Information provided by health professionals to potential donors and recipients is essential for an autonomous and objective decision to make a living kidney donation.
ObjectivesTo determine the characteristics of the information received by living kidney donors and recipients, to find out their socio-sanitary profile, their socio-demographics, financial and labor characteristics, health and the caregiving activity of these donors and recipients.
MethodsObservational, descriptive and cross-sectional study of the population of living kidney donors and recipients from the University Hospitals Puerta del Mar (Cádiz), Virgen del Rocío (Seville), and the University Hospital Complex of Granada, between 08/04/2014 and 08/06/2015.
Results and conclusionsAccording to the 40 living kidney donors and their 40 recipients surveyed, it is mainly nephrologists who make people aware and provide information about living kidney donation. Almost half of recipients require more information so the evaluation processes and pre-donation information should be updated. In general, the living kidney donor is female, aged 50, with primary/secondary education, lives with a partner and is related to the kidney recipient. Also, the living kidney donor is in paid employment, is overweight, perceives her health as very good or good, and does not smoke or drink alcohol. However, the typical living kidney recipient is male, aged 44 and has completed secondary school studies and vocational training. Furthermore, he does not work, perceives his health as good or regular, and he is an independent person for activities of daily living.
La información suministrada por profesionales sanitarios a posibles donantes y receptores es fundamental para una decisión autónoma y objetiva de donar un riñón en vida.
ObjetivosConocer las características de la información que reciben los donantes y receptores renales de vivo, averiguando su perfil sociosanitario, sus características sociodemográficas, económico-laborales, de salud y la actividad cuidadora de dichos donantes y receptores.
MétodosEstudio observacional, descriptivo, transversal, de la población de donantes y receptores renales de vivo, de los Hospitales Universitarios Puerta del Mar (Cádiz), Virgen del Rocío (Sevilla) y Complejo Hospitalario Universitario de Granada, entre el 8 de abril de 2014 y el 8 de junio de 2015.
Resultados y conclusionesSegún los 40 donantes y 40 receptores renales de vivo encuestados, los facultativos de nefrología son principalmente quienes dan a conocer e informan sobre la donación renal en vida. Casi la mitad de receptores demandan más información, por lo que se deberían actualizar los procesos de evaluación y de información antes de la donación. En general, el donante renal vivo es mujer, de 50años, con estudios de Primaria/ESO, vive en pareja, está emparentado con el receptor del riñón, realiza un trabajo remunerado, tiene sobrepeso, percibe su salud como muy buena o buena, y no fuma ni consume alcohol. Sin embargo, el receptor renal tipo es hombre, con 44años, tiene estudios de bachillerato/FP, no trabaja, percibe su salud como buena o regular, y son personas independientes para las actividades de la vida diaria.
The shortage of cadaveric organs for transplantation1 and the better results obtained with live donor kidney transplantation (LDKT) make this transplant modality the best and first option that should be offered to those who need short-term renal replacement therapy.2,3 The LDKT aims to significantly improve the survival prognosis and rehabilitation of the living kidney receptor, with minimal damage to the living kidney donor. In an adequately selected live kidney donor the risk of requiring dialysis or transplantation in the future is so small that there is consensus on the ethical justification of donation, under the assumption that the donor is well informed and is free to makes such decision.4–9
Health professionals are key in the final decision of the potential living kidney donor.1 The information provided to patients about the donation process in life is fundamental. It is one of the factors that allow an autonomous and objective decision so, if the kidney transplant is not contraindicated, the donor will consider that the option of the LDKT is of minimum risk and maximum benefit for the receptor.3
In addition to accurate and real knowledge about the process of organ donation and transplantation, the manner in which a person is informed often generates feelings about the donation, and has been positively associated with the attitude toward donation and the decision making process to donate in life.10 The number of living donors and transplants increases when the information is given in an appropriate environment with an optimal presentation and quality of information to patients and family members.11 This is important given the relationship between information provided by health professionals, knowledge, attitude and willingness to donate organs in life.10
Regarding the information of the LDKT process, there are studies taking place in areas and populations different from ours that do not analyze certain characteristics such as the informants, the format of communication used and how donors and recipients perceive the information received. In United States it has been identified aspects of the information and education that may increase the number of living donors for black people, in other minorities, older adults and in patients with low incomes. It was assumed that LDKT was more likely to occur in whites, younger adults and in high family income.12–14
Consequently, we conducted an investigation aiming to learn about the characteristics of the information received by donors and living kidney receptors, before and during the process of evaluation of potential donors and receptors, as well as evaluating their socio-health profile, the sociodemographic characteristics, economic-employment status, health and caregiving activities of donors and receptors.
Achieving these objectives may help to improve renal donation in life. To increase donations, “it is necessary to inform more and better” to both, health professionals and patients.3 It is also important to know the social and health status of living kidney donors and receptors, since some features may predict the levels of well-being and the manifestation of psychological symptoms in the living donor after donation.15 Also acquire a real vision of the donors and recipients, their social and family environment, the style and habits of life, health status, the characteristics that distinguish them from other groups, and even identify the behavior of the population where donors and recipients come from in relation to the LDKT.16
MethodsTo achieve these objectives, we have performed an observational, descriptive, cross-sectional study including individuals who donated or received a live kidney, between April 8, 2014 and June 8, 2015, in the following University Hospitals: Puerta del Mar (HUPM), of Cádiz, Virgen del Rocío (HUVR), of Seville, and in the University Hospital Complex of Granada (CHUG). All these hospitals belong to the Public Health System of Andalusia.
The target population was all individuals who donated a kidney and the recipients of a kidney from living donor. Recipients under 18 years of age were excluded from the study.
In both living donors and recipients the following information was obtained: sociodemographic data, donor-recipient relationship, living address, employment status, sources of income, whether they had the responsibility of taking care of family members and for how long the had such a duty. To assess their health profile the following parameters were evaluated: weight, height, body mass index (BMI), self perception of health, hospital admissions, visits to emergency rooms, and consumption of tobacco and alcohol. The calculation of daily alcohol consumption was made using the standard drink unit.17
Regarding the characteristics of the information received by living kidney donors and recipients, we identified the informant and how the information was received. In addition, in donors taking care of family members we obtained information about the extrawork as caregivers. In kidney recipients we collected information on the etiology of chronic kidney disease (CKD), the type of renal replacement therapy before transplantation, time on dialysis and on the waiting list, and the degree of autonomy for daily activities.
Researchers collected the information through interviews, before the donation and actual graft implant, to those individuals who accepted to participate in the study.
The protocol was approved by the Research Ethics Committee of the HUVR, under the CEI 2013/PI153 file.
The analysis of the data was made with the statistical program IBM SPSS 21.0 for Windows. The qualitative variables are expressed as frequencies and percentages and the numerical variables with normal distribution are presented as means, standard deviations and maximum and minimum values.
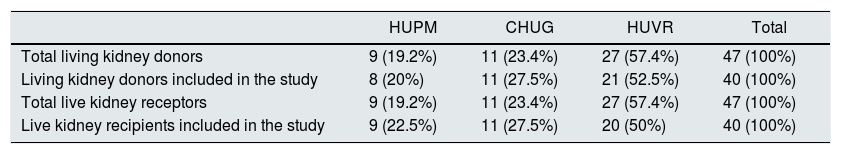
ResultsDuring the study period in the 3 hospitals there were 47 kidney living donors, of which 5 (10.6%) did not answer the survey because they did not have the time to do it before the donation and 2 (4.3%) did not agree to participate in the study. Forty seven patients received a live kidney, of which 4 (8.5%) did not participate in the study because they did not have the time to do it before transplantation and 3 (6.4%) because were not adults (Table 1).
Donations and live kidney transplants, separated by hospitals, from April 8, 2014 to June 8, 2015.
| HUPM | CHUG | HUVR | Total | |
|---|---|---|---|---|
| Total living kidney donors | 9 (19.2%) | 11 (23.4%) | 27 (57.4%) | 47 (100%) |
| Living kidney donors included in the study | 8 (20%) | 11 (27.5%) | 21 (52.5%) | 40 (100%) |
| Total live kidney receptors | 9 (19.2%) | 11 (23.4%) | 27 (57.4%) | 47 (100%) |
| Live kidney recipients included in the study | 9 (22.5%) | 11 (27.5%) | 20 (50%) | 40 (100%) |
CHUG, Complejo Hospitalario Universitario de Granada (Granada); HUPM, Hospital Universitario Puerta del Mar (Cádiz); HUVR, Hospital Universitario Virgen del Rocío (Sevilla).
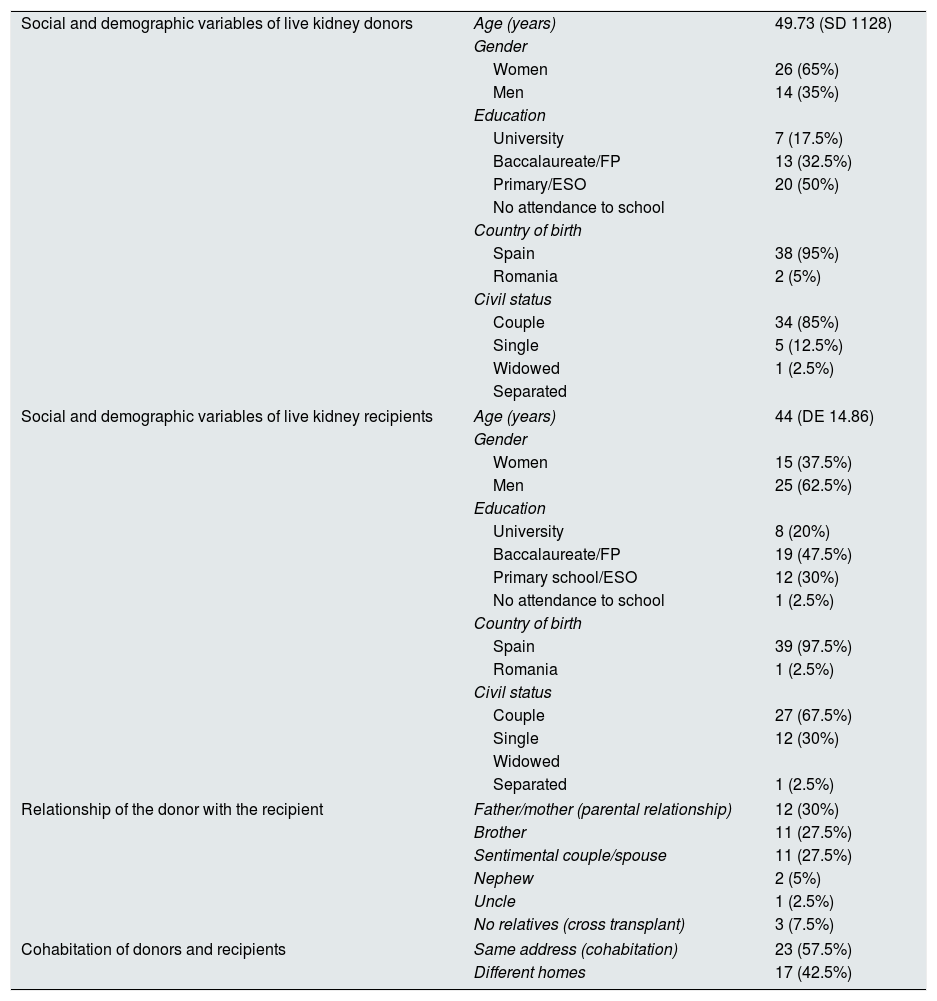
There were more women donors than men (65% vs 35%). A 50% of the donors had a low or very low level of education. This percent decreased to 32.5% in the group of recipients, in fact a 67.5% had high school or university studies. The majority of donations were between relatives (92.5%) within the same family, specially between parents and children, siblings or partner (85%) (Table 2).
Social and demographic profile of living kidney donors and recipients.
| Social and demographic variables of live kidney donors | Age (years) | 49.73 (SD 1128) |
| Gender | ||
| Women | 26 (65%) | |
| Men | 14 (35%) | |
| Education | ||
| University | 7 (17.5%) | |
| Baccalaureate/FP | 13 (32.5%) | |
| Primary/ESO | 20 (50%) | |
| No attendance to school | ||
| Country of birth | ||
| Spain | 38 (95%) | |
| Romania | 2 (5%) | |
| Civil status | ||
| Couple | 34 (85%) | |
| Single | 5 (12.5%) | |
| Widowed | 1 (2.5%) | |
| Separated | ||
| Social and demographic variables of live kidney recipients | Age (years) | 44 (DE 14.86) |
| Gender | ||
| Women | 15 (37.5%) | |
| Men | 25 (62.5%) | |
| Education | ||
| University | 8 (20%) | |
| Baccalaureate/FP | 19 (47.5%) | |
| Primary school/ESO | 12 (30%) | |
| No attendance to school | 1 (2.5%) | |
| Country of birth | ||
| Spain | 39 (97.5%) | |
| Romania | 1 (2.5%) | |
| Civil status | ||
| Couple | 27 (67.5%) | |
| Single | 12 (30%) | |
| Widowed | ||
| Separated | 1 (2.5%) | |
| Relationship of the donor with the recipient | Father/mother (parental relationship) | 12 (30%) |
| Brother | 11 (27.5%) | |
| Sentimental couple/spouse | 11 (27.5%) | |
| Nephew | 2 (5%) | |
| Uncle | 1 (2.5%) | |
| No relatives (cross transplant) | 3 (7.5%) | |
| Cohabitation of donors and recipients | Same address (cohabitation) | 23 (57.5%) |
| Different homes | 17 (42.5%) | |
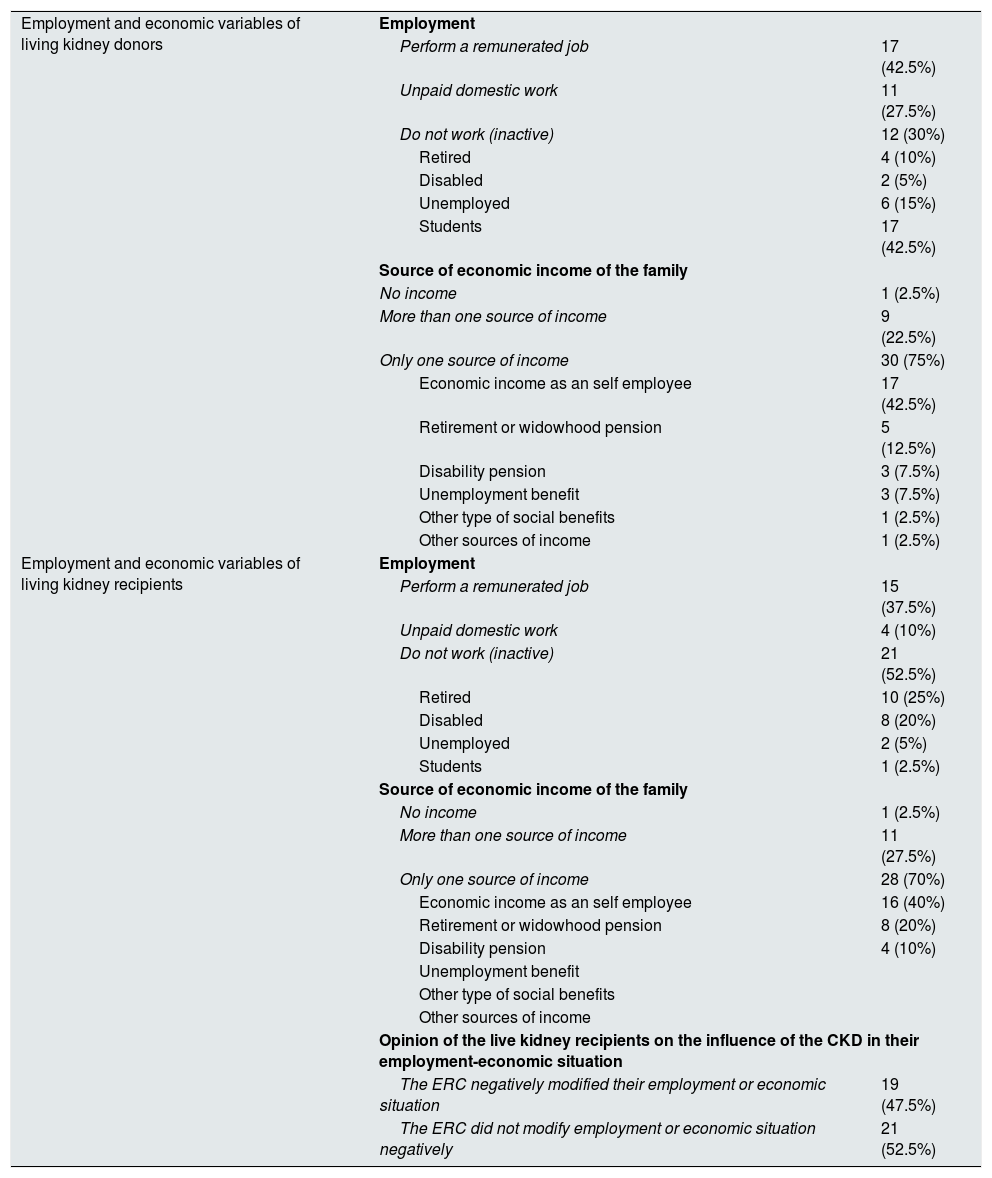
Almost one third of the living kidney donors were not employed (30%), and t half of the recipients of a live kidney were also unemployed (52.5%). Almost all donors (95%) and living kidney recipients (95%) had some source of income from their families (Table 3).
Employment and economic profile of living kidney donors and recipients.
| Employment and economic variables of living kidney donors | Employment | |
| Perform a remunerated job | 17 (42.5%) | |
| Unpaid domestic work | 11 (27.5%) | |
| Do not work (inactive) | 12 (30%) | |
| Retired | 4 (10%) | |
| Disabled | 2 (5%) | |
| Unemployed | 6 (15%) | |
| Students | 17 (42.5%) | |
| Source of economic income of the family | ||
| No income | 1 (2.5%) | |
| More than one source of income | 9 (22.5%) | |
| Only one source of income | 30 (75%) | |
| Economic income as an self employee | 17 (42.5%) | |
| Retirement or widowhood pension | 5 (12.5%) | |
| Disability pension | 3 (7.5%) | |
| Unemployment benefit | 3 (7.5%) | |
| Other type of social benefits | 1 (2.5%) | |
| Other sources of income | 1 (2.5%) | |
| Employment and economic variables of living kidney recipients | Employment | |
| Perform a remunerated job | 15 (37.5%) | |
| Unpaid domestic work | 4 (10%) | |
| Do not work (inactive) | 21 (52.5%) | |
| Retired | 10 (25%) | |
| Disabled | 8 (20%) | |
| Unemployed | 2 (5%) | |
| Students | 1 (2.5%) | |
| Source of economic income of the family | ||
| No income | 1 (2.5%) | |
| More than one source of income | 11 (27.5%) | |
| Only one source of income | 28 (70%) | |
| Economic income as an self employee | 16 (40%) | |
| Retirement or widowhood pension | 8 (20%) | |
| Disability pension | 4 (10%) | |
| Unemployment benefit | ||
| Other type of social benefits | ||
| Other sources of income | ||
| Opinion of the live kidney recipients on the influence of the CKD in their employment-economic situation | ||
| The ERC negatively modified their employment or economic situation | 19 (47.5%) | |
| The ERC did not modify employment or economic situation negatively | 21 (52.5%) | |
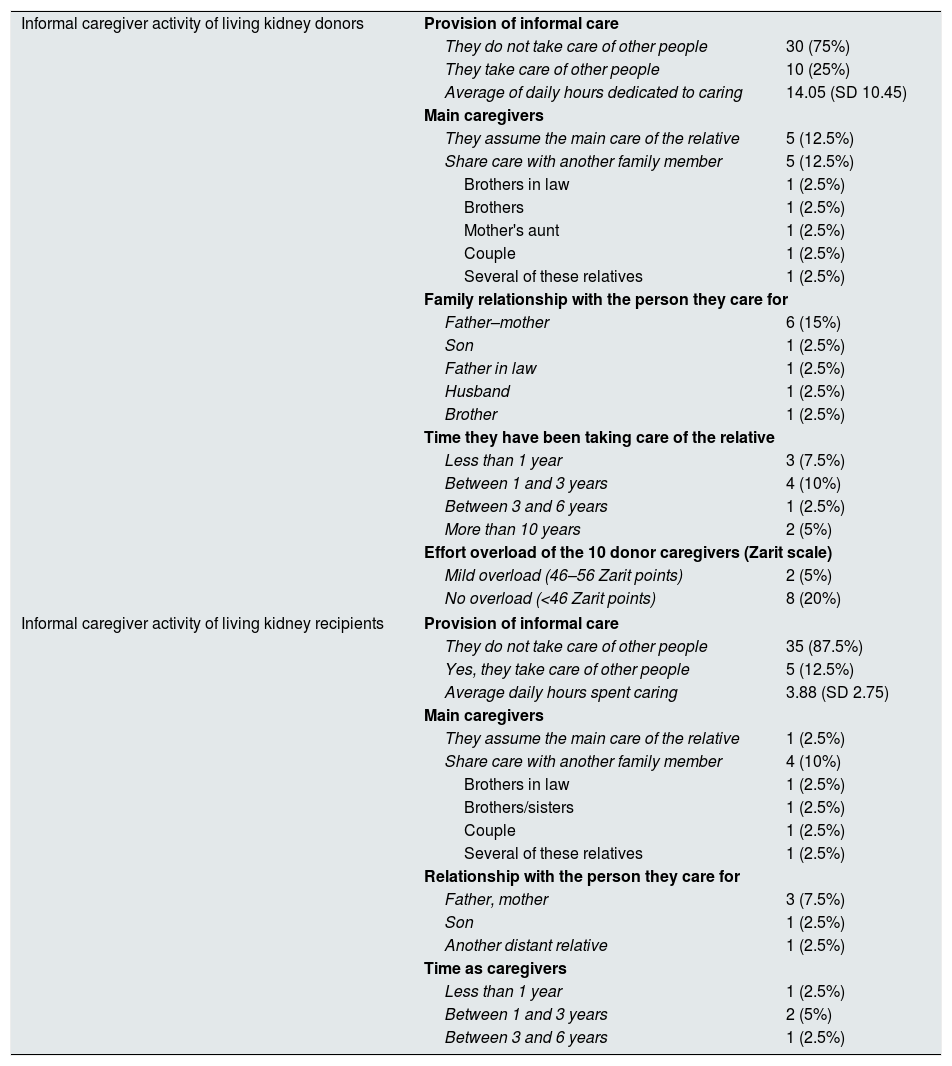
Thirteen donors (32.5%) and 13 recipients (32.5%) had a family member of less than 15 years of age, but only 6 donors (15%) and 5 recipients (12.5%) had the responsibility of caring for these children.
Likewise, one out of four donors provided informal care to family members, mainly parents (17.5%); on average, they spent more than half day dedicated to such activity (14.05h/day). A 12.5% of recipients provided informal care to relatives, mostly parents, and devoted to this activity a little less than one sixth of the day (3.88h/day) (Table 4).
Informal caregiver activity of living kidney donors and recipients.
| Informal caregiver activity of living kidney donors | Provision of informal care | |
| They do not take care of other people | 30 (75%) | |
| They take care of other people | 10 (25%) | |
| Average of daily hours dedicated to caring | 14.05 (SD 10.45) | |
| Main caregivers | ||
| They assume the main care of the relative | 5 (12.5%) | |
| Share care with another family member | 5 (12.5%) | |
| Brothers in law | 1 (2.5%) | |
| Brothers | 1 (2.5%) | |
| Mother's aunt | 1 (2.5%) | |
| Couple | 1 (2.5%) | |
| Several of these relatives | 1 (2.5%) | |
| Family relationship with the person they care for | ||
| Father–mother | 6 (15%) | |
| Son | 1 (2.5%) | |
| Father in law | 1 (2.5%) | |
| Husband | 1 (2.5%) | |
| Brother | 1 (2.5%) | |
| Time they have been taking care of the relative | ||
| Less than 1 year | 3 (7.5%) | |
| Between 1 and 3 years | 4 (10%) | |
| Between 3 and 6 years | 1 (2.5%) | |
| More than 10 years | 2 (5%) | |
| Effort overload of the 10 donor caregivers (Zarit scale) | ||
| Mild overload (46–56 Zarit points) | 2 (5%) | |
| No overload (<46 Zarit points) | 8 (20%) | |
| Informal caregiver activity of living kidney recipients | Provision of informal care | |
| They do not take care of other people | 35 (87.5%) | |
| Yes, they take care of other people | 5 (12.5%) | |
| Average daily hours spent caring | 3.88 (SD 2.75) | |
| Main caregivers | ||
| They assume the main care of the relative | 1 (2.5%) | |
| Share care with another family member | 4 (10%) | |
| Brothers in law | 1 (2.5%) | |
| Brothers/sisters | 1 (2.5%) | |
| Couple | 1 (2.5%) | |
| Several of these relatives | 1 (2.5%) | |
| Relationship with the person they care for | ||
| Father, mother | 3 (7.5%) | |
| Son | 1 (2.5%) | |
| Another distant relative | 1 (2.5%) | |
| Time as caregivers | ||
| Less than 1 year | 1 (2.5%) | |
| Between 1 and 3 years | 2 (5%) | |
| Between 3 and 6 years | 1 (2.5%) | |
The 10 donors that took care of their relatives obtained in the “Career-Zarit Overload Scale” an average of 34.2±8.43 points, with the minimum and maximum values of 23 and 49 points. Two (5%) of these 10 donors caregivers obtained a Zarit score of 49 points each, which is considered a moderate overload (Table 4).
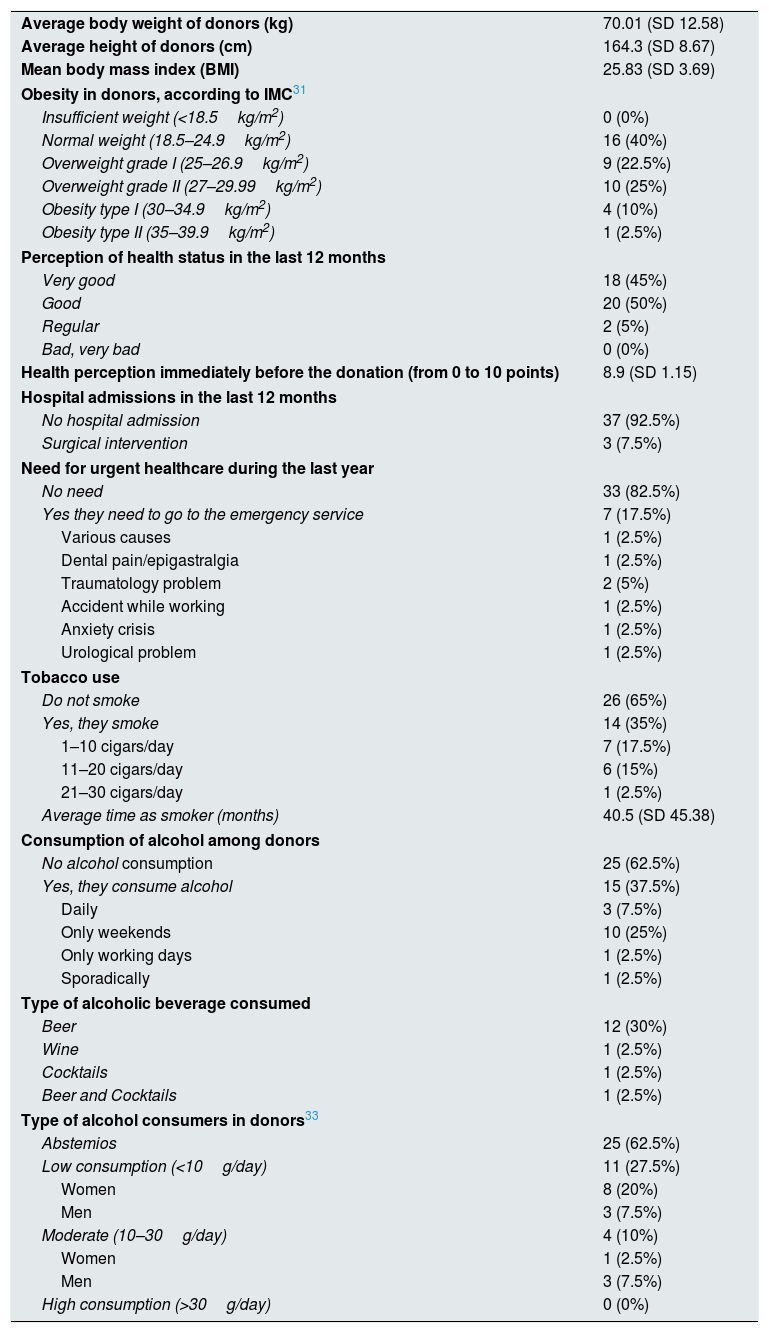
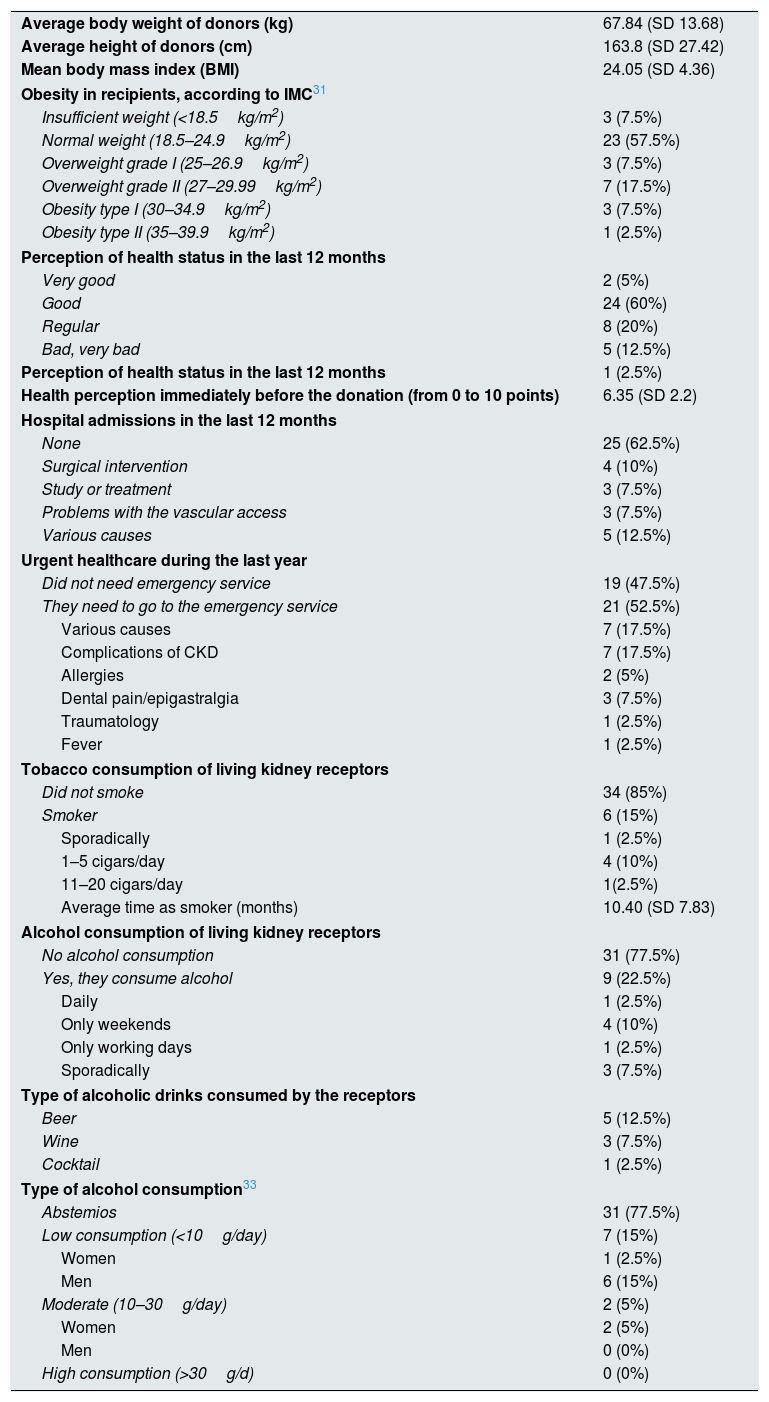
Health profile of living kidney donors and recipientsSixty percent of donors had some degree of obesity or overweight, none had a bad perception their health in the last year slightly more than a one third of donors smoked (35%) and consumed alcohol (37.5%) (Table 5). More than half of recipients had “normal weight” (57.5%), 15% perceived their state of health as “bad/very bad”, all of them required some hospital admission during the last year and less than a quarter of the studied recipients smoked (15%) and consumed alcohol (22.5%) (Table 6). Among donors and recipients who drank alcohol, only one recipient, who was a woman, had an alcohol consumption that may be considered dangerous (>20g/day).18,19
General health profile of living kidney donors.
| Average body weight of donors (kg) | 70.01 (SD 12.58) |
| Average height of donors (cm) | 164.3 (SD 8.67) |
| Mean body mass index (BMI) | 25.83 (SD 3.69) |
| Obesity in donors, according to IMC31 | |
| Insufficient weight (<18.5kg/m2) | 0 (0%) |
| Normal weight (18.5–24.9kg/m2) | 16 (40%) |
| Overweight grade I (25–26.9kg/m2) | 9 (22.5%) |
| Overweight grade II (27–29.99kg/m2) | 10 (25%) |
| Obesity type I (30–34.9kg/m2) | 4 (10%) |
| Obesity type II (35–39.9kg/m2) | 1 (2.5%) |
| Perception of health status in the last 12 months | |
| Very good | 18 (45%) |
| Good | 20 (50%) |
| Regular | 2 (5%) |
| Bad, very bad | 0 (0%) |
| Health perception immediately before the donation (from 0 to 10 points) | 8.9 (SD 1.15) |
| Hospital admissions in the last 12 months | |
| No hospital admission | 37 (92.5%) |
| Surgical intervention | 3 (7.5%) |
| Need for urgent healthcare during the last year | |
| No need | 33 (82.5%) |
| Yes they need to go to the emergency service | 7 (17.5%) |
| Various causes | 1 (2.5%) |
| Dental pain/epigastralgia | 1 (2.5%) |
| Traumatology problem | 2 (5%) |
| Accident while working | 1 (2.5%) |
| Anxiety crisis | 1 (2.5%) |
| Urological problem | 1 (2.5%) |
| Tobacco use | |
| Do not smoke | 26 (65%) |
| Yes, they smoke | 14 (35%) |
| 1–10 cigars/day | 7 (17.5%) |
| 11–20 cigars/day | 6 (15%) |
| 21–30 cigars/day | 1 (2.5%) |
| Average time as smoker (months) | 40.5 (SD 45.38) |
| Consumption of alcohol among donors | |
| No alcohol consumption | 25 (62.5%) |
| Yes, they consume alcohol | 15 (37.5%) |
| Daily | 3 (7.5%) |
| Only weekends | 10 (25%) |
| Only working days | 1 (2.5%) |
| Sporadically | 1 (2.5%) |
| Type of alcoholic beverage consumed | |
| Beer | 12 (30%) |
| Wine | 1 (2.5%) |
| Cocktails | 1 (2.5%) |
| Beer and Cocktails | 1 (2.5%) |
| Type of alcohol consumers in donors33 | |
| Abstemios | 25 (62.5%) |
| Low consumption (<10g/day) | 11 (27.5%) |
| Women | 8 (20%) |
| Men | 3 (7.5%) |
| Moderate (10–30g/day) | 4 (10%) |
| Women | 1 (2.5%) |
| Men | 3 (7.5%) |
| High consumption (>30g/day) | 0 (0%) |
General health profile of living kidney receptors.
| Average body weight of donors (kg) | 67.84 (SD 13.68) |
| Average height of donors (cm) | 163.8 (SD 27.42) |
| Mean body mass index (BMI) | 24.05 (SD 4.36) |
| Obesity in recipients, according to IMC31 | |
| Insufficient weight (<18.5kg/m2) | 3 (7.5%) |
| Normal weight (18.5–24.9kg/m2) | 23 (57.5%) |
| Overweight grade I (25–26.9kg/m2) | 3 (7.5%) |
| Overweight grade II (27–29.99kg/m2) | 7 (17.5%) |
| Obesity type I (30–34.9kg/m2) | 3 (7.5%) |
| Obesity type II (35–39.9kg/m2) | 1 (2.5%) |
| Perception of health status in the last 12 months | |
| Very good | 2 (5%) |
| Good | 24 (60%) |
| Regular | 8 (20%) |
| Bad, very bad | 5 (12.5%) |
| Perception of health status in the last 12 months | 1 (2.5%) |
| Health perception immediately before the donation (from 0 to 10 points) | 6.35 (SD 2.2) |
| Hospital admissions in the last 12 months | |
| None | 25 (62.5%) |
| Surgical intervention | 4 (10%) |
| Study or treatment | 3 (7.5%) |
| Problems with the vascular access | 3 (7.5%) |
| Various causes | 5 (12.5%) |
| Urgent healthcare during the last year | |
| Did not need emergency service | 19 (47.5%) |
| They need to go to the emergency service | 21 (52.5%) |
| Various causes | 7 (17.5%) |
| Complications of CKD | 7 (17.5%) |
| Allergies | 2 (5%) |
| Dental pain/epigastralgia | 3 (7.5%) |
| Traumatology | 1 (2.5%) |
| Fever | 1 (2.5%) |
| Tobacco consumption of living kidney receptors | |
| Did not smoke | 34 (85%) |
| Smoker | 6 (15%) |
| Sporadically | 1 (2.5%) |
| 1–5 cigars/day | 4 (10%) |
| 11–20 cigars/day | 1(2.5%) |
| Average time as smoker (months) | 10.40 (SD 7.83) |
| Alcohol consumption of living kidney receptors | |
| No alcohol consumption | 31 (77.5%) |
| Yes, they consume alcohol | 9 (22.5%) |
| Daily | 1 (2.5%) |
| Only weekends | 4 (10%) |
| Only working days | 1 (2.5%) |
| Sporadically | 3 (7.5%) |
| Type of alcoholic drinks consumed by the receptors | |
| Beer | 5 (12.5%) |
| Wine | 3 (7.5%) |
| Cocktail | 1 (2.5%) |
| Type of alcohol consumption33 | |
| Abstemios | 31 (77.5%) |
| Low consumption (<10g/day) | 7 (15%) |
| Women | 1 (2.5%) |
| Men | 6 (15%) |
| Moderate (10–30g/day) | 2 (5%) |
| Women | 2 (5%) |
| Men | 0 (0%) |
| High consumption (>30g/d) | 0 (0%) |
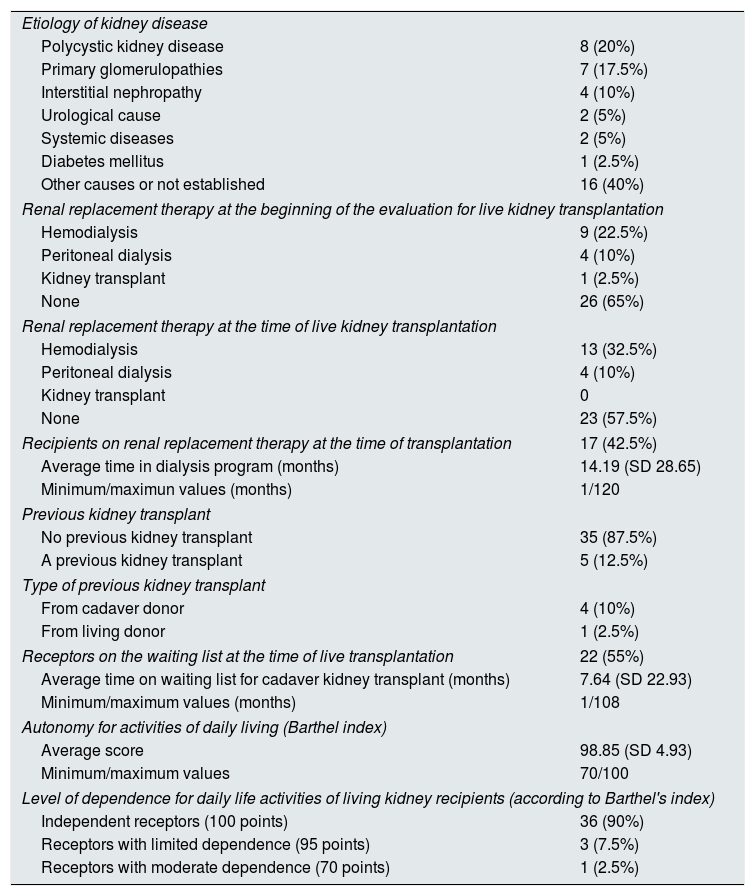
Of the 26 (65%) recipients who had not started renal replacement therapy at the beginning of the study, only 3 (7.5%) had to initiate replacement therapy before transplantation. Thus 23 recipients (57.5%) received an early live kidney transplant (Table 7). Of the 5 (12.5%) recipients who had a previous kidney transplanted (Table 7), only one had a functioning graft at the start of the study. In this case, the renal function of the graft decreased progressively during the study period requiring initiation of renal replacement therapy. Evaluation of recipients autonomy with the scale for activities of daily life (Barthel index), revealed that only 4 (10%) of the total recipients had some degree of dependency for daily life activities (Table 7).
Data on living kidney receptors on chronic kidney disease and its dependence on activities of daily living.
| Etiology of kidney disease | |
| Polycystic kidney disease | 8 (20%) |
| Primary glomerulopathies | 7 (17.5%) |
| Interstitial nephropathy | 4 (10%) |
| Urological cause | 2 (5%) |
| Systemic diseases | 2 (5%) |
| Diabetes mellitus | 1 (2.5%) |
| Other causes or not established | 16 (40%) |
| Renal replacement therapy at the beginning of the evaluation for live kidney transplantation | |
| Hemodialysis | 9 (22.5%) |
| Peritoneal dialysis | 4 (10%) |
| Kidney transplant | 1 (2.5%) |
| None | 26 (65%) |
| Renal replacement therapy at the time of live kidney transplantation | |
| Hemodialysis | 13 (32.5%) |
| Peritoneal dialysis | 4 (10%) |
| Kidney transplant | 0 |
| None | 23 (57.5%) |
| Recipients on renal replacement therapy at the time of transplantation | 17 (42.5%) |
| Average time in dialysis program (months) | 14.19 (SD 28.65) |
| Minimum/maximun values (months) | 1/120 |
| Previous kidney transplant | |
| No previous kidney transplant | 35 (87.5%) |
| A previous kidney transplant | 5 (12.5%) |
| Type of previous kidney transplant | |
| From cadaver donor | 4 (10%) |
| From living donor | 1 (2.5%) |
| Receptors on the waiting list at the time of live transplantation | 22 (55%) |
| Average time on waiting list for cadaver kidney transplant (months) | 7.64 (SD 22.93) |
| Minimum/maximum values (months) | 1/108 |
| Autonomy for activities of daily living (Barthel index) | |
| Average score | 98.85 (SD 4.93) |
| Minimum/maximum values | 70/100 |
| Level of dependence for daily life activities of living kidney recipients (according to Barthel's index) | |
| Independent receptors (100 points) | 36 (90%) |
| Receptors with limited dependence (95 points) | 3 (7.5%) |
| Receptors with moderate dependence (70 points) | 1 (2.5%) |
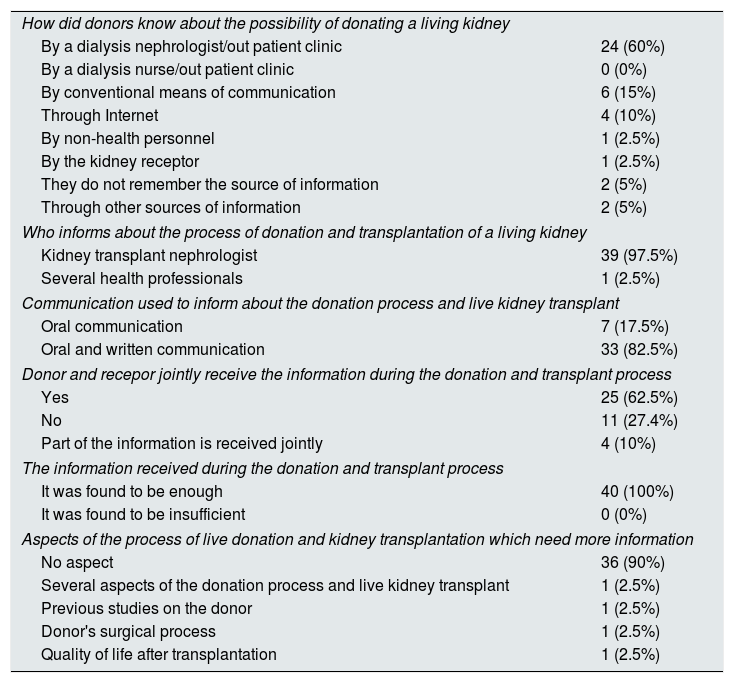
The donors knew about the possibility of donating a kidney mainly from the nephrologist taking care of patients in the dialysis unit or the nephrologist visiting patients in the advanced chronic kidney disease (ACKD) out-patient clinic (60%) and to a lesser extent by the media, both conventional and internet (25%) (Table 8). The recipients were aware of the possibility of a live kidney transplant from the information received by dialysis nephrologist or the ERCA consultation (62.5%) and to a lesser extent by the media (12.5%) (Table 9). It is noteworthy that the dialysis nurses or the ERCA out-patient clinics contributed to announcing the possibility of living donation in only 3 cases (7.5%) (Table 9). All recipients received prior information about the study process of transplantation of a live kidney: The informants were the nephrologist from dialysis or from the ERCA clinics and the kidney transplant nephrologist (57.5 vs. 42.5%) (Table 9).
Information to the living kidney donors about the donation and transplant process.
| How did donors know about the possibility of donating a living kidney | |
| By a dialysis nephrologist/out patient clinic | 24 (60%) |
| By a dialysis nurse/out patient clinic | 0 (0%) |
| By conventional means of communication | 6 (15%) |
| Through Internet | 4 (10%) |
| By non-health personnel | 1 (2.5%) |
| By the kidney receptor | 1 (2.5%) |
| They do not remember the source of information | 2 (5%) |
| Through other sources of information | 2 (5%) |
| Who informs about the process of donation and transplantation of a living kidney | |
| Kidney transplant nephrologist | 39 (97.5%) |
| Several health professionals | 1 (2.5%) |
| Communication used to inform about the donation process and live kidney transplant | |
| Oral communication | 7 (17.5%) |
| Oral and written communication | 33 (82.5%) |
| Donor and recepor jointly receive the information during the donation and transplant process | |
| Yes | 25 (62.5%) |
| No | 11 (27.4%) |
| Part of the information is received jointly | 4 (10%) |
| The information received during the donation and transplant process | |
| It was found to be enough | 40 (100%) |
| It was found to be insufficient | 0 (0%) |
| Aspects of the process of live donation and kidney transplantation which need more information | |
| No aspect | 36 (90%) |
| Several aspects of the donation process and live kidney transplant | 1 (2.5%) |
| Previous studies on the donor | 1 (2.5%) |
| Donor's surgical process | 1 (2.5%) |
| Quality of life after transplantation | 1 (2.5%) |
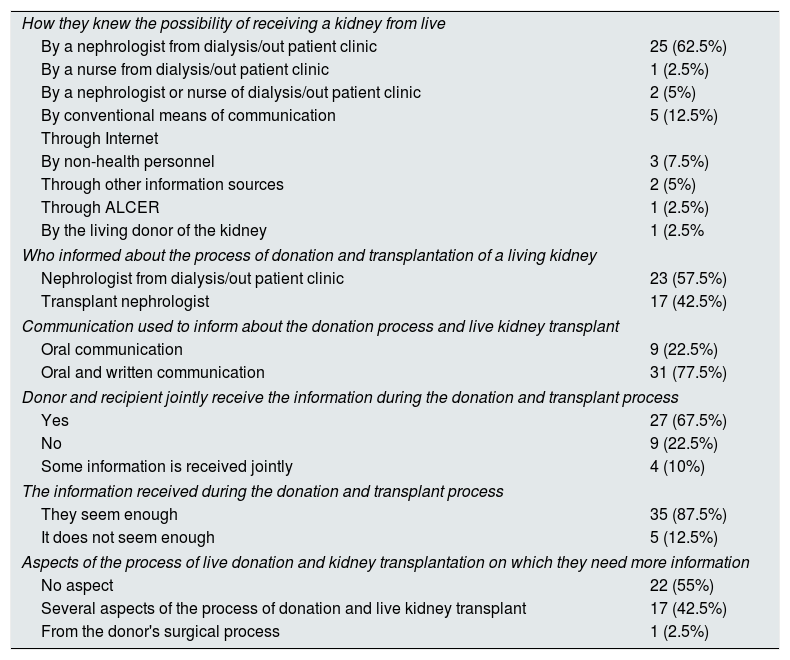
Information to live kidney recipients on the process of donation and transplantation.
| How they knew the possibility of receiving a kidney from live | |
| By a nephrologist from dialysis/out patient clinic | 25 (62.5%) |
| By a nurse from dialysis/out patient clinic | 1 (2.5%) |
| By a nephrologist or nurse of dialysis/out patient clinic | 2 (5%) |
| By conventional means of communication | 5 (12.5%) |
| Through Internet | |
| By non-health personnel | 3 (7.5%) |
| Through other information sources | 2 (5%) |
| Through ALCER | 1 (2.5%) |
| By the living donor of the kidney | 1 (2.5% |
| Who informed about the process of donation and transplantation of a living kidney | |
| Nephrologist from dialysis/out patient clinic | 23 (57.5%) |
| Transplant nephrologist | 17 (42.5%) |
| Communication used to inform about the donation process and live kidney transplant | |
| Oral communication | 9 (22.5%) |
| Oral and written communication | 31 (77.5%) |
| Donor and recipient jointly receive the information during the donation and transplant process | |
| Yes | 27 (67.5%) |
| No | 9 (22.5%) |
| Some information is received jointly | 4 (10%) |
| The information received during the donation and transplant process | |
| They seem enough | 35 (87.5%) |
| It does not seem enough | 5 (12.5%) |
| Aspects of the process of live donation and kidney transplantation on which they need more information | |
| No aspect | 22 (55%) |
| Several aspects of the process of donation and live kidney transplant | 17 (42.5%) |
| From the donor's surgical process | 1 (2.5%) |
All donors and 87.5% of the recipients considered that the information received during the live kidney donation process was sufficient (Tables 8 and 9), although 45% of the recipients stated that they needed more information (Table 9).
DiscussionIn this paper we analyze the characteristics of the information received by living kidney donors and recipients, before and during the process of donation and transplantation; we also analyze its demographic, social and health profile, in the three hospitals involved.
In our investigation, the average age of the kidney donors (49.73 years) and recipients (44 years) were somewhat lower than in the rest of Spain, with donors (51.4 years) and recipients (46.6 years).20 However, our donors were younger than in other European studies, such as that of Timmerman et al.21 (56 years), although our recipients were somewhat older than those studied by Gozdowska et al. (40 years).22
We have detected a gap in the gender of living kidney donation, since almost twice as many women (65%) donated a living kidney (Table 2). These figures are very similar to the rest of Spain (64% of women donors).20 However, they differed from studies conducted in Israel or United States, where women donors barely reach 60%,23,24 or from the Netherlands, in which there is no such gender gap.15,21 Given these results, and that there are studies that identify a more favorable attitude to donate organs in women than men,1,25 some informative and educational strategies should be explored in our area aiming at promote live renal donation by men.
Half of the our donors had completed bachelor and university studies, which differs from the report by Boas et al.23 or from northern Europe,21 where more than 60% of donors have this level of education. This issue should be investigated since a lower educational level has been identified as a barrier for living kidney donors, who may discard the idea of donating organs in life, due to a limited access to information.26,27
Our research also showed that almost all donations of kidneys in life were between relatives (92.5%), within close family members, and 7.5% were from unrelated donors of cross-transplants program (Table 2). These percentages are similar to the rest of Spain with a 89.1% of donations between relatives,20 however they are different from other areas; Taler et al.24 reported a 66% of donations to relatives and in the study by Erim et al. there were up to 97.2% of donations to relatives.28 The percentage of donors and recipients living in the same house was higher in our patients (57.5%) than in other areas (41.7%).15,21 Our study coincides with the general tendency of being the family the main source for people that choose the option of a LDKT, it is reasonable that an individual who needs a kidney seeks help from the members of their family.
Less than half of our donors were employed (Table 3), and in the study by Boas et al.23 78.9% of donors had a work. Our results, that shows fewer employed donors, may be explained by specific socioeconomic factors of our area and also because our donors are mostly women that have less presence in the labor market. In contrast to our data, other studies show more male donors,23 which may explain a greater number of donors being employed. It is striking, that more than half of our recipients (52.5%) did not work at the time of the transplant, because they were retired or incapacitated by disability (Table 3) despite being relatively young (mean of 44 years). These results contrast with even much higher figures of non-active people (89.2%) obtained by Lorenzo-Sellares et al.29 in a population similar to ours, composed of people with advanced chronic kidney disease and in hemodialysis. The consequences of CKD and renal replacement therapy on heath may justify this situation.30
Regarding the BMI, donors and recipients evaluated were “grade-1 overweight” and “normal weight”31 (Tables 5 and 6). This means that most of them were distant from “type-1 obesity”,31 which marks the beginning of a higher risk of nephropathy since “type-1 obesity” is associated, at the long term, with risk factors such as hypertension, diabetes, etc. This justifies maintaining donors and recipients within a normal weight range during the follow-up. Only 4 recipients met the criteria of “tipo I obesity”, and therefore they would be recommended to reduce their weight before transplantion18,19 (Table 6).
Despite the sequelae of CKD and renal replacement therapy, recipients of our study had a “good” perception of their health before transplantation (6.35 out of 10 points) and two thirds of those recipients perceived their health during the last year as “good” or “very good” (Table 6).
Regarding toxic habits, there were more smokers in our donors (35%) than in the general adult Spanish population (24.08%),32 which is clearly higher than the proportion of smokers in recipients before transplantation (15%). Although 37.5% of the donors and 22.5% of the recipients consumed alcohol (Tables 5 and 6), this prevalence is much lower than that observed in the general population, where alcohol consumption is approximately 89% in men and 74% in women. This may be due mainly to the fact that the recipients, due to their CKD, limit alcohol consumption spontaneously or after recomendation.33 Likewise, no donor or recipient had a harmful alcohol consumption (>40.9mg/day) (Tables 5 and 6), so according to the best practice guidelines it was not necessary to advise any donor to abandon or reduce the consumption of alcohol to be able to donate a kidney in life.18,19
It is noteworthy that the majority of recipients (57.5%) received an early live kidney transplant (Table 7), so they received the optimal therapeutic option for terminal renal failure34 indicating that the study centers consider the possibility of early live transplantation from beginning of CKD. However, the recipients who were on dialysis at the time of transplantation had been for an average of 14.19 months on dialysis, which should be taking into consideration since graft survival is significantly better in recipients that were on dialysis for less than 6 months.34 It is also observed in our study that the proportion of recipients independent for daily activities (90%) (Table 6) is greater than in populations similar to ours, where 81.5% of patients with advanced chronic kidney disease and 69.8 of dialysis patients are capable of self-care.29
Since the nephrologist is responsible for monitoring the patient with CKD, it seems reasonable that the nephrologist inform about the living kidney donation and the process that has to be followed (Tables 8 and 9). However, the joint and complementary action of nephrologists and nurses to inform and promote the possibility of LDKT, may contribute to improve the development and the process of these LDKT.
The vast majority of recipients (87.5%) considered that the information received during the donation and live kidney transplant process was sufficient, but almost half of them would have desired more information (45%) (Table 9). This demand for additional information may imply that there is a lack of knowledge in these patients and insufficient public awareness of the process of renal donation in life.27
Consequently, to improve the LDKT process, the current evaluation procedures and pre-donation information should be reconsidered and adapted to the educational and level of knowledge of candidates and families. The decision to donate should be made only after being well informed with realistic expectations about the results of transplantation in the recipient and, the potential consequences in the donor including possible impact on personal relationships.35 The manner in which health professionals inform and educate potential kidney donors and recipients has long-term implications on the psychosocial and health outcomes of living donors.2 Likewise, in order to improve the LDKT process, novel informative and educational strategies should be implemented,35 focusing especially on potential male donors of our environment, on the possibility of unrelated donation and actively integrating other health professionals in the task of educating and increasing the awareness about kidney donation in life.
As a strength of our research, it is worth mentioning that this is the first time that the information received by living kidney donors and recipients of and its social and health profile has been evaluated in our environment. During the 15 months duration of the study, all the donors and kidney recipients available were evaluated which accounted for 85.1% of the total population (Table 1), with only two refusals to participate in the study (5%). By contrast, our study has the limitations of a descriptive study with a limited number of subjects since living donation depends on the social and cultural characteristics of the area where is being developed. Despite these limitations, we think that our study can be used to improve the information about the process of living kidney donation and transplantation and to establish new lines of research, which should contemplate those candidates that were evaluated, but at the end, the fail to donate.
In short, it can be concluded that since the information provided has a direct impact on the results of the LDKT programs and that a significant number of recipients demand for more information, the evaluation and information processes should be updated to increase donors and living kidney recipients. Renal donations in life in our area are mostly to relatives, and despite the limitations to extrapolate our study, it is observed that the sociodemographic profiles obtained in the donors and recipients studied tend to approximate those of the whole country and to differ from studies obtained in other geographical areas.
Regarding employment and economic profile, a high percentage of kidney donors and recipients do not have a remunerated job, although this inactivity would be compensated with some retirement or disability benefit and would not have an impact on their economy, since almost all of them have some source of income in their family.
Renal donors and recipients care for elderly people in their families in percentages much higher than in the Spanish population and the great majority of these donors and recipients do not have work overload.
In relation to the health profile, the tendency to be over weighted is the only negative aspect identified in the kidney donors and recipients. It should be highlighted that more than half recipients receive an anticipated LDKT and that they are independent for daily activities.
Conflicts of interestThe authors declare to have no conflicts of interest.
Please cite this article as: Calvo-Calvo M-Á, Morgado Almenara I, Gentil Govantes MÁ, Moreno Rodríguez A, Puertas Cruz T, García Álvarez T, et al. Perfil sociosanitario e información a donantes y receptores renales de vivo en tres hospitales andaluces. Nefrologia. 2018;38:304–314.