Peritoneal dialysis (PD) is a treatment option in patients with chronic kidney disease (CKD), offering multiple advantages over haemodialysis, although it is not without complications.1 Among these, peritoneal fluid leak (PFL) to other compartments stands out. Despite being the technique of choice for diagnosing leaks, peritoneal scintigraphy (PS) has fallen into disuse, probably due to lack of knowledge on the part of emerging specialists and the availability of other techniques.2
We present a series of images of the most representative cases of all the PS procedures performed at our hospital, from 2014 to the present, where we have performed a total of 19 procedures in 16 PD patients with CKD and suspected PFL, using the acquisition of static images in supine decubitus of the thoracic and abdominal/pelvic region after intraperitoneal administration of [99mTc] Tc-nanocolloid in the dialysis solution, post-Trendelenburg of 5 min duration, and after evacuation of the labelled peritoneal solution, approximately 60 min post-administration. Single-photon emission computed tomography with computed tomography (SPECT-CT) was performed in three of them.
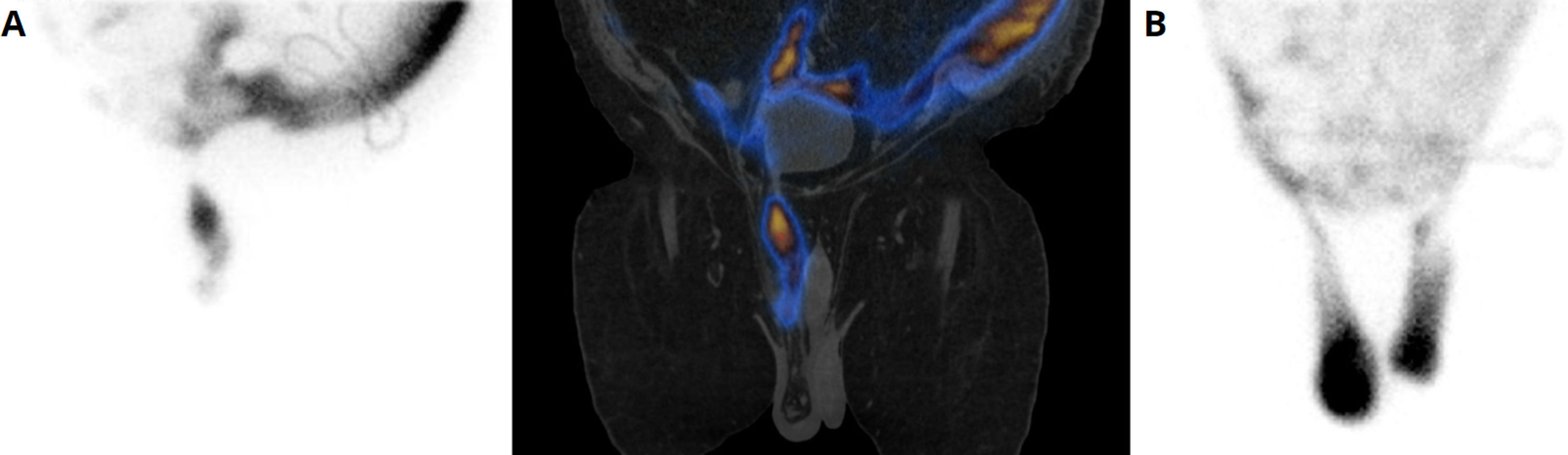
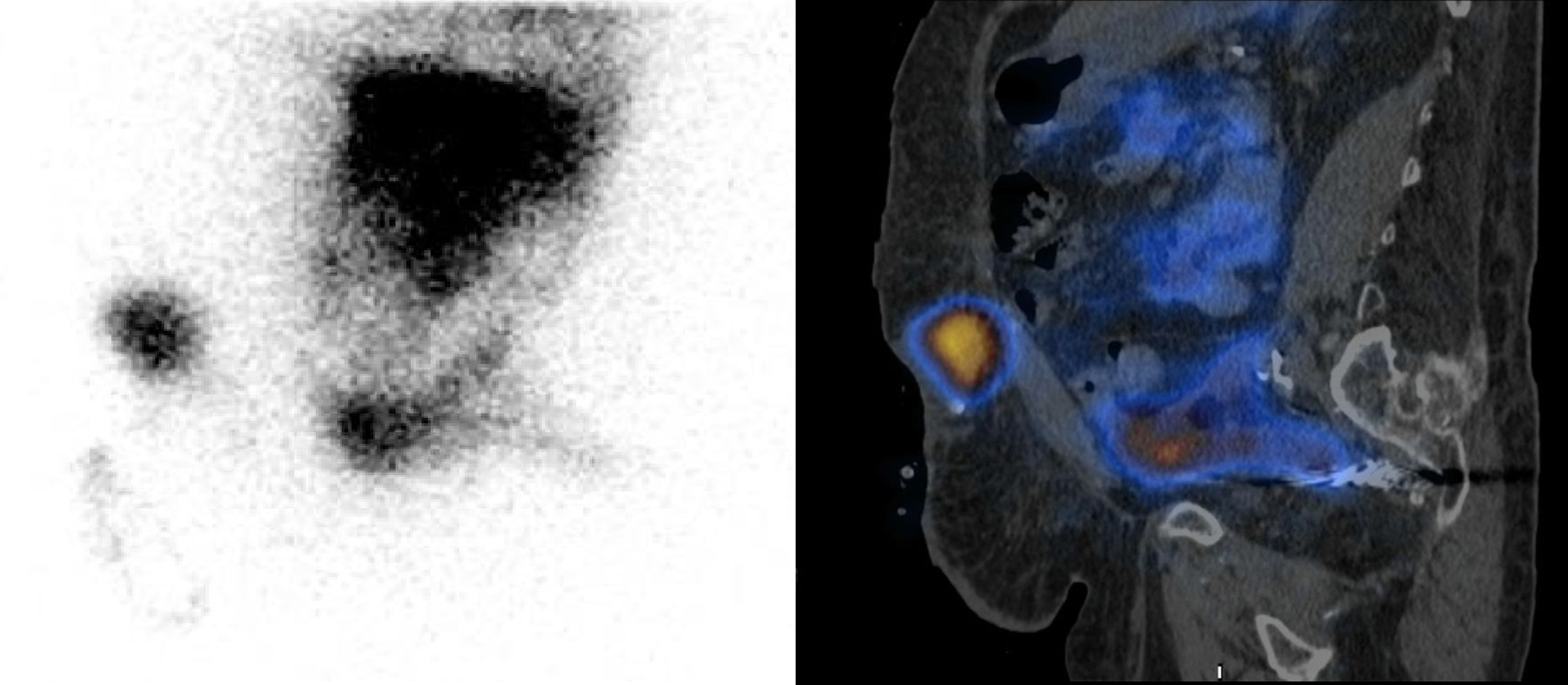
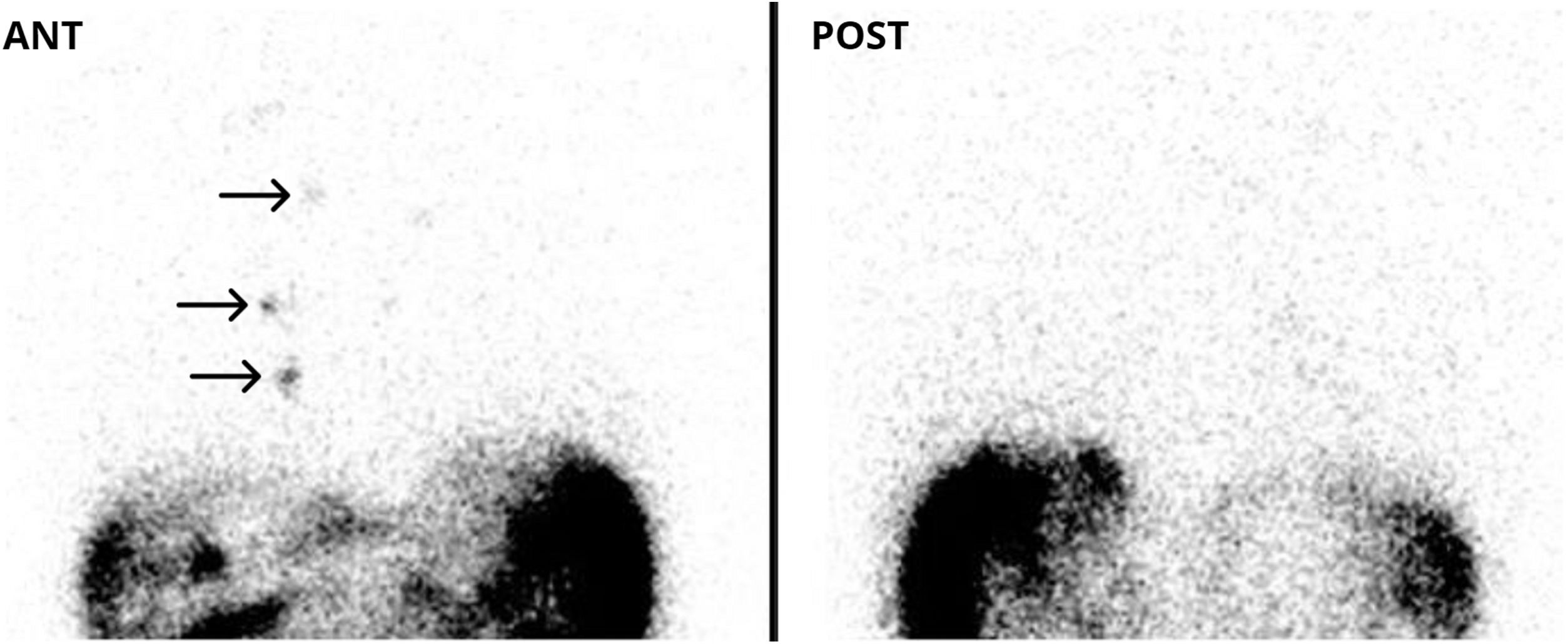
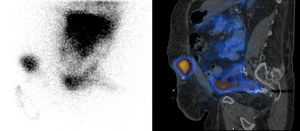
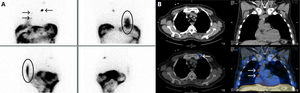
A total of 13 PFLs were diagnosed: two inguinal (Fig. 1), one subcutaneous (Fig. 2) and 11 pleural (Fig. 3). Of these, 53% were kept on peritoneal repose for 3–4 weeks, requiring temporary haemodialysis in a few cases, as well as radiographic and analytical follow-up tests, with subsequent resumption of PD (three patients required pleurodesis), while 38% of them made a direct transition to haemodialysis PFL was not diagnosed in 3% and they continued PD without presenting other complications. Incidentally, migration of the tracer to thoracic/mediastinal lymph nodes was observed in six of the 16 patients (“hotspots”), with no clear pathological significance (Fig. 3).
A: Passage of the tracer to the base of the posterior right hemithorax, diagnosis of pleuroperitoneal communication (ovals) with visualisation of “hotspots” in the upper left thoracic region and right hemithorax (arrows). B: SPECT-CT where it is verified that all the foci described in planar images/“hotspots” correspond to thoracic/mediastinal lymph nodes.
The appearance of these aforementioned mediastinal lymph node “hotspots”, not previously reported in other publications, does not seem to be associated with PFL in the pleural cavity per se, since this event was also seen in patients without a leak (Fig. 4). Therefore, these findings establish that the appearance of mediastinal foci constitutes a possible event that can be considered as a misleading image or “pitfall” of PS with [99mTc] Tc-nanocolloid, which is probably attributed, as in other procedures where this type of tracers are also used, to the injection technique thereof.
In our experience, PS has been shown to be a simple, highly effective diagnostic tool with good accuracy for the diagnosis of PFL, allowing PD therapy to be adapted or stopped, positively impacting the quality of life of CKD patients on dialysis.