Dear Editor:
Nephrotic-range proteinuria is a rare form of presentation of primary antiphospholipid syndrome (PAPS). Renal anifestations of PAPS can be acute or chronic, accompanied by hypertension and progressive renal failure.1 Chronic kidney disease (CKD) with a reduction in glomerular filtration is evident in the majority of studies, with an incidence range of 56-100%. Principal treatment is based on anticoagulation with an INR >3.2 On rare occasions treatment with immunosuppressant drugs has been tried, with a variable response3.
Clinical case
31 year old patient with paranoid schizophrenia and depressive syndrome, mixed dyslipidaemia, smoker and drinker. Thrombosis of the femoral veins, up to the inferior vena cava, and left renal vein; plasma creatinine (PCr) of 2.7mg/dL, in treatment with acenocoumarol (INR 2-3).
The patient attended consultation with negative hypercoagulability, PCr 2.1mg/dL and proteinuria of 2g/24h. The ultrasound showed the right kidney at 13.6cm and the left at 10.5cm, with some cortical scarring. The patient reported a sedentary lifestyle with dyspnoea of moderate strength. Arterial tension normal, with moderate obesity. Isotope renogram with Tc99m showed renal asymmetry with minor cortical scarring.
Laboratory tests: platelets 100-130 10^3/ul; urea: 50; creatinine: 1.7; uric acid: 10.4; triglycerides: 676; cholesterol: 303mg/dL; albumin 3.5g/dL; remainder normal. Immunological test was negative except for positive lupus anticoagulant in several findings. Proteinuria: 9g/24h, normal sediment. CrCl: 100ml/min.
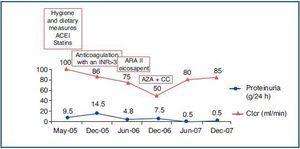
Given the patient¿s clinical characteristics, a right renal biopsy using microlumbotomy was proposed, but refused. We started treatment with enalapril, allopurinol, atorvastatin and hygiene and dietary measures (figure 1).
Six months later the patient suffered a superficial phlebitis of the right lower extremity with deterioration in renal function (CrCl 86ml/min) and an increase in proteinuria, passing from 9 to 14.5g/24h. An angio-MRI was carried out which confirmed stenosis of the right renal artery, thus increasing the INR to >3. The stenosis was not evident in a follow-up x-ray (figure 2).
Since the proteinuria had not abated, in the context of myocarditis therapy was started with carvedilol and telmisartan, eicosapent, decreasing the proteinuria to 4.8g/24h with a CrCl of 75ml/min.
In 2006, given the new deterioration of renal function (CrCl 50ml/min), the possibility of immunosuppressant treatment was agreed with the patient and his family. Empirical treatment was begun with prednisone 0.5mg/kg/day and azathioprine 100mg/24h. The patient demonstrated a progressive decrease in proteinuria. Six months after beginning immunosuppressant treatment, proteinuria was 0.5g/24h with a CrCl of 80ml/min; thus the azathioprine was withdrawn, with just 10mg/24h steroids remaining.4,5
We reached a diagnosis of stage II CKD secondary to PAPS, associated with nephrotic-range proteinuria, corrected with azathioprine and steroids.
Discussion
Nephrotic syndrome is a rare finding that can be induced by thrombotic microangiopathy affecting the glomerular level. We could not discern the type of glomerular lesion since a renal biopsy was refused. However, given the gravity of the case and significant PAPS activity, we are inclined to determine focal segmental glomerulosclerosis in the context of a focal cortical atrophy, caused by probable renal infarctions. Furthermore, the patient presented with grade I obesity which, together with a decrease in renal mass, could bring about some degree of hyperfiltration.
Figure 1.
Figure 2.