Dear Editor:
Familial Mediterranean fever (FMF) is an autoinflammatory, autosomal recessive inherited disorder, characterised by recurrent attacks of fever and serositis.1 The identification of mutations in the MEFV gene has been of major assistance in early diagnosis in the majority of cases. Among the possible mutations, M694V is the most common, and is the mutation responsible for the most severe cases in heterozygous carriers.2 The most significant long term complication is chronic renal failure caused by AA amyloidosis.3We describe the case of a female in which this disease presented itself in the form of nephrotic syndrome. Furthermore, we carry out a clinical follow-up of the response obtained after one year of combined colchicine and infliximab therapy.
Clinical case study
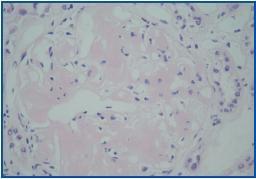
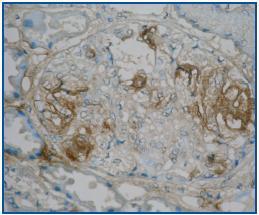
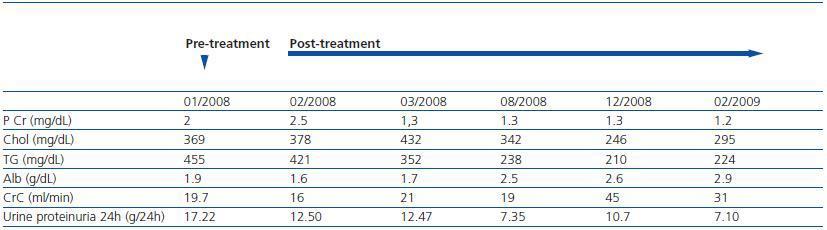
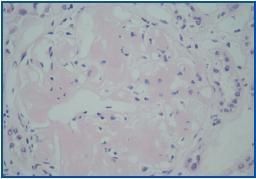
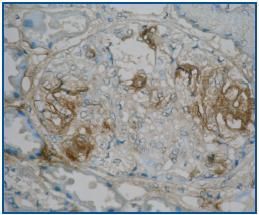
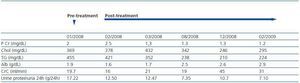
38 year old female, originally from Armenia, with no relevant personal history and a family history of father with nephropathy, who died at 50 years of age, and maternal aunt also with nephropathy. The patient was assessed for nephrotic syndrome in the nephrology department. In the assessment the patient described, in addition to oedemae in the lower extremities and palpebrae, nonspecific lumbar pain. During the assessment for nephrotic syndrome, the patient required numerous admissions for hydropic decompensation. A renal biopsy was carried out, with the discovery of eight glomeruli per section plane. These all showed a massive and diffuse deposit of congo red-positive amorphous, acellular and eosinophilous matter (figure 1A). The immunohistochemical study showed congo red positivity for AA (figure 1B), this being the definitive diagnosis of amyloidosis AA. Given the family history of nephropathy, the patient¿s country of origin and the presence of secondary amyloidosis, a genetic study was carried out which showed the presence of M680I and M694V mutations in heterozygosis in the MEFV gene associated with FMF. Treatment with colchicine was started at a dose of 0.5mg every 8hrs/day and infliximab at a dose of 5mg/kg IV, in basal form, for two weeks, and thereafter every two months. The patient¿s subsequent progress after establishing the treatment regime is detailed in table 1.
Discussion
FMF manifests clinically in the form of attacks of fever, peritonitis, pleuritis or polyarthritis.1 As a consequence of these inflammatory episodes, development of renal amyloidosis is common, worsening the prognosis.3 Gingold-Belfer et al.4 describe the case of a female patient in whom nephrotic syndrome was the primary manifestation of FMF, detected via the presence of an M694V mutation. Similarly, in our patient the diagnosis of FMF was also made via an assessment for nephrotic syndrome, since her symptoms did not relate to the classic symptoms of FMF and thus its presence was not suspected. In the case which we have described, our attention was drawn to the already advanced stage of the disease at diagnosis, with findings of severe nephrotic syndrome and AA amyloid deposits in the kidney. Furthermore, the presence of two mutations was detected, one of which (M694V) is the most common and that which is found in the most severe cases2 such as ours.
With regard to treatment, colchicine is the drug typically used to treat this condition.3 In cases of intolerance (diarrhoea) or inefficacy, other therapeutic options are considered.5 TNF-alpha is a proinflammatory cytokine which can play a role in FMF as well as the development of secondary amyloidosis.6 TNF inhibitors can therefore be of use in FMF.7 This is reflected in some publications, where it is described how anti-TNF-alphas, including infliximab, reduce the frequency of FMF attacks and, therefore, bring about a recovery from proteinuria.6,7 Considering that our patient did not tolerate antiproteinuric drugs (ACEI, ARA II), and given the severity of proteinuria and deterioration of renal function, as well as the biopsy findings which demonstrated amyloidosis, we decided to use a combined treatment of colchicine and infliximab to assess her progress. This combined therapy has achieved a subjective improvement in the patient (there has been no hydropic decompensation throughout the year, nor admission for any other motive), as well as a recovery of renal function and a stabilisation in the proteinuria with an increase of albumin in the plasma. It is possible that this only partial response which we have obtained with combined therapy could be due to the fact that the disease presented itself without the typical symptoms, and it was its first complication (renal amyloidosis) that allowed us to reach a diagnosis, indicating that the disease was already advanced at the time of diagnosis. However, it could also be due to the fact that the patient was a carrier of the M694V mutation, which is associated with the most severe cases.
With regard to the tolerance and safety of infliximab, we have detected no adverse effect with this medication or any infectious complications during the period of its administration, indicating a good level of tolerance. In conclusion, an unusual presentation of FMF could delay diagnosis and, therefore, worsen the prognosis in these patients. For those cases in which amyloidosis is the manner through which a diagnosis of FMF is reached, a combined therapy of colchicine and infliximab could be of use at least to achieve a stabilisation of the disease.
Figure 1a.
Figure 1b.
Table 1. Development of the analytic parameters alongside combined therapy (colchicine+infliximab)