after 12 years of transplantation. On hemodialysis until end of follow up | No |
| Death at the end of follow up? | No | No | No | Yes | No | Yes |
The feature of a CKD patient with STR is a relatively young patient on hemodialysis for more that 5 years that may be malnourished, with insufficient dose of dialysis, amyloidosis, chronic acidosis and also SHPT which is the most important pathogenic factor for STR.1–5 The pathophysiology is not totally clear; it has been proposed that the increased subperiostial resorption together with elastosis of the connective tissue due to chronic acidosis may debilitate the ostetendinous junction favoring the STR.6–8
STR affecting extensor knee required urgent or immediate surgery, it has to be done within the first few days after rupture, so fibrosis and retraction of tendon and muscle are avoided. Optimal results require immobilization and 4–6 months of rehabilitation.9
In addition to the treatment of STR, it is necessary to control risk factors to prevent new STR. Therefore SHPT should be treated, the use of calcimimetics have markedly reduced the need for parathyroidectomy. In patients with STR and persistent hyperparathyroidism, parathyroidectomy is reccomended.10
In conclusion, STR in CKD patients usually affect the knee extensor tendons; it is more frequent in young males with more than nine years in hemodialysis and the main predisposing factor is SHPT. Quick surgical treatment, rehabilitation and treatment of SHPT allows patient's recovery and prevents long term re-occurrence.
Please cite this article as: Ruiz J, Ríos A, Rodríguez JM, Llorente S. Roturas tendinosas espontáneas en la insuficiencia renal crónica. Nefrologia. 2017;37:341–343.