Pleuroperitoneal leak (PL) is an uncommon complication in peritoneal dialysis (PD), with an estimated incidence of less than 2%,1–3 but leading to a large proportion of patients abandoning the technique.3
There are multiple predisposing factors including diaphragmatic muscle hypotonia, congenital diaphragmatic defects, increased pleuroperitoneal pressure gradients, as may occur in polycystic kidney disease, and impaired lymphatic drainage.1,4
Clinically, PL manifests as dyspnoea of more or less sudden onset, loss of ultrafiltration and pleural effusion3, but there are no cases in the literature with the reason for consultation being an episode of seizures due to posterior reversible encephalopathy syndrome (PRES) when performing PD and in which there was a massive PL.
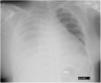
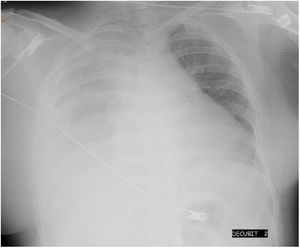
We present the case of a 24-year-old woman with chronic renal failure due to IgA mesangial nephropathy on continuous ambulatory peritoneal dialysis for one month, who was transferred to the emergency department due to intense headache and blurred vision with subsequent loss of consciousness and generalised tonic-clonic movements while undergoing PD replacement. Her previous medical history also included obesity, with a BMI of 32, and hypertension controlled with enalapril and furosemide. The patient subsequently suffered two more episodes of seizures and her blood pressure (BP) was 260/112 mmHg and O2 saturation 87%. The recent history reported by the family included a decrease in peritoneal drainage balances and right rib pain for 2–3 days, and worse control of her BP with values of 165/100 mmHg. She was initially received oxygen therapy, intravenous labetalol, clonazepam and levetiracetam, with a gradual decrease in blood pressure. Further tests included a chest X-ray, showing massive right pleural effusion (Fig. 1), blood tests, showing electrolytes to be normal, normal brain CT scan, lumbar punction with no evidence of infection and eye fundi with preserved macula in both eyes, with no exudates or haemorrhages suggestive of hypertensive retinopathy. Analysis of the pleural fluid was compatible with transudate, with glucose levels higher than plasma blood glucose. With the diagnosis of a massive right pleuroperitoneal leak and given the severity of the patient's clinical condition, a right jugular catheter was inserted and haemodialysis with progressive ultrafiltration started, with recovery of consciousness, gradual decrease in pleural effusion and optimisation of BP control. MRI of the brain at 24 h showed lesions compatible with PRES. Ten days later, a peritoneal scintigraphy showed, 90 min after administration of the radiotracer, diffuse passage of the radiotracer to the right posterior pleural region, occupying a large part of the right thoracic region and causing the patient right pleuritic pain and dyspnoea. We decided to definitively discontinue the PD.
Although there are numerous published cases of PRES in patients with renal failure, many of them on haemodialysis, few cases have been reported in patients on PD. Virtually all of them had seizures as an initial symptom, and volume overload and poor compliance with dialysis were the main contributing or aggravating factors.5,6 In a review of the literature we did not find any cases in which PL was the triggering cause of PRES.
Conservative treatment of PL is effective in approximately 50% of patients.5 In the case we present here, the severity of the symptoms and the suspicion of a possible diaphragmatic defect led us to definitively discontinue PD. Progressive ultrafiltration through intensification of the haemodialysis programme achieved resolution of the PRES and PL.