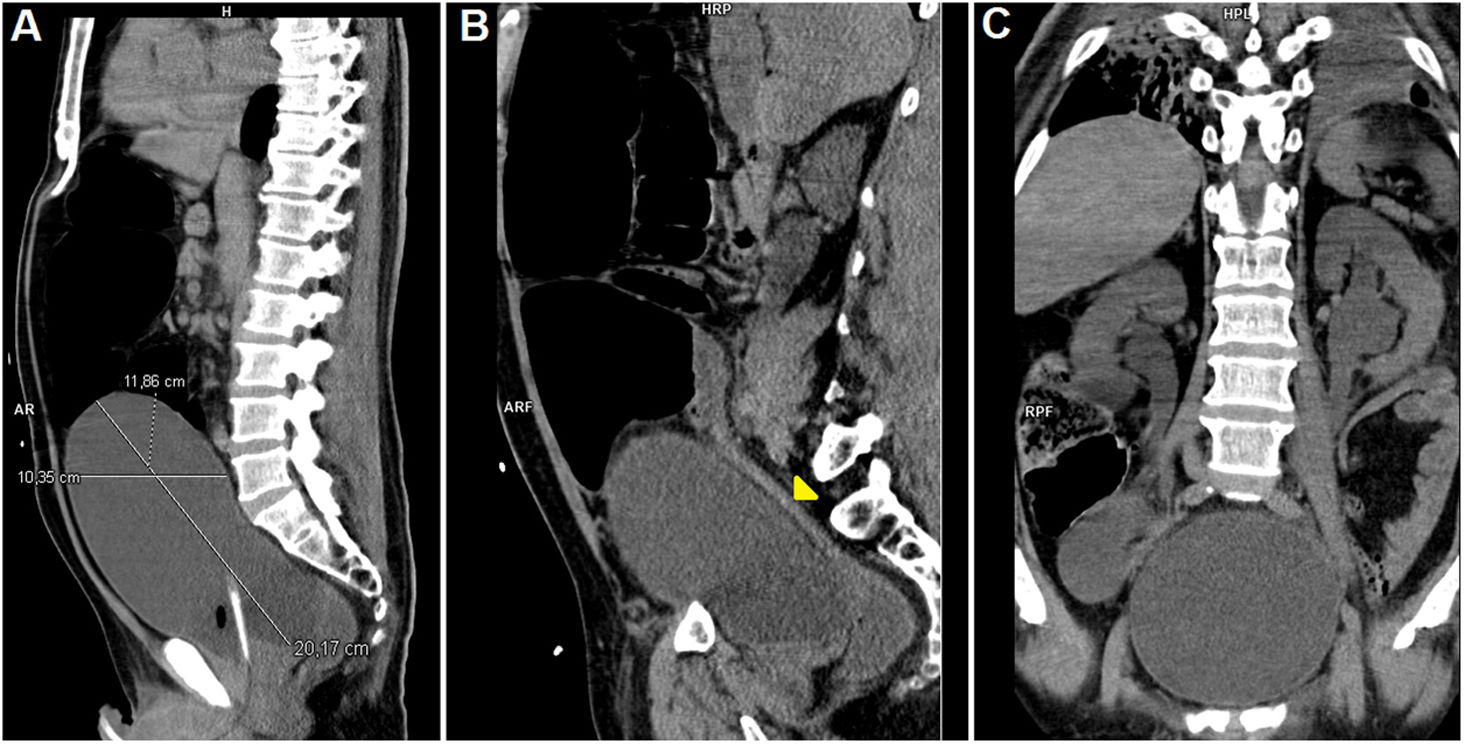
A 72-year-old male with no previous medical history or treatment came to the emergency department after two weeks of symptoms of cough, dyspnoea, asthenia, abdominal pain, and oliguria. He was dehydrated, afebrile, normotensive, and presented signs of an acute abdomen. Laboratory tests revealed acute kidney failure with a serum creatinine of 11.3 mg/dl and urea of 354 mg/dl, metabolic acidosis, elevation of the anion gap that presented (venous sample, so the respiratory compensation was not estimable: pH 7.24, bicarbonate 16 mmol/l and carbon dioxide 39 mmHg, anion gap 22 mEq/l), lactate 2 mmol/l and negative urine ketones. There was no ingestion of toxins or any type of medication. Routine d-lactic acid was not requested. The rest of the lytes were: potassium 4.1 mmol/l, sodium 127 mmol/l, chloride 89 mmol/l, phosphorus 12.2 mg/dl and calcium corrected for albumin was 10.6 mg/dl. Lymphopenia was 500 × 103/l, C-reactive protein (CRP) 134 mg/l and D-dimer > 80,000 g/l. Prior to admission, laboratory tests were normal. Magnesium, requested 48 h following admission, was normal. There was no ingestion of toxins and did not receive any type of medication. A non-contrast-enhanced abdominal computed tomography (CT) scan revealed a significant bladder dilation of 20.2 × 10.3 × 11.8 cm (Fig. 1A) with bilateral hydronephrosis. The considerable bladder distension compressed the rectum and sigmoid colon against the sacrum (Fig. 1B) causing an obstructive ileus with distension of the entire colon. No wall thickening or irregularity of the colon section was observed. The patient did not report any previous history of urological or G.I. abnormalities prior to admission.
A) Sagittal multiplanar reconstruction (MPR) revealing the dimensions of the bladder. We can observe the loops of the large intestine dilated above the bladder. There was no associated dilation of the small intestine. We observed an anterior interposition of the colonic loops to the liver (Chilaiditi syndrome). B) Sagittal MPR revealing an abrupt change in the calibre of the sigmoid colon (yellow arrowhead). C) Axial MPR identifying pyeloureteral dilation compatible with grade III hydronephrosis.
For all these reasons, the patient was diagnosed with acute obstructive renal failure, likely of infravesical origin with grade III bilateral hydronephrosis (Fig. 1C) and intestinal obstruction secondary to the compression exerted by the bladder. After bladder catheterisation, fluid and electrolyte replacement, and initiation of treatment with tamsulosin, renal function returned to normal. In addition, COVID-19 pneumonia was diagnosed and treated with azithromycin and hydroxychloroquine. These are two common pathologies (acute obstructive renal failure and intestinal obstruction), but they rarely appear together, having a simple and non-surgical treatment. In this case, the hydroelectrolytic disorders did not justify the episode of obstructive renal failure, and it was attributed to a possible prostatic origin. On discharge, the patient was referred to urology for complete evaluation with imaging and urodynamic studies. The bladder distension obtained is striking, suggesting that, apart from the possibility of an underlying prostate pathology, there may be also some type of co-existing bladder dysfunction. It is important to highlight that the SARS-CoV-2 epidemiological situation made the patient to come late to the hospital emergency room, with the identification of a case, both remarkable and uncommon, of advanced obstructive renal failure with the secondary intestinal complication.
FundingThis study did not receive any funding.
Conflicts of interestThe authors have no conflicts of interest to declare.