For decades, radical nephrectomy (RN) has been considered the gold standard treatment for localised renal cell carcinoma. However, it has become evident that after RN, a significant number of solitary kidney patients have an increased risk of developing chronic kidney disease (CKD).1,2 Therefore, in situ ablation methods have been developed; radiofrequency ablation (RFA) is being the most used. In transplant patients, renal tumours represent 3% of all neoplasms.3
We present our preliminary experience of RFA treatment for small renal tumours (SRT) in transplant patients. The results revealed excellent tumour control without deterioration in renal function.
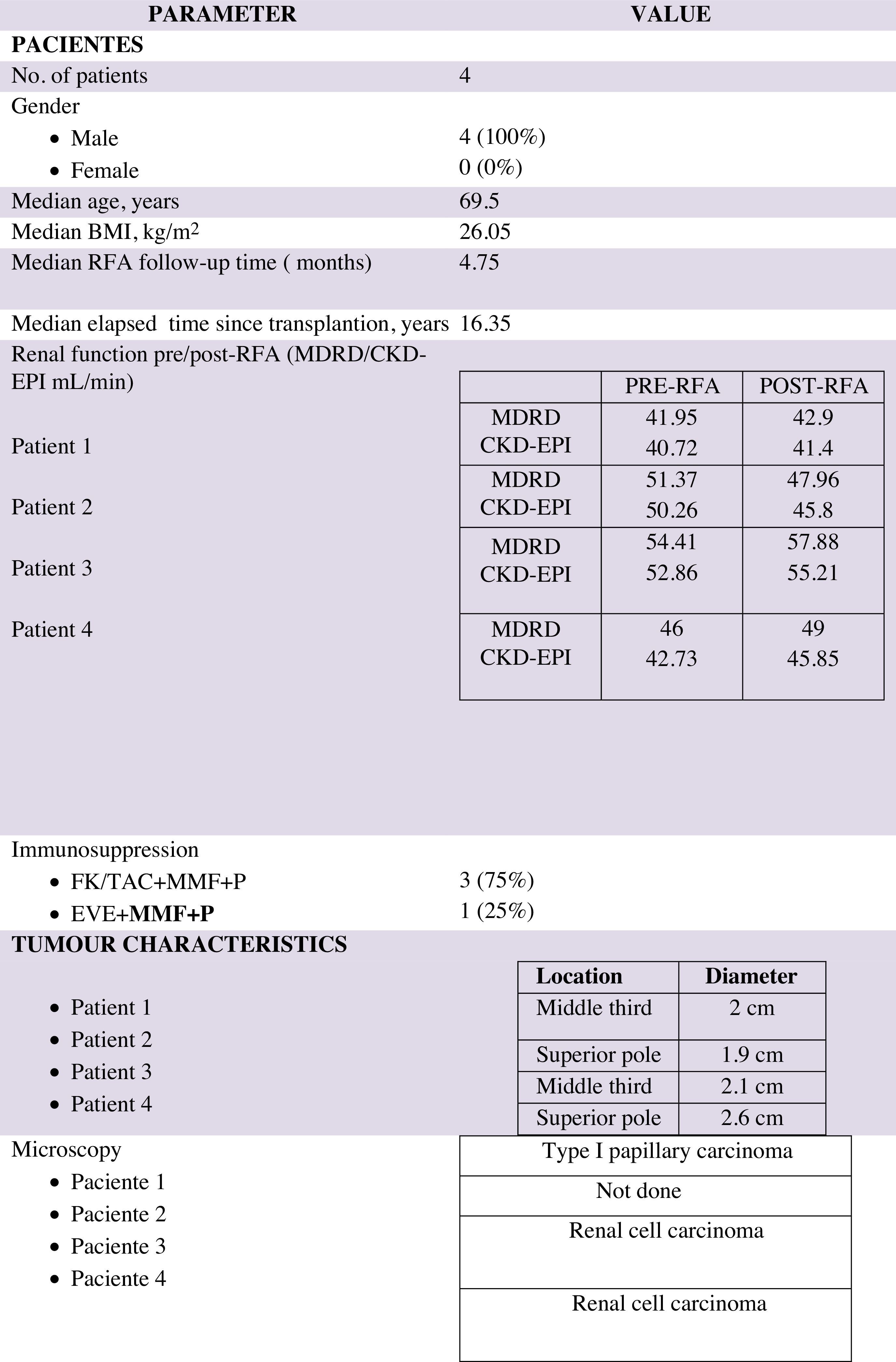
Out of 315 transplant patients being followed-up in our centre, with a median of 16.35 post-transplant years, 5 had renal tumours: 4 in native kidneys and 1 in a transplanted kidney. Only 1 patient had a radical nephrectomy of a native kidney, and the others were treated with RFA between September 2013 and December 2014. All lesions were detected by ultrasound, and were confirmed by with contrast-enhanced ultrasound. Staging was determined by computed tomography (CT) or magnetic resonance imaging (MRI). The demographic characteristics of the patients and the observed lesions are shown in Table 1. The comorbidities of the 4 solitary kidney patients with CKD were: 3 had dyslipidaemia, 2 had uncontrolled arterial hypertension and 1 had severe cardiovascular disease.
Percutaneous RFA was performed in the surgical room under general anaesthesia with ultrasound guidance, after ultrasound-guided fine needle aspiration biopsy of the tumour. Treatment was planned so as to obtain a healthy tissue ablation margin of 0.5–1cm width around the tumour to avoid recurrence, and contrast-enhanced ultrasound study was performed after completing treatment to assess the response, and if the case of incomplete tumour destruction, ablation was repeated.4
Patients remained in the hospital for 24h, and a follow-up abdominal ultrasound was performed before discharge, to confirm the absence of complications. Follow-up was at 1 month, then every 3 months during the first year, and every 6 months during the subsequent 2 years, which was when local recurrence was most common (Fig. 1). Follow-up included contrast-enhanced ultrasound, and CT or MRI if required. Success was defined as the absence of contrast in the arterial phase, indicating complete destruction of the tumour.
The mean duration of the procedure was 60min (range, 45–70min). The success rate was 100%. The median follow-up time was 4.75 months. There were no complications or incomplete ablations. Regarding microscopic examination, the patient with the transplanted kidney tumour had type I papillary carcinoma. The other patients, with native kidney tumours, had renal cell carcinomas. Only one patient did not have a biopsy because radiologically the tumour behaved like a renal cell carcinoma, and the patient elected to be treated percutaneously. In the follow-ups completed to date, no patients have shown local recurrence or distal metastases. None of the patients had significant changes in renal function pre- and post-RFA. In our series, the mean creatinine levels of the 4 patients before RFA and after a mean of 3.2 months of RFA were 1.51 and 1.57mg/dL, respectively.
The diagnosis of renal tumour is increasing in older patients with comorbidities and renal failure. Treatment requires techniques that preserve renal parenchyma. Several authors have described favourable experiences of RFA in SRT, in terms of both local tumour control and preservation of renal function.5–9
Three of our tumours measured less than 3cm; one tumour measured 3.1cm, which received 2 sessions of RFA in the same surgical procedure, for complete tumour ablation.
Tumours adjacent to the great vessels tend undergoes a “heat sink” effect, and conversely the ablative effect on exophytic tumours is higher, due to the insulating effect of surrounding perirenal fat that allows higher temperatures.5 In our series, 2 tumours were located in the superior pole and 2 in the middle third.
The success rate of RFA is 90–100%10; our patients had success in all treated tumours without local recurrence.5,8
ConclusionsRFA offers the advantage of being able to maintain patients’ renal function sufficiently to not require a dialysis programme, thus avoiding transplantectomy. Transplant patients with native kidney tumours do not have to undergo periodic radiological follow-up to assess tumour growth, and are able to continue their previously established immunosuppressive treatment.
Please cite this article as: Hernández-Socorro CR, Henríquez-Palop F, Santana-Toledo L, Gallego-Samper R, Rodríguez-Pérez JC. La ablación por radiofrecuencia como alternativa terapéutica al tratamiento de las neoplasias renales en pacientes trasplantados. Un estudio preliminar. Nefrologia. 2015;35:514–516.