With regard to the article published in the journal of Nefrología "Iliac artery stenosis after kidney transplantation as a cause of refractory hypertension and claudication"1 and a review on posterior reversible encephalopathy syndrome (PRES),2 published in NefroPlus, we present a case that is closely related to both publications.
Vascular problems remain one of the main complications after kidney transplantation, with an incidence of 3%–15%.3
Post-transplant arterial hypertension (HTN) secondary to decreased renal blood flow, due to the involvement of the graft artery or less frequently of the proximal aorto-iliac segment,4 is a correctable form1 of HTN.
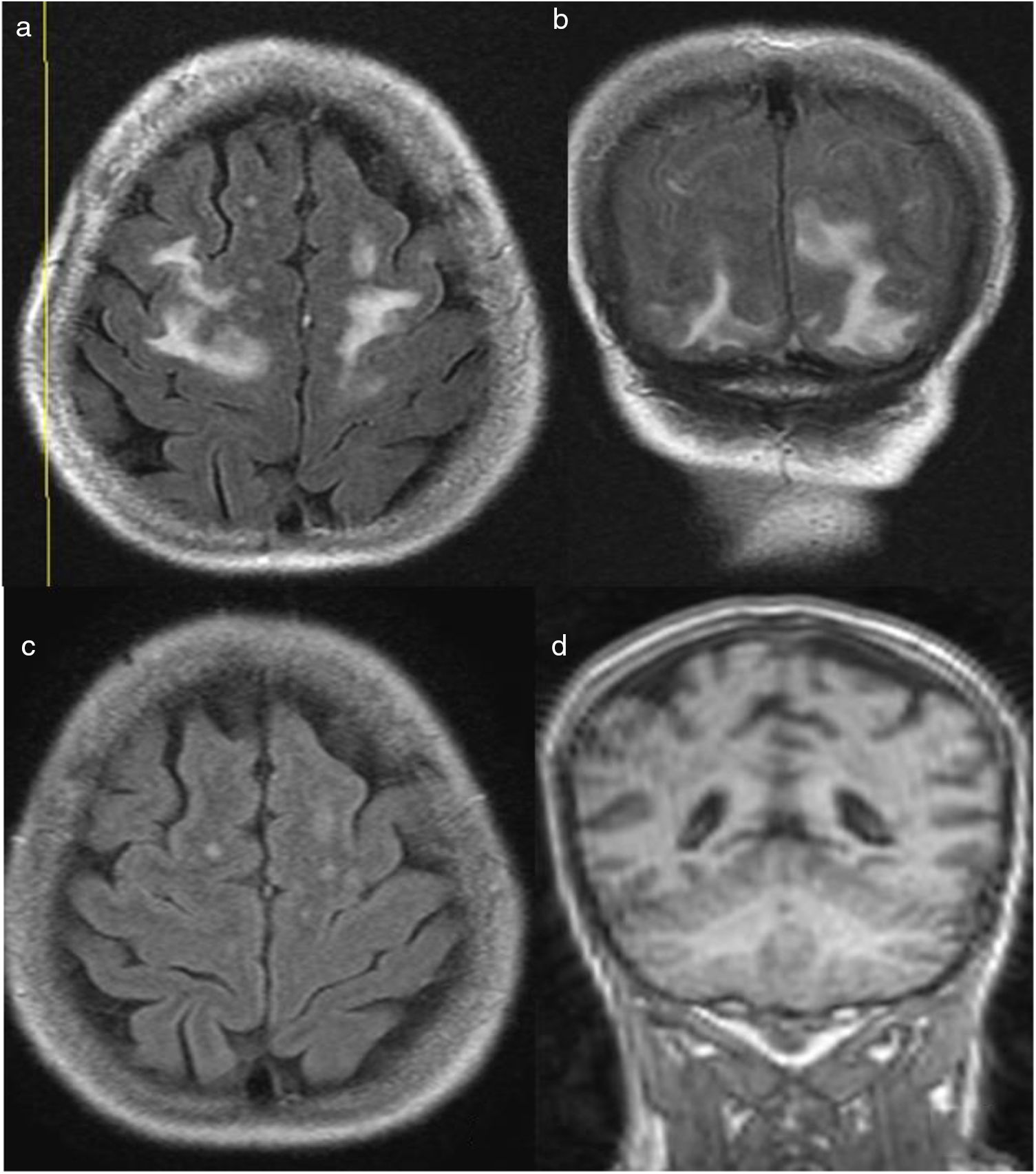
We present the case of a 62-year-old woman with a history of chronic tubulo-interstitial nephropathy and HTN controlled with amlodipine, who had received a kidney transplant and was on immunosuppressive treatment with tacrolimus, sirolimus and prednisone. At 3 weeks, she began with complaints of severe headache, vomiting and blurred vision, associated with refractory HTN, with no evidence of impairement in renal function or proteinuria. The eye fundi showed a grade 2 hypertensive retinopathy. Given the clinical suspicion of hypertensive encephalopathy, a brain CT scan was ordered, with findings compatible with PRES, which was confirmed by brain nuclear magnetic resonance (MNRB) (Fig. 1a and b). Due to poor blood pressure control, hypotensive treatment was intensified; complementary examinations were performed to rule out causes of secondary hypertension and tacrolimus was discontinued, although its plasma concentration remained within the target therapeutic range from admission.
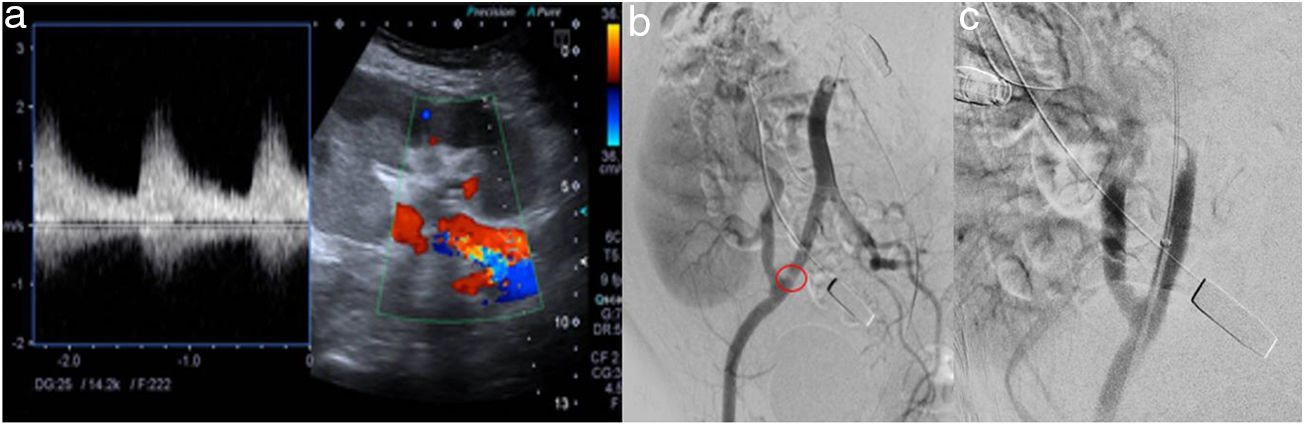
The study of secondary HTN was negative, except for the echo-Doppler of the graft, which reported probable renal artery stenosis (tardus parvus morphology and increased speeds up to 200 cm/s in the proximal portion) (Fig. 2a). CT angiography posed the possibility of arteriovenous fistula, being not very assessable due to artefact (right hip prosthesis), so selective arteriography was performed that evidenced a stenosis of the external iliac artery prior to anastomosis of the artery of the graft (Fig. 2b), with reduction of the calibre of the lumen to 3.5 mm. An endovascular treatment was then performed with angioplasty of the stenosis, achieving a good morphological result. (Fig. 2c), with this procedure with/without stent being the treatment of choice in this type of pathology.4
At 24 h blood pressure was better controlled, with gradual disappearance of the symptomatology, which allowed the hypotensive treatment to be progressively reduced.
The MNRB, which was performed one month later, showed a significant improvement in the signs of PRES (Fig. 1c-d). In the control echo-Doppler there were no findings compatible with vascular alteration of the graft and the tacrolimus was reintroduced. The patient is currently asymptomatic and normotensive.
Some authors point to refractory hypertension as the fundamental element in the diagnosis of stenosis of the proximal iliac segment,4 with the echo-Doppler being the screening technique of choice followed by CT angiography as a confirmatory test.1 Both were inconclusive in our case and it was necessary to resort to arteriography, prior to endovascular treatment.5
The form of clinical presentation meant that PRES, a potentially reversible and rare clinical-radiological entity, which manifests itself with acute neurological symptoms (alterations in consciousness, seizures, headache, visual disorders, focal neurological deficit, etc.)6 had to be ruled out. The pathophysiological changes that underlie PRES are not fully known,6 although some researchers postulate that abrupt fluctuations in blood pressure figures cause dysfunction of the self-regulation of cerebral blood flow and cause endothelial injury with subsequent vasogenic oedema.2,7
This syndrome is related to several diseases, such as hypertensive encephalopathy, acute or chronic kidney disease, thrombotic microangiopathy, autoimmune diseases, vasculitis and immunosuppressive drugs.2 Regarding the latter, calcineurin inhibitors such as tacrolimus have been related to having direct cytotoxic effects on the cerebral endothelium,8 even with normal serum levels.9 This data led us to the withdrawal of this drug in our patient, without improvement of the clinical picture.
Clinical suspicion, laboratory tests and the use of an adequate imaging test help establish a diagnosis of certainty.2 MNRB is the method with the highest diagnostic value, which makes it possible to differentiate this syndrome from acute ischaemic lesions,10 objectifying in our case hyperintense areas in the occipital and bilateral frontal subcortical white matter,2,8,10 corresponding to the findings described in the literature.
As treatment, HTN control measures, the discontinuation of potentially implicated medications and the treatment of underlying disorders are recommended.6
A post-transplant ischaemia triggered a refractory HTN that led to the development of a posterior reversible encephalopathy, so incorporating this entity as a differential diagnosis of acute neurological conditions in kidney transplant patients with hypertensive disorders or in immunosuppressive treatment mainly with calcineurin inhibitors may contribute to early diagnosis and timely treatment to avoid cases of irreversibility.
Please cite this article as: Franco A, González Y, Balibrea N, Díaz M, Planells MC, Pérez Contreras FJ. Síndrome de encefalopatía posterior reversible en paciente trasplantada renal con hipertensión arterial refractaria secundaria a estenosis de arteria ilíaca. Nefrologia. 2019;39:677–679.