Brown tumours (BT) in chronic kidney disease (CKD) are the result of high bone turnover, one type of renal osteodystrophy (ROD), which is caused by secondary hyperparathyroidism (HPT). BT lesions are characterised by the presence of multinucleated cells and brown haemosiderin deposits; this differentiate BT from osteitis fibrosa cystica (OFC) .BT has specific clinical presentation, with imaging and histopathology feature that are different from other disorders caused by HPT or renal osteodystrophy.1
This is a case of a 13-year-old male patient from a rural area of Loja in Ecuador. He had a history of CKD and symmetrical growth retardation. His symptoms began with chronic nocturnal pain in his left knee that was exacerbated by trauma. Anthropometric measurements showed that, a short stature, low weight and severe thinness (below Z score −3 of the median on the weight/age, height/age and BMI/age curves). Sexual infantilism was observed, in addition to little muscle mass in limbs and genu-valgus angular deformity (Fig. 1).
Description of the patient's brown tumour bone lesion. (A) Marked genu varus with mild left lower limb oedema. (B) AP X-ray of left knee, incomplete fracture zone of left femur distal epiphysis, with infiltrative radiopaque image. (C) CT of same anatomical area, solid osteolytic lesion 40mm×33mm in the distal femoral epiphysis, cartilage growth seems to be unaffected. (D) Processed tissue sample, large quantity of multinucleated cells. (E) MRI of same anatomical area, metaphyseal, irregular, heterogeneous, space-occupying process with compromise of bone and cortical portion centred in the distal femoral metaphyseal portion 35mm×33mm and with the presence of perilesional fluid; not compromising other structures. (F) Whole-body bone scan with 99mTc-sestaMIBI shows uptake of radiotracer in distal metaphysis of left femur. (G) 3-Dimensional tomographic view, lateral and posterior view of distal epiphysis of left femur. (H) Precise identification of the multinucleated giant cell, characteristic of brown tumour of bone.
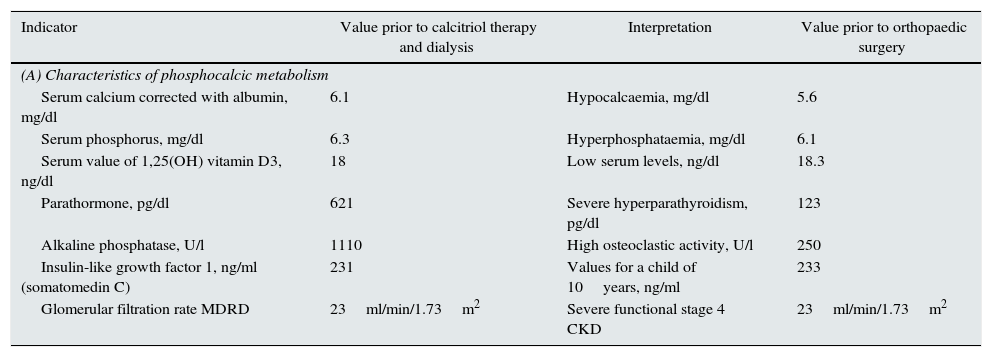
Further tests showed altered phosphorus/calcium metabolism (Table 1). Imaging and biopsy obtained with a Jamshidi® needle identified the BT (Fig. 1).
Description of phosphocalcic metabolism in the patient.
| Indicator | Value prior to calcitriol therapy and dialysis | Interpretation | Value prior to orthopaedic surgery |
|---|---|---|---|
| (A) Characteristics of phosphocalcic metabolism | |||
| Serum calcium corrected with albumin, mg/dl | 6.1 | Hypocalcaemia, mg/dl | 5.6 |
| Serum phosphorus, mg/dl | 6.3 | Hyperphosphataemia, mg/dl | 6.1 |
| Serum value of 1,25(OH) vitamin D3, ng/dl | 18 | Low serum levels, ng/dl | 18.3 |
| Parathormone, pg/dl | 621 | Severe hyperparathyroidism, pg/dl | 123 |
| Alkaline phosphatase, U/l | 1110 | High osteoclastic activity, U/l | 250 |
| Insulin-like growth factor 1, ng/ml (somatomedin C) | 231 | Values for a child of 10years, ng/ml | 233 |
| Glomerular filtration rate MDRD | 23ml/min/1.73m2 | Severe functional stage 4 CKD | 23ml/min/1.73m2 |
| (B) Characteristics of the CKD | |
|---|---|
| Mild microcytic hypochromic anaemia | |
| Elevated nitrogenous compounds: | |
| Urea 125mg/dl | |
| Creatinine 4.64mg/dl | |
| Proteinuria: | |
| Macroalbuminuria: albumin/creatinine ratio of 301.25mg/g | |
| Proteinuria: protein/creatinine ratio of 0.54mg/mg | |
CKD: chronic kidney disease; MDRD: modification of diet in renal disease.
Treatment included intravenous calcitriol (0.5–1μg) and dialysis. Once the parathyroid hormone (PTH) was reduced the patient had orthopaedic surgery.
The pseudoneoplasm is caused by proliferation of multinucleated giant cells and the mineral bone tissue is being replaced by fibrosis.2
The criteria used in diagnosis were: presence of hypocalcaemia and hyperphosphataemia and deficiency of 1,25(OH)3D related to secondary HPT (SHPT)3,4; multinucleated giant cells and haemosiderin coexistent with OFC5; thyroid and parathyroid gland with no structural alterations6; and no history of prolonged steroid therapy. His PTH values were greater than 120pg/l and he had no history of aluminium exposure, as opposed to a low-turnover ROD.3,4
Chronic pain triggered by trauma shows that the condition has gone unnoticed; when located in extremities it can cause night-time itching; in other cases, it starts with pathological fractures. The location is still the subject of much debate. SHPT does not follow a common pattern; lessions in the extremities, tend to affect hands phalanges.7 There are no reports in the literature of location in the femur. The differential diagnosis according to the location are: primary malignant tumours (osteosarcoma, chondrosarcoma and Ewing's tumour); primary benign tumours such as aneurysmal bone cyst; others such as multiple myeloma, solitary bone plasmacytoma, giant cell granuloma (Langerhans disease) and polyostotic fibrous dysplasia; secondary to infectious such as multifocal osteomyelitis; and other HPT-related disorders such as osteomalacia and rickets.7
Radiographical findings include subperiosteal cortical bone resorption and cystic changes, in addition to extraskeletal calcification and bone sclerosis.5 In our case, the subperiosteal lesion was limited to the bone and did not affect the soft tissue which is important to be different from osteosarcoma.
The coexistence of BT with CKD depends proportionally on PTH, and it is in stages 4 and 5 with PTH values greater than 250pg/ml that it occurs more frequently.7 While BT in adolescents with CKD 4 is poorly documented, the few cases reported involved children with primary HPT.5
Being a condition dependent on SHPT, management is focused on stabilising the PTH for subsequent orthopaedic correction. In cases of severe secondary HPT, surgical parathyroidectomy may be necessary to control PTH8 and experimental studies have evaluated the possibility of more advance therapies.9
In our case, we combined calcitriol and tri-weekly haemodialysis. However, the best measure is kidney transplantation, as this can restore expression of the genes encoding the VD receptors that are sensitive to calcium in the cells of a parathyroid gland with advanced Parathyroid hyperplasia.2
The other stage in the management was the orthopaedic intervention once the PTH was stabilised, achieving a reduction of 150pg/ml per month (Table 1). For the incomplete pathological fractures in the femur, surgical fixation and bone grafting are indicated.10
In conclusion, the atypical presentation presented is not only related with the location but also with the patient's age; in paediatric populations, bone lession is a criterion for starting dialysis, regardless of the glomerular filtration rate. The patient's prognosis is favourable, but the possibility of renal transplantation to prevent relapse and the development of further BT will have to be considered.
Please cite this article as: Alemán-Iñiguez JM, Mora-Bravo F, Bravo-Aguilar C. Rara localización de tumour pardo en paciente pediátrico. Nefrologia. 2016;36:560–562.