Dialysis fluid in the peritoneal cavity increases intraperitoneal pressure (IPP).1 This increase in pressure may lead to complications in the abdominal wall, particularly hernias. It may also contribute to the failure of ultrafiltration, and it may be cause of abandonment of the technique.
The aim of the study was to assess the frequency of hernias, identify the risk factors for the development of hernia and to determine whether or not they lead to failure of the dialysis technique.
We studied prevalent patients on peritoneal dialysis at day 01 August 2015 in the Complejo Asistencial Universitario de Leon, in Leon, Spain. We analysed the variables: age; gender; type; time on dialysis; presence of polycystic kidney disease; history of abdominal surgery; diagnosis and repair of hernia before starting dialysis; anthropometric parameters (body mass index (BMI), fat tissue index (FTI) and lean tissue index (LTI) measured by bioimpedance); daytime/sc volume; nocturnal/sc volume; residual volume; and IPP and ultrafiltration measured by a peritoneal equilibration test. We compared the group of patient with hernias with the group without hernias. Continuous variables were expressed as mean and standard deviation; in the case of discrete variables, absolute frequencies and percentages are provided. The association between qualitative variables was evaluated with the chi-square test and quantitative variables using Student's 2-tailed t-test. For the comparisons, the tests were considered to be significant when p<0.05. SPSS® statistical software for Windows was used.
We analysed 44 patients, 27 males (61.4%), 17 females (38.6%), 28 on continuous ambulatory peritoneal dialysis (CAPD) (63.6%), the average time on dialysis 27.63±19.1 months, 3 PKD (6.8%), 22 had a history of abdominal surgery (50%) and 8 (18.8%) had a hernia repair prior to starting dialysis.
There were 8 hernias (18.8%), 3 umbilical and 5 inguinal, 7 in males (87.5%), 50% on CAPD. In 6 patients, the prescription was changed to automated peritoneal dialysis (APD) with a dry day, one patient remained on CAPD with reduction of volume/sc; with these prescription changes, 6 (75%) patients remained asymptomatic and without complications such as incarceration or strangulation. One hernia (12.5%) was repaired surgically with mesh implant, and the patient was switched temporarily to haemodialysis due to the presence of persistent pain.
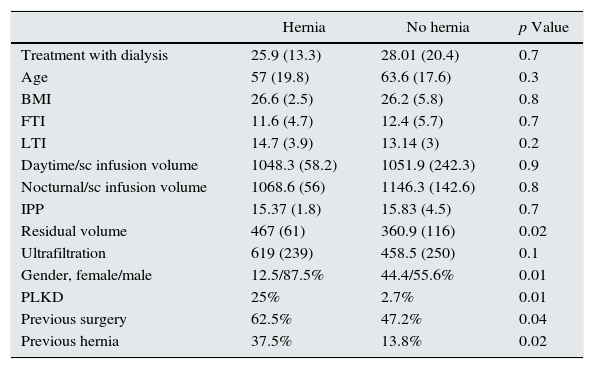
There were no differences between patients with hernias or without hernias in the variables age, dialysis modality, BMI, FTI, LTI, time on dialysis, volume/sc, ultrafiltration and IPP. In contrast, there was greater residual volume in the patients with hernias: 467±61.8 compared to 360.9±116ml (p 0.017). There were more subjects with PKD and more with hernias and previous abdominal surgery in the group with hernias (p<0.05) (Table 1). 100% of the group with hernias had IPP>13cm/H2O.
Comparison between patients with and without hernias.
| Hernia | No hernia | p Value | |
|---|---|---|---|
| Treatment with dialysis | 25.9 (13.3) | 28.01 (20.4) | 0.7 |
| Age | 57 (19.8) | 63.6 (17.6) | 0.3 |
| BMI | 26.6 (2.5) | 26.2 (5.8) | 0.8 |
| FTI | 11.6 (4.7) | 12.4 (5.7) | 0.7 |
| LTI | 14.7 (3.9) | 13.14 (3) | 0.2 |
| Daytime/sc infusion volume | 1048.3 (58.2) | 1051.9 (242.3) | 0.9 |
| Nocturnal/sc infusion volume | 1068.6 (56) | 1146.3 (142.6) | 0.8 |
| IPP | 15.37 (1.8) | 15.83 (4.5) | 0.7 |
| Residual volume | 467 (61) | 360.9 (116) | 0.02 |
| Ultrafiltration | 619 (239) | 458.5 (250) | 0.1 |
| Gender, female/male | 12.5/87.5% | 44.4/55.6% | 0.01 |
| PLKD | 25% | 2.7% | 0.01 |
| Previous surgery | 62.5% | 47.2% | 0.04 |
| Previous hernia | 37.5% | 13.8% | 0.02 |
FTI: fat tissue index; BMI: body mass index; LTI: lean tissue index; IPP: intraperitoneal pressure; PLKD: polycystic liver and kidney disease.
Data are expressed as mean plus standard deviation.
We analysed the 34 patients who had IPP>13cm/H2O and compared them to those with lower IPP. Time on dialysis was 31.47±18 vs 14.55±15 months (p 0.012), BMI 27.68±4 vs 21.62±46kg/m2 (p 0.001), FTI 13.6±5 vs 7.6±4 (p 0.02), daytime/sc infusion volume 1103.12±132 vs 875±349ml/m2 (p 0.003) and residual volume 411.11±94 vs 275.14±125ml (p 0.001). We found no significant differences in the rest of the variables, including ultrafiltration.
Frequency of hernias vary in the range of 12–37% in different studies,2 similar to that found in our series, and there is no reason why a hernia should influence the continuing success or failure of the technique.3 No patient in our series has had to abandon the technique so far, although it has been needed to increase the use of cycler with dry day.
As in other studies, neither IPP or infusion volume appear to predict the development of abdominal hernias.1,4 A positive association has however been described with being elderly, polycystic kidney disease, BMI,5 prolonged time on peritoneal dialysis6 and previous hernias.7 There is a negative association with being female.6
We were unable to demonstrate any association with age or a lower LTI, perhaps because of the small sample size.
We can conclude that 18.8% of our patients developed an abdominal hernia as a complication; nevertheless 100% were able to continue with their dialysis technique.
The risk factors in our series were: being male; polycystic kidney disease; having had previous hernias; previous abdominal surgery; and greater residual volume.
IPP>13cm/H2O was associated with more time on dialysis, higher BMI, FTI and daytime volume/sc and greater residual volume.
Since 100% of these complications occur with IPP>13cm/H2O, we recommend adjusting the dialysis prescription to not exceed these limits, especially in patients with the risk factors described.
We believe that our finding of residual volume being a risk factor for hernias is a new observation; the tolerated pressure limit could be reduced to 13cm/H2O in patients at high risk of developing mechanical problems affecting the abdominal wall.
Please cite this article as: Sastre A, González-Arregoces J, Romainoik I, Mariño S, Lucas C, Monfá E, et al. Factores de riesgo asociados a hernias en diálisis peritoneal. Nefrologia. 2016;36:567–568.