We present the case of a 54-year-old male with a history of IgA nephropathy that has progressed to stage 5 chronic kidney disease, for which he received a cadveric kidney transplant in 2011. His immunosuppression treatment included: tacrolimus, mycophenolate mofetil (MMF) and prednisone, and he had a baseline creatinine level of 2.11mg/dl. Two months prior to admission, he was started on treatment with corticosteroids at a dose of 1mg/kg, subsequently in tapering regimen, due to a recent diagnosis of borderline rejection.
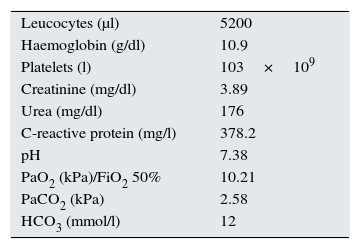
The patient was admitted to our hospital with respiratory failure in the context of bilobar pneumonia. Table 1 shows some of the patient's analytical parameters on admission.
The chest X-ray showed infiltrates in the right and left lower lobes. It was initially treated empirically with ceftriaxone and levofloxacin. Due to the poor clinical progress, the ceftriaxone was changed to meropenem, and the levofloxacin was withdrawn as the urinary antigen test for Legionella pneumophila (L. pneumophila) was negative. He was then also started on co-trimoxazole. The serial blood and sputum cultures obtained on admission were negative, as were the selective cultures for Legionella, Nocardia and fungi. The test for influenza A and B in nasopharyngeal aspirate was negative. Acid-fast bacillus staining and fluid and solid cultures also resulted negative. Quantitative PCR for the detection of cytomegalovirus in blood only revealed 93 CMV copies/ml.
Despite broad-spectrum antibiotic treatment, the patient remained febrile and had high oxygen requirements at day five after admission; thus, the treatment of immunosuppression with tacrolimus and MMF was discontinued. A bronchoscopy was performed with non-invasive ventilation, bronchoalveolar lavage (BAL) and tracheal aspirate were collected for cultures of conventional bacteria, Pneumocystis jirovecii, acid-fast bacilli and selective cultures for Legionella, Nocardia, fungi and mycobacteria.
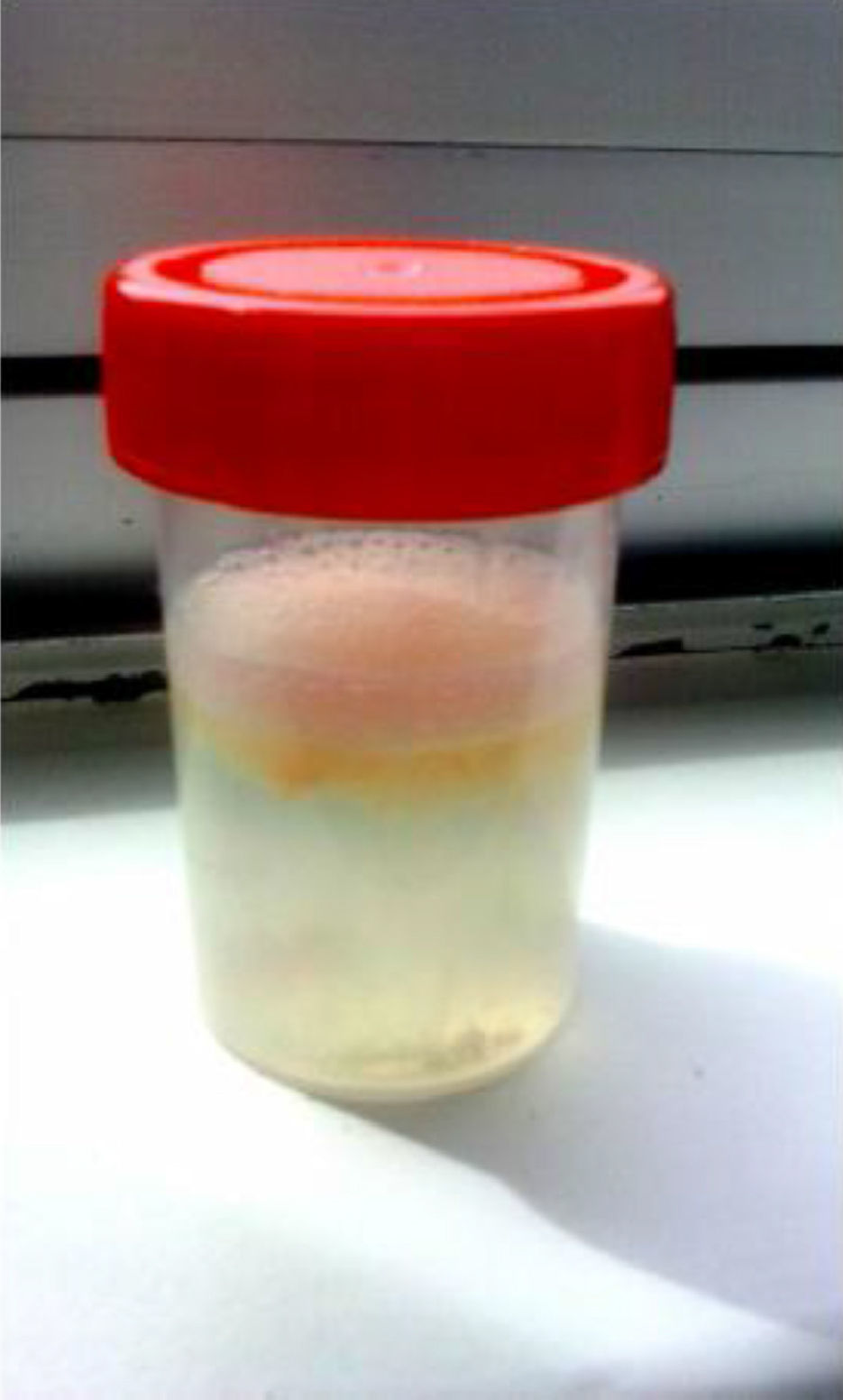
On day 10, the patient's general condition deteriorated, with high fever (39.3°C), coinciding with expectoration of a large amount of orange colour sputum (Fig. 1). We decided to add vancomycin and clindamycin to the treatment. Finally, on day 12 in hospital, colonies of Legionella micdadei (L. micdadei) were isolated in the BAL and tracheal aspirate cultures. All antibiotics were discontinued and treatment with levofloxacin was re-introduced for an additional 10 day period. The patient continued to have intermittent episodes of expectoration of large amounts of orange like sputum for a few more days but, ultimately, he made good clinical progress. It was possible to re-introduce the immunosuppressant treatment and his kidney function returned to previous levels.
DiscussionOne of the most common causes of undiagnosed community-acquired pneumonia is infection by Legionella spp.; L. pneumophila is responsible for around 85% of the cases of Legionella infection, with L. micdadei the second most common cause, responsible for 60% of infections by Legionella species other than L. pneumophila.1
Outbreaks of community-acquired pneumonia due to Legionella species other than L. pneumophila are uncommon,1,2 although the fact that culture and isolation of Legionella is so difficult means that the diagnosis is omitted in some cases. Infection by L. micdadei is more likely than L. pneumophila to be found in immunocompromised patients, and lower mortality rates have been reported.3
No differences in clinical presentation have been described between L. pneumophila and L. micdadei pneumonia. The gold standard test for diagnosis is the culture of respiratory secretions using Buffered Charcoal Yeast Extract (BCYE) agar. However, due to its viability and speed, detection of L. pneumophila serogroup 1 antigen in urine has become one of the methods most commonly used. The tests used, are able to detect the urinary antigen for all serogroups of L. pneumophila and some for other species, but the highest sensitivity is achieved with the detection of L. pneumophila serogroup 1 antigen.4
It has been reported that orange-like sputum in a patient with pneumonia is suggestive of infection by L. pneumophila. Fujita et al.5 put forward that the orange-coloured sputum is caused by factors released by L. pneumophila that interact with the tyrosine in the fluids in the epithelial lining.
In our case, we were dealing with an isolated case of community-acquired L. micdadei pneumonia in an immunosuppressed patient. Although the infection was originally being empirically covered with a quinolone, the negative urine test for Legionella led to us withdraw that treatment. However, that test has very low sensitivity for the diagnosis of Legionella infections other than L. pneumophila. For that reason, in the particular case of immunocompromised patients with pneumonia without alternative aetiology, we suggest that empirical treatment against Legionella spp. should not be discontinued until infection by species other than L. pneumophilia has been ruled out, or until the patient shows good progress with the conventional treatment.
FundingThis work was not funded.
Conflicts of interestThe authors have no conflicts of interest.
Please cite this article as: Soler-Majoral J, Sánchez-Escuredo A, Prat Aymerich C, Sanchis Vidal E, Marín-Tàpia A, Prats Bardají MS, et al. Esputo anaranjado en el contexto de neumonía por Legionella micdadei en un paciente trasplantado renal. Nefrologia. 2016;36:558–560.