A pesar de los progresos en el tratamiento farmacológico de la hipertensión arterial (HTA) y el empleo de múltiples fármacos antihipertensivos, un pequeño pero significativo porcentaje de los pacientes con HTA refractaria severa verdadera continúa sin alcanzar su objetivo de control tensional. En estos casos, la denervación simpática renal (DNSR) parece mostrarse como un método seguro y eficaz para aquellos pacientes hipertensos severos refractarios al tratamiento farmacológico múltiple. Presentamos el caso de un paciente de 52 años de edad diagnosticado de HTA esencial refractaria a tratamiento con 7 fármacos antihipertensivos. Tras 10 ingresos hospitalarios sin conseguir un adecuado control de las cifras de presión arterial, decidimos plantear la DNSR como coadyuvante al tratamiento médico. El procedimiento se realizó sin complicaciones a corto y medio plazo, consiguiéndose una mejoría significativa de las cifras tensionales, con el objetivo de disminuir su riesgo vascular global.
Despite advances in the pharmacological treatment of arterial hypertension (AHT) and the use of multiple antihypertensive drugs, a small but significant percentage of true severe refractory arterial hypertension patients are still not reaching their target blood pressure. In these cases, renal sympathetic denervation (RSD) seems to be a safe and effective method for severe hypertensive patients who are resistant to multiple drug treatment. We present the case of a 52-year-old patient diagnosed with essential hypertension, resistant to treatment with seven antihypertensive drugs. After 10 hospitalisations without achieving adequate blood pressure control, we decided to propose renal sympathetic denervation as an addition to medical treatment. The procedure was performed without complications in the short to medium-long term, achieving a significant improvement in blood pressure with the intention of reducing overall vascular risk.
INTRODUCTION
Resistant or refractory arterial hypertension (AHT) is defined as persistent blood pressure (BP) levels >140/90mm Hg in outpatient clinics, despite the application of hygienic and dietetic measures and good compliance with treatment of at least three anti-hypertensive drugs (one of which is a diuretic).1,2 This definition includes the existence of organ damage indicators, reception of adequate treatment, and confirmed inadequate control of BP as determined by ambulatory BP measurement (ABPM)/24 hours.3,4
Approximately 2% to 5% of these hypertensive patients refractory to treatment with high vascular risk cannot be properly controlled, despite the use of combinations of multiple anti-hypertensive drugs at appropriate doses.
In recent years, the gamut of complementary non-pharmacological treatment alternatives has expanded. One of these alternatives, endovascular sympathetic denervation of the afferent and efferent renal sympathetic nerves (renal sympathetic denervation [RSDN]),5 presents a rational basis for treating refractory AHT6 and significantly contributes to increasing the effects of anti-hypertensive medication and improves blood pressure control in these patients.7,8 This makes RSDN a cost-effective and appropriate therapeutic measure.9
Here, we present the case of a patient diagnosed with resistant AHT, treated with seven different anti-hypertensive drugs, and with a registry of 24-hour BP measurements >140/90mm Hg. Due to the inability to reach target BP levels, radiofrequency ablation RSDN was administered.
CASE REPORT
Our patient was a 55-year-old male who sought care for the first time in our AHT and vascular risk unit due to poor control of BP levels in March 2010. Relevant family history included: mother on renal replacement therapy due to chronic renal failure of unknown origin, and known AHT in the patient that was first observed incidentally in a routine medical examination and had been followed by primary care since 2002. The patient was a smoker until February 2010, but reported that he did not ingest major quantities of salt, alcoholic beverages, or other substances or drugs that could interfere with BP or anti-hypertensive medications. An initial physical examination revealed a BP of 190/110 mm Hg, and a mean BP over 24 hours (ABPM) of 169/109mm Hg, with a non-dipper profile.10
Complementary tests revealed: haematocrit: 39.6%; haemoglobin: 13.1g/dl; glycaemia: 102mg/dl; creatinine: 0.9mg/dl; uric acid: 5.9mg/dl; total cholesterol: 149mg/dl; triglycerides: 250mg/dl; HDL cholesterol: 23mg/dl; LDL cholesterol: 104mg/dl; sodium: 146mmol/l; and potassium: 4.1mmol/l. Urinary sediments were normal, with microalbuminuria at 42mg/24 hours, and no toxic substances present. Other laboratory results included: thyrotropin-releasing hormone (TRS): 1.43mIU/ml; plasma renin activity (PRA): 0.26ng/ml/min; aldosterone: 264pg/ml; and catecholamine levels within normal range. A renal Doppler-ultrasound was normal, and an electrocardiogram revealed sinus rhythm with signs of left ventricular hypertrophy.
Since the PRA/aldosterone ratio was >100, we started treatment with spironolactone, which was not very effective. Two months later (June 2010), the patient required the prescription of 5 anti-hypertensive drugs, despite which the treatment objectives were still not reached. As such, he was hospitalised for the control of BP, and to evaluate compliance with treatment and the possibility of secondary causes. After an exhaustive evaluation that included new measurements of specific hormone levels, with catheterisation of the renal arteries and scintigraphy with metaiodobenzylguanidine (MIBG) and I-cholesterol, secondary causes were ruled out.
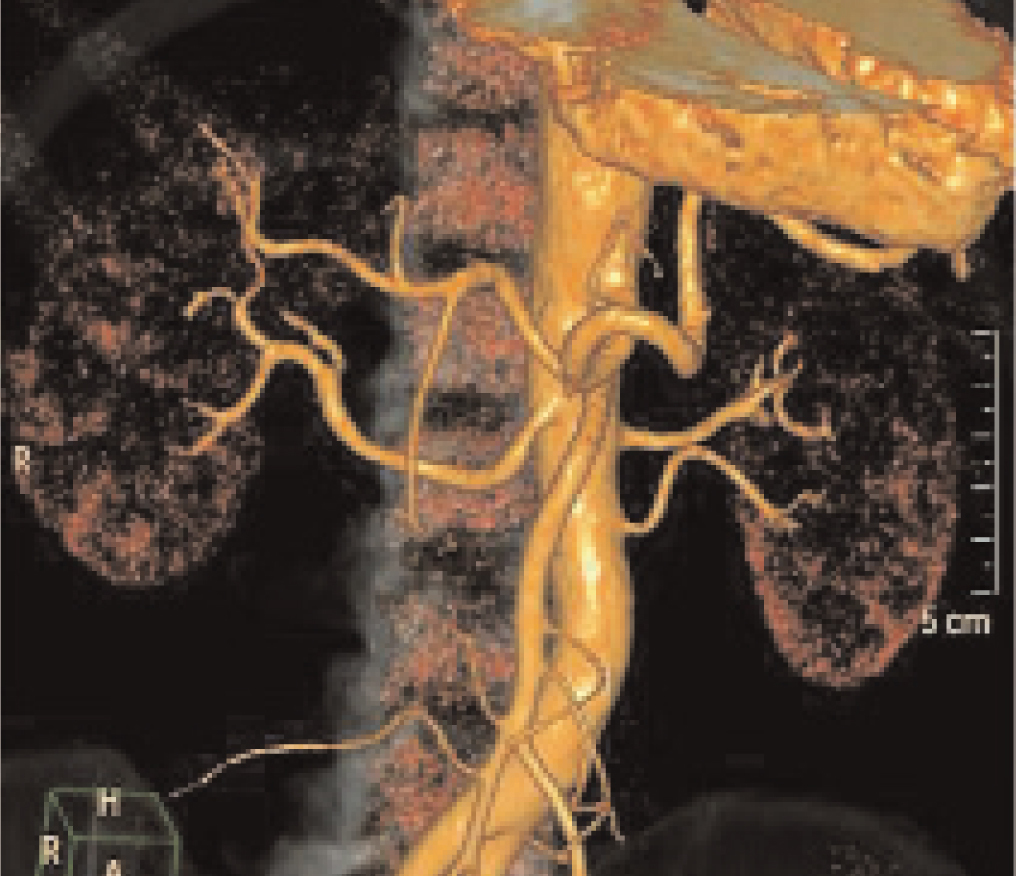
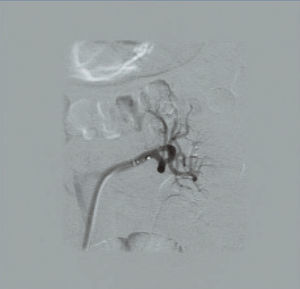
Before deciding on administering RSDN, the patient required a total of 10 hospitalisations due to hypertensive emergencies, in which resistance to treatment was again confirmed. Given the inability to control BP levels, and after ruling out possible contraindications for administering RSDN (Figure 1),2,3 in January 2012, RSDN was applied through a femoral approach after prior monitoring and premedication, using the recommended protocols. At this point, the patient had grade 3 AHT with signs of target organ damage: left ventricular hypertrophy (LVH), grade 2 hypertensive retinopathy, and microalbuminuria, and was receiving treatment with: telmisartan/amlodipine at 80/10mg 1/12 hours, aliskiren at 300 mg 1/24 hours, eplerenone at 50mg 1/12 hours, doxazosin at 8mg 1/8 hours, hydrochlorothiazide at 25mg 1/24 hours, and carvedilol at 25mg 1/12 hours.
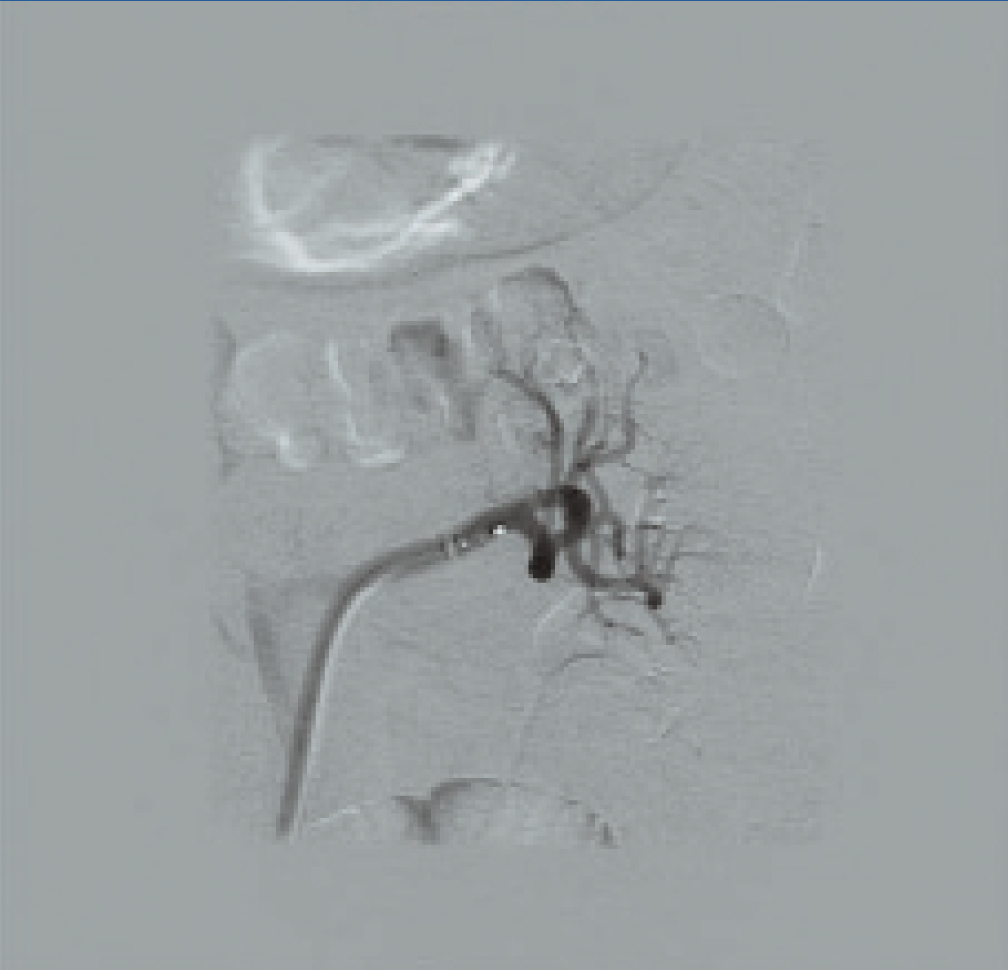
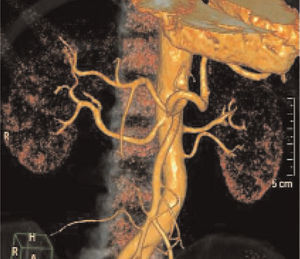
RSDN was applied without complication (Figure 2); we decided not to treat the left inferior renal polar artery, since the minimum required diameter was not reached, and we observed a left renal artery spasm in the immediate post-procedure radiological control (Figure 3), which was resolved by injecting nitroglycerin, and for which we decided to start anti-platelet treatment with triflusal.
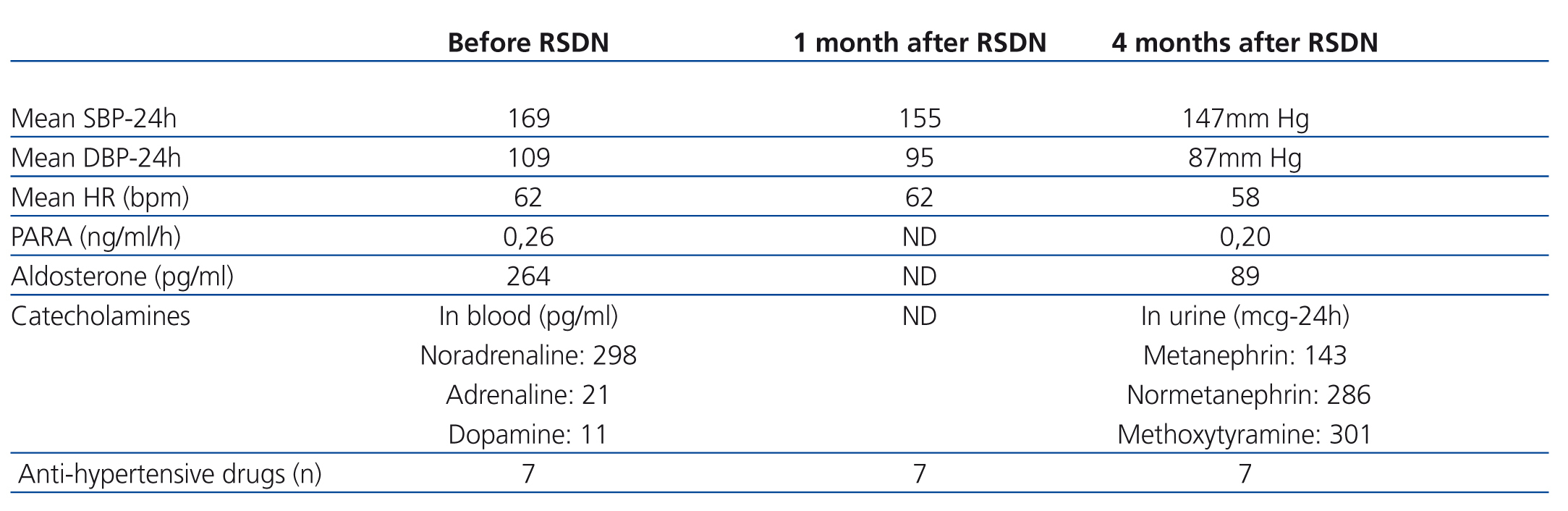
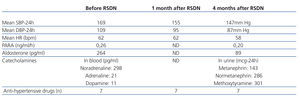
The evolution of BP values following the procedure is described in the Table. Three months after the procedure, mean 24-hour systolic and diastolic BP values had decreased by 22mm Hg, with no significant modification in heart rate. No immediate complications were produced, and the patient has not required further hospitalisations.
DISCUSSION
AHT refractory to medical treatment implies a global increase in cardiovascular risk, incurring greater morbidity and mortality rates and economic costs.1,2 In the small percentage of these patients in which BP control is not reached using anti-hypertensive treatment, RSDN can be a safe and effective treatment option. However, the application of this technique must be preceded by an exhaustive confirmation of true resistance to treatment (through ABPM and evaluation of compliance with treatment) and the presence of target organ damage.3 In this sense, our patient was an appropriate candidate for this procedure, as he had ABPM-confirmed grade 3 AHT and target organ damage (hypertensive retinopathy, LVH, and microalbuminuria), with 7 anti-hypertensive drugs, 10 hospitalisations, and yet still deficient control of BP values.
In the editorial of this issue of Nefrología, the rational basis for the use of RSDN as a treatment alternative in severe cases of refractory hypertension is concisely described.3 In short, the concrete indications for this procedure involve sympathetic hyperactivity patients that decisively contributes to the maintenance of high blood pressure values and the production of target organ damage.
The endovascular procedure is not particularly difficult, although it always requires prior evaluation of renal anatomy, since the probability of anatomical contraindications is high (10%-15%), given the multiple possible renal anatomical variants and the possibility of stenosis, which would represent contraindications.2,3 In our patient, the left inferior renal polar artery was left untreated due to a diameter <4mm. Apart from these considerations, the technique offers no special difficulty, as in our case, with only minimal rates of secondary side effects (<5%),2,7,8 usually in the form of transitory local pain when the procedure is carried out.5
The results obtained in our case (mean decrease in BP of 22mm Hg) reflect the results from the Simplicity HTN-17 and Simplicity HTN-28 studies, where the mean reduction in BP was similar, and even increases over time during follow-up.2,3 We still have yet to confirm whether the decrease in BP is associated with regression of target organ damage.
To conclude, larger randomised studies with longer follow-up periods are needed to address several unanswered questions regarding this technique.3 However, RSDN appears to be an effective and safe method for producing better control of BP in severe cases of hypertension refractory to multiple pharmacological treatments at appropriate doses.
Conflicts of interest
The authors have no conflicts of interest to declare.
Figure 1. Angio-CAT scan before RSDN. Left inferior renal polar artery
Figure 2. Left RSDN
Figure 3. Left renal artery spasm following the procedure
Table 1. Evolution of clinical and laboratory parameters following the procedure