Data recorded from external visit in hospitals, reflects high number of nephrectomized patients. Most of these patients were remitted after any surgery or deteriorizated renal function or any other associated pathology. Several studies of nephrectomized patients are reported in literature concerning both healthy patients and comorbility factors, and renal function and its evolution are evaluated. However, obtained results present a wide variability, which needs to be assessed. In this study we present a retrospective observational study of 92 one-kidney surgical patients, visited in Nephrology surgery of University Clinic Hospital. Patients presented an average age of 67 years old (range 22-89 years old), and a post-surgery monitoring of 21 years. Population was divided in two groups according with their glomerular filtration (FG). Before surgery, group 1 presented FG <60 ml/min and group 2 >60 ml/min, respectively. Group 1 patients (a total of 24 patients) presented an FG average of 48 ml/min, 8% had proteinuria and 63% presented high blood pressure. 21% of them needed an average of 20 years (10-30 years) to reach E4 and E5 steps and in general, most of them progressed to insufficient renal chronic disease. Five cases achieved renal therapy replacement. Group 2 patients, composed of a total of 68 patients, had an FG average of 76.5 ml/min, and 10% of patients presented proteinuria and 34% HTA; however, 80% of group 2 patients achieve E3 step with average age of 17 years, and a post-surgery of 47 years (1-48 years). A total of 19.1 % presented an FG higher 60 ml/min with an average development of 22 years along their evolution. According to the results obtained it is suggested that monorrenal surgical patients present a low progression of renal disease and it is also observed a progressive tendency to the chronic renal failure due to emerging of proteinuria.
A las consultas externas de nefrología acude un importante número de pacientes nefrectomizados, quienes son remitidos tras la cirugía o bien cuando presentan un deterioro de la función renal o alguna otra patología asociada. Existen diferentes estudios sobre pacientes nefrectomizados en los que se valoran la función renal y su evolución (tanto en sanos como en pacientes con factores de comorbilidad), con unos resultados muy variables. Presentamos un estudio observacional y retrospectivo sobre 92 pacientes, monorrenos quirúrgicos, atendidos en las consultas de nefrología de nuestro centro, con una edad promedio de 67 años (rango, 22-89 años) y con un promedio de seguimiento posterior a la cirugía de 21 años. La población fue dividida en dos grupos según el filtrado glomerular (FG): los pacientes del grupo 1 presentaban un FG inferior a 60 ml/min antes de la cirugía y los del grupo 2 presentaban un FG superior a 60 ml/min. En el grupo 1, en el momento de la nefrectomía, 24 pacientes tenían un FG promedio de 48 ml/min, el 63% hipertensión arterial (HTA) y el 8% presentaban proteinuria. El 21% de los pacientes del grupo 1 tardó 20 años de promedio (10-30 años) en entrar en estadios 4 y 5, y 5 casos evolucionaron hasta necesitar terapia renal sustitutiva. El grupo 2 estaba formado por 68 pacientes con un FG promedio de 76,5 ml/min, un 34% con HTA y un 10% con proteinuria. El 80% del grupo 2 alcanzó el estadio 3 en un promedio de 17,47 años después de la intervención quirúrgica (1-48 años). El 19,1% presentaron, a lo largo de su evolución, un FG superior a 60 ml/min, tras una media de 22 años de evolución. Nuestros resultados indican que los pacientes monorrenos quirúrgicos presentan una progresión de la enfermedad renal muy lenta, y se observa una tendencia a la progresión de la insuficiencia renal al presentar proteinuria.
INTRODUCTION
Nephrology outpatient services receive a significant number of nephrectomised patients, who are referred after surgery, when there is a decrease in kidney function, or when another associated disease arises. Experimental studies have shown that after the reduction of renal mass, hyperfiltration develops. This is a compensatory mechanism that prevents glomerular filtration rate from decreasing1,2 (preglomerular vasodilation, increase in nephron plasma flow and increase in glomerular intracapillary pressure).3 The suspected diagnosis is based exclusively on clinical data, such as the appearance of proteinuria and a decrease in glomerular filtration rate. These changes can be harmful in the long term, especially if they are associated with risk factors, including arterial hypertension (HT), diabetes mellitus, dyslipidaemia, microalbuminuria, proteinuria, obesity, and others.4-6 Published studies do not agree unanimously about the evolution of patients with a unilateral nephrectomy.7-10 The few publications that we find on this topic present series of selected patients with no kidney disease prior to surgery, and they do not address patients with bilateral kidney disease.11,12 With this in mind, the objectives for this project are to study how kidney function evolves in our nephrectomised patient population and to analyse for risk factors that may be involved in the evolution of a more advanced stage of kidney disease, whether at the time of the nephrectomy or throughout the progression of the disease, in order to be able to detect and control them at early stages.
PATIENTS AND METHODS
We performed a retrospective observational study of cases and controls with patients who had undergone nephrectomy for different reasons. These patients were seen in our nephrology department at the Clinical University Hospital of Valencia between 2005 and 2007, and their progress was monitored from the nephrectomy up to the present. We examined 210 patients with a single functioning kidney and excluded 118 for not having undergone a nephrectomy. We therefore included 92 patients with an average follow-up time of 21 years (1-51 years). The study variables were the following: anthropometric data (sex, age, weight, height and body mass index [BMI]), reason for nephrectomy, glomerular filtration rate (GFR), (GFR evolution from the time of the procedure to the present, and time of initiation for stage 3, (GFR 30-59ml/min), stage 4 (GFR 15-29ml/min), stage 5 (GFR < 15ml/min) or stage 5D (dialysis).13 Cardiovascular risk factors were proteinuria, HT, diabetes mellitus, dyslipidaemia and anaemia, as well as pharmacological treatments (ACEI and/or ARBs, statins and/or fibrates, erythropoietin and/or iron). Glomerular filtration rate was measured using creatinine clearance or MDRD depending on the time when the nephrectomy was performed (keep in mind that the method for measuring GFR has changed over the years). The study population was divided into two groups for further analysis. Group 1 consisted of patients whose GFR was > 60ml/min before surgery, and group 2 of patients whose GFR was above 60ml/min before surgery; both groups were analysed separately. SPSS 15 software was used for the statistical study, and the quantitative variables were compared for both groups using Student’s t-test and the Wilcoxon test depending on variable distribution. The Kaplan-Meier method was used to predict time of evolution. Meanwhile, binary multivariate logistic regression analysis was used to analyse the influence of different factors on the progression of chronic kidney disease (CKD).
RESULTS
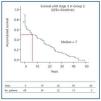
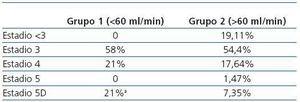
The patient total was 46.92% male; patients’ average age was 67 years (22-89) and 53.08% of them had a left nephrectomy. The cause of the nephrectomy was pyelonephritis in 24 cases, tuberculosis in 13, lithiasis in 12, clear cell carcinoma in 12, congenital dysplasia in 7, adenocarcinoma in 6, other tumours in 8, traffic accidents in 4, hydronephrosis in 4, live donation in one and renal haematoma in one. Lithiasis in the reserved kidney was present in 17.39% of the patients, with subsequent episodes of renal colic or pyelonephritis. Group 1 (GFR < 60ml/min) consisted of 24 patients, 46% of which were male. They had the following characteristics at the time of the nephrectomy: average age 51 years (32-75), average GFR 48ml/min (18-59ml/min; 86% stage 3), 63% with HT and 8% with proteinuria. In this group, 58% did not experience decreased renal function during follow-up; in the rest (42%), there was an average delay of 20 years (10-30 years) to evolve from stage 4 to stage 5, and five cases needed renal replacement therapy (21%) (Table 1). Group 2 (GFR > 60ml/min) consisted of 68 patients, 44.2% of which were male. They had the following characteristics at the time of the surgical procedure: Average age 51.5 years (16-60), average GFR of 76.5ml/min (60-133.8ml/min), 34% with HT and 10% with proteinuria. In group 2, 80% reached stage 3 in an average of 17.47 years after the operation (1-48 years). These patients’ condition at present is as follows: 54.4% in stage 3; 17.64% in stage 4; 1.4% in stage 5, and 7.3% in stage 5D (Table 1). Throughout a follow-up period spanning an average of 22 years (6 to 33 years), 19.1% presented a GFR higher than 60ml/min. The risk factors for both population groups at the time of the nephrectomy and at the present time are shown in Table 2. Table 3 describes the treatment currently administered to patients. We find no significant differences. In the second group, 10% of the patients presented proteinuria. Throughout the follow-up period, we observe that 62% of the patients have had proteinuria, with an average level of 1.26g/24 h (0.3 to 4.9g/24 h). In group 1, corresponding to patients who had a decreased kidney function at the time of the surgery, 8% of the patients presented proteinuria; this number became 57.14%, with an average proteinuria level of 0.52g/24 h (0.3 to 1g/24 h). Evolution of kidney function in group 2 patients with proteinuria before the surgery was as follows: 44% in stage 3, 28% in stage 4 and 28% on renal replacement therapy (RRT). If we analyse our population by BMI, we find that those with a BMI higher than 30 are more likely to have proteinuria than those with a lower BMI, although we did not detect greater deterioration of kidney function (Table 4). In the group with a pre-surgery GFR higher than 60ml/min (group 1), 50% of the population reaches stage 3 in seven years according to the Kaplan-Meier curve (Figure 1). In group 2, the mean time to reach stage 5D is 23 years (19 to 27) (Figure 2). In group 1, progression from stage 4 to stage 5 occurs in a mean time of 10-30 years, and dialysis is needed in 24% of the cases. We must consider the presence of risk factors: 87.5% obesity, 71% HT, 57.14% proteinuria, 43% dyslipidaemia, 41.66% diabetes mellitus and 33.33% anaemia. All of the above favour the progression of kidney disease, although when we realize how long it takes for patients to progress to stage 4 or 5, we can state that evolution is slow. In group 2, the average time to reach stage 3 is 17.3 years after the surgery. Only 7% of the patients require RRT and 54% of the patients did not reach stage 4 or 5. After 22 years of follow-up, 19% of the patients in this group continued to maintain a GFR of more than 60ml/min. In the logistic regression analysis, the only variable predicting evolution toward renal failure is GFR at the time of the nephrectomy; patients with proteinuria tended to present a decrease in filtration that was not statistically significant.
DISCUSSION
In our study, the only significant factor for predicting CKD progression was GFR below 60ml/min at the time of surgery, which results in a faster decrease in GFR. We cannot ignore the fact that this study has an important limitation, due to being a retrospective study with many years of follow-up. Furthermore, it has a selection bias, since the patients in the study include both those who were referred after surgery or at such time as they presented a slight decrease in renal function and those who had another type of associated cardiovascular disease. As we see in other studies of healthy nephrectomised patients, the decrease in GFR also occurs very slowly in our study.14,15 The average time in which a patient in the group with GFR > 60 reached stage 3 was 17.3 years. In other studies, progression is slower and patients present statistically significant comorbidity factors such as obesity and proteinuria.16,17 The rapid decrease in GFR in these patients is therefore related not only to the hyperfiltration phenomenon but also to the associated risk factors. If we analyse proteinuria considering GFR, we see that patients in the higher GFR group present increased proteinuria. This is because if GFR decreases, then the glomerulus ability to excrete proteins is also less; the lower the GFR, the lower the proteinuria. However, we also observe that over time, there has been an increase in proteinuria in both groups. The measurement technique employed has probably had an effect; proteinuria was initially measured using a 24-hour proteinuria test. This type of technique tends to lead to proteinuria assessment errors due to the difficulty quantifying the true volume in diuresis. The technique that best reflects proteinuria level is the urinary protein-creatinine index, which is the one used today. At the same time, we observe a significant increase in proteinuria over time, and one that is larger than that observed in studies of nephrectomised patients with no associated risk factors,18 due to most of our patients presenting an associated condition along with proteinuria at the time of the nephrectomy. Among the six patients that received RRT, four presented kidney diseases that tend to affect both kidneys (two had tuberculosis [TB], one had pyelonephritis, and the last had renal lithiasis). Therefore, at the time of surgery, these patients had a lower renal mass. In our group, six patients presented a notably longer follow-up time (surgeries performed between 1956 and 1962) and the reason for the surgical procedure was renal lithiasis in four cases and pyelonephritis in the other two. In this group, we observe that the patients’ GFRs were not below 60ml/min, and that after 43 and 36 years of followup in our department, none has needed RRT and their mean GFR is 32.28ml/min (range: 48 to 23ml/min). At present, all of these patients have HT and 66.6% present proteinuria, which is under good control with pharmacological treatment. These are the patients with the longest follow-up and examination histories in our department, and they seem to be progressing well. If we analyse our patients by their BMI, we see that present more proteinuria (differences are not significant), but we do not observe differences having to do with renal failure progression. This is because there are high numbers of obese patients in both groups. This result differs from findings in the study by Praga et al. These authors evaluated the correlation between obesity and decreased GFR due to hyperfiltration in a group of patients with unilateral nephrectomies. They observed that obesity in the nephrectomised patients favours developing proteinuria and renal failure.19-21 We may therefore conclude that in the study population, the only significant factor for predicting CKD progression in nephrectomised patients is a GFR below 60ml/min at the time of surgery. Furthermore, we observe a tendency toward progression to renal failure in patients with proteinuria
Table 1. Current stage according to glomerular filtration rate.
Table 2. Risk factors for groups 1 and 2 at the time of the nephrectomy and at prese
Table 3. Treatment for groups 1 and 2 at present
Table 4. Classification according to BMI at the time of the nephrectomy and the stages of renal failure patients have reached, and according to current presence of proteinuria.
Figure 1. Survival before reaching stage 3 in group 2 patients (GFR > 60ml/min) following the nephrectomy.
Figure 2. Survival before reaching stage 5D in group 1 patients (GFR < 60ml/min) following the nephrectomy.