La rabdomiólisis es un síndrome producido por la lesión del músculo estriado con liberación al torrente sanguíneo de gran cantidad de productos intracelulares. Es frecuente el desarrollo de fracaso renal agudo que, además, constituye el principal factor de morbimortalidad en estos pacientes. Entre las causas más frecuentes destacan los traumatismos, la compresión muscular o la realización de ejercicio físico intenso. Son casos que se reconocen fácilmente al realizar una adecuada historia clínica. Sin embargo, en ausencia de un desencadenante claro, el diagnóstico es difícil y suele requerir un alto grado de sospecha. Deben investigarse consumo de drogas y fármacos, infecciones, trastornos electrolíticos y determinados defectos enzimáticos en los que el músculo es incapaz de utilizar la energía disponible. Presentamos dos casos de fracaso renal agudo debido a rabdomiólisis por miopatías metabólicas, secundarios a déficit de carnitina-palmitoil-transferasa en un caso y de miofosforilasa en el otro. Se revisa esta enfermedad insistiendo en las formas de presentación y medidas preventivas.
Rhabdomyolysis is a syndrome characterized by injure of skeletal muscle with the release of intracellular constituents into the circulation. Acute renal failure is a common complication and is the leading cause of morbidity and mortality in these patients. The most common aetiology is traumatisms, muscle compressions and extreme exertions. Most commonly, the cause of rhabdomyolysis is evident from the careful clinical history. Nevertheless, when the precipitant is not obvious the diagnosis is difficult and a raised clinical suspicion is required. We should investigate used medication or drugs, infections, electrolyte abnormalities and a number of inherited enzyme deficiencies, in which cases the muscle is unable to use available energy. We report two clinical cases of acute renal failure due to rhabdomyolysis by metabolic myopathies due to a carnitine palmitoyltransferase deficiency on the one hand and by myophosphorylase deficiency on the other. We describe their clinical features and progress.
INTRODUCTION
The Metabolic Myopathies (MM) comprise a heterogeneous group of genetic disorders that compromise the glycogen synthase pathway, lipids, purines or the mitochondrial metabolism resulting in muscle tissue unable to produce the necessary energy. Even though clinical symptoms vary according to the type of problem, it is also verified exercise intolerance and myalgia besides exertional rhabdomyolysis. In general, these are not usually the cause of Acute Renal Failure (ARF), but frequent episodes of rhabdomyolysis during a childhood with moderate physical activity should raise suspicion. To confirm, it is required to employ molecular biology techniques to determine the effect from the enzyme.
Two cases of myopathy due to enzyme deficiency that resulted in ARF due to rhabdomyolysis are presented.
CASE 1
A 30-year-old man, who at the age of 14 suffered from episodes of acute myalgia and from dark urine due to prolonged physical exercise (walking 6-7 kilometres.) No family member showed similar episodes.
After four years of no symptoms, one day after a basketball game he began to have general myalgies and dark urine. In order to reduce muscle pain, he initiated a treatment with ibuprofen (1.200 mg/d during 3 days.) In the following days it was verified nausea, vomit and a volume drop of diuresis, reasons why he visited our centre.
The patient was found to be hypertensive (160/90 mmHg), without fever, in a good general condition and slightly dehydrated. The analytical study revealed leukocytes (13.400 x103/μl) with neutrophilia (85%), haemoglobin 14.5g/dl, plasmatic creatinine 13,1mg/dl, urea 233mg/dl, sodium 127mEq/l, potassium 5.4mEq/l, calcium 8.1mg/dl, albumin 2.5g/dl, LDH 2.649U/L, CPK 2.266U/L, uric acid 9mg/dl, phosphorus 5.2mg/dl, GOT 83U/L and GPT 264U/L. Urine: creatinine 87mg/dl, sodium 48meq/l, haemoglobin (3+), sediment 15-20 haematids/field.
He was treated by recovering the loss of volume and through urine alcalinization. However, the renal function continued to get worse. On the 4th day of treatment and after two sessions of haemodialysis, he began to recover his renal function which returned to normal after three weeks. The myalgia improved progressively until it disappeared.
With the clinical possibility of a MM, given the recurrent nature of the picture and its relation with physical exercise, once it was recivered ARF the patient underwent a muscle biopsy that gave a normal histology. Nevertheless, by determining the enzyme activity of Carnitine Palmitoyl transferase (CPT) in the muscles through isotope exchange – performed in the hospital’s research centre on the 12th of October, in Madrid – it was detected a reduced activity with a result of 0.07nmol/min-1/mg-1 NPC, with the lowest reference limit being 21 nmol/min-1/mg-1 NPC. It was diagnosed a deficiency of CPT and the patient was told to avoid prolonged physical exertions and to eat frequently with a diet low on calories and high on carbohydrates.
CASE 2
A 39-year-old man, diagnosed 20 years earlier with McArdle’s Disease through muscle biopsy, performed after showing episodes of acute myalgia related with physical exertions during childhood. A study of the family history revealed the same affliction in four of his 11 brothers, in who the problem seemed to have no clinical significance.
After spending several days using a transcutaneous electrical stimulation device with the purpose of increasing muscle mass in the abdominal wall, he began to experience strength loss, myalgia, dark urine and decrease in diuresis. The patient visited our centre one week later. He was found to be normotensive, without fever, presenting serious oedemas in lower limbs and with oliguria.
In the analytical study, the hemogram was normal, plasmatic creatinine 12,4mg/dl, urea 128mg/dl, sodium 134meq/l, potassium 5.5meq/l, calcium 6.9mg/dl, albumin 3g/dl, LDH 406U/L, CK 15.507U/L, uric acid 5.8mg/dl, phosphorus 5.4mg/dl, GOT 88U/L and GPT 148U/L. A radiography of the chest revealed bilateral pleural effusion and interstitial oedema.
He required treatment with nine sessions of haemodialysis, achieving a negative hydric balance of more than 18kg. After two weeks of treatment, he began to recuperate diuresis and slowly decrease the plasmatic creatinine until it became normal. There was also a complete recuperation of muscle strength. The patient was advised to avoid physical exercise and increase his diet's protein level.
DISCUSSION
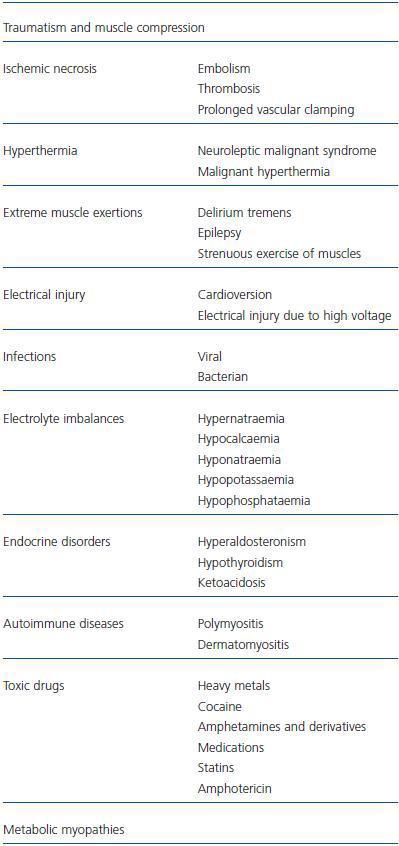
In 1941 it was performed the first detailed description of rhabdomyolysis.1 Since then, numerous cases report has been published and it has been known a growing list of possible etiologies2 (table 1.)
In the 50s a group of patients was diagnosed with recurrent episodes of rhabdomyolysis, often starting in childhood and with a family history of myoglobinuria. After 1970, hereditary enzyme abnormalities related with these recurrent cases began to be verified.
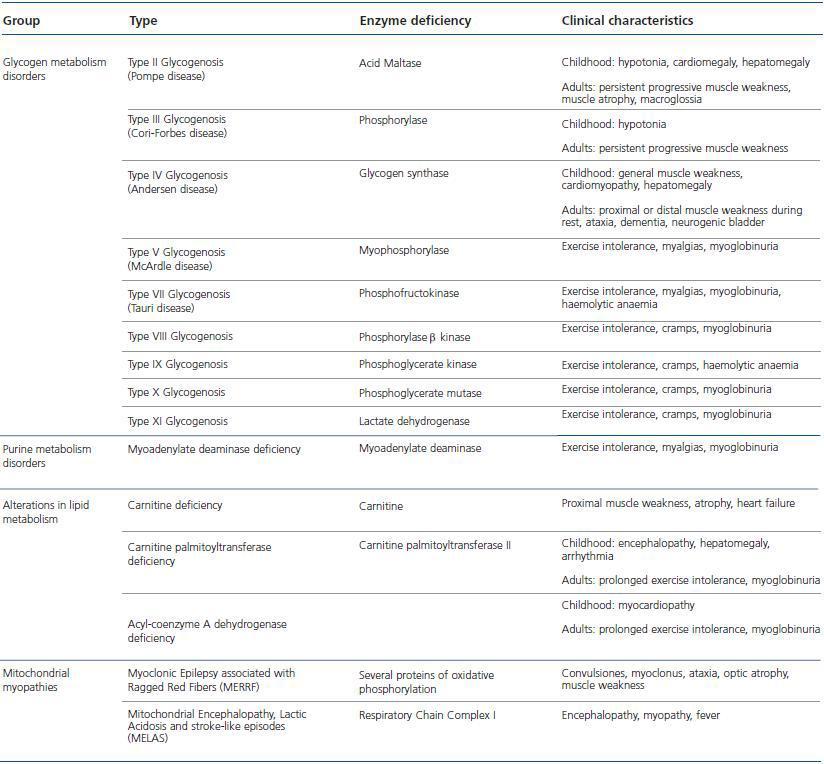
MM create a heterogenous group of uncommon diseases where the energetic metabolism of the muscles is changed, resulting in a skeletal muscle dysfunction. These are ordered according to the way they affect the metabolic pathway of glucogen, lipids, purines or mitochondrial metabolism3 (table 2.) Even though it has not been established a precise mechanism for muscle necrosis, it is likely that the insufficient production of energy during exercise may lead to a depletion of ATP that can jeopardize muscle cells.4
In the first case, the patient was diagnosed with CPT deficiency, a rare abnormality of the lipid metabolism related to autosomal recessive inheritance (AR.) Even though it represents a small percentage of rhabdomyolysis cases, it is the most common MM.
The enzyme deficiency prevents the transportation of fatty acids to the mitochondrion for beta oxidation and later ATP synthese. When performing a prolonged physical exercise (at least one hour) the energy produced through this pathway is necessary after the depletion of glycogen reserves and the resulting muscle injury include myalgia and in some cases myoglobin, with possible complication of ARF. Known triggering effects include fasting, fever and anti-inflammatory drugs.5 The patient suffered myoglobinuria after performing prolonged physical exertions. Furthermore, the described episode was associated with the use of ibuprofen, which can prompt the development of ARF.
Mc Ardle’s the most common disorder of muscle carbohydrate metabolism and the second most common MM that causes rhabdomyolysis." AR inheritance is also caused by mutations in the genetic code of myophosphorylase enzyme. Its deficiency makes the glycogen’s metabolism difficult, which comprises the main source of muscle energy specially when performing short and intense exercises. Patients with McArdle’s disease present intolerance to shortterm exercise and cramps or muscle weakness especially as in the case of our patient when he was subjected to short and frequent periods of physical exercise through the use of an electrostimulator. Up to half the cases of McArdle’s disease begin with episodes of rhabdomyolysis and half of these complicate with ARF.2
A clinical analysis is essential for the diagnosis of MM. Regarding the inheritance of AR, in many cases it is verified that family history is not a determinant factor. However, it is very important for rhabdomyolysis to be frequent and begin during childhood. The clinical characteristics of the main MM useful for a differential diagnosis is summarised in table 2. The definitive diagnosis requires a muscle biopsy in order to identify the enzyme disorder through molecular biology techniques.
Currently, there is no cure. Being careful with hygiene and diet will also help to prevent myoglobinuria.2 It is necessary to control physical activity. Concerning CPT deficiency, excercises should be short-time and avoided in case of fasting or infections. It is recommended to have a frequent meals with a low fat and high carbohydrate diet, which will be the main source of energy in these cases. The daily consumption of medium chain triglycerides can be beneficial, as verified in some cases.6
As for myophosphorylase deficiency, besides limiting physical exercise, it is advised to increase the diet’s protein level, since it improves resistance and muscle operation in most cases.7 On the other hand, it was verified in a controlled study with 12 patients that sucrose intake before exercise improves considerably its tolerance. The sucrose is quickly converted in glucose and fructose, which the muscle will use to obtain energy due to the inability to metabolize muscle glycogen. Although useful, it is a measure that should be taken with caution due to the high level of calories, which can result in an excessive weight gain.8 Vitamin B6 supplements were also found to be beneficial in case of McArdle’s disease, but needs to be verified by controlled studies.9
Perhaps in the near future a specific treatment will be available by enzyme replacement or a genetic treatment that will allow to improve effectively the tolerance to exercise, preventing episodes of rhabdomyolysis.
Table 1. Causes for rhabdomyolysis
Table 2. Metabolic myopathies