Introducción: La biopsia renal percutánea (BRP) es una exploración invasiva fundamental para el estudio de enfermedades renales que lleva asociada una apreciable morbilidad. Estudios retrospectivos han mostrado que el 10-20 % de los casos presentan complicaciones menores y el 1,2-6,6 % complicaciones consideradas mayores. Sin embargo, este aspecto no ha sido examinado prospectivamente. Objetivo: El objetivo del estudio fue evaluar prospectivamente las complicaciones asociadas a la BRP en el riñón nativo. Métodos: Estudio prospectivo desde enero de 2009 hasta mayo de 2013 de las BRP realizadas por nefrólogos en riñón nativo bajo control ecográfico. Se analizaron variables clínicas y analíticas. Definimos complicación menor como la caída de la hemoglobina (Hb) de más de 1 g/dl y complicación mayor la necesidad de transfusión o técnica invasiva. Resultados: En este período se han realizado 241 BRP. La edad media de los pacientes fue de 49 años (± 17), la mayoría eran varones (56 %) y el 58,1 % padecían hipertensión arterial. Se realizaron dos punciones en el 51 %. Se observaron complicaciones menores en 46 pacientes (19,1 %) y mayores en 9 pacientes (3,7 %). En el análisis univariante, la Hb pre-BRP fue 10,3 g/dl (± 1,3) en aquellos que desarrollaron complicaciones mayores y 12,3 g/dl (± 2,2) en los demás (p = 0,003); en el análisis multivariante: OR 0,51, IC 95 %(0,2-0,9), p < 0,05. Conclusiones: La BRP es un procedimiento no exento de riesgos, ya que las complicaciones menores se presentaron en el 19,1 % y las mayores en el 3,7 % de los casos. La Hb pre-BRP es un factor de riesgo independiente para el desarrollo de complicaciones mayores.
Background: Percutaneous renal biopsy (PRB) is a key invasive technique in the study of kidney disease and it is associated with considerable morbidity. Retrospective studies have shown minor complications in 10%-20% and major complications in 1.2%-6.6% of cases. However, this aspect has not been studied prospectively. Objective: The aim of our study was to prospectively assess complications related to PRB in the native kidney. Methods: From January 2009 to May 2013, we prospectively analysed PRB performed by nephrologists in native kidneys under ultrasound guidance. We analysed clinical and laboratory variables. We defined minor complications as the decrease in haemoglobin (Hb) of more than 1g/dL and major complications as the need for a transfusion or invasive technique. Results: 241 PRB were performed over this period. The mean patient age was 49 years (±17), the majority (56%) were male and 58.1% had high blood pressure. In 51% of cases, we carried out 2 punctures. There were minor complications in 46 patients (19.1%) and major complications in 9 patients (3.7%). In the univariate analysis, pre-PRB Hb was 10.3g/dL (±1.3) in patients with major complications and 12.3g/dL (±2.2) in the remaining patients (p=.003); in the multivariate analysis: OR 0.51, 95% CI (0.2-0.9), p<.05. Conclusions: PRB is a procedure that is not without risk, since minor complications occurred in 19.1% and major complications in 3.7% of cases. Pre-PRB Hb is an independent risk factor for the development of major complications.
INTRODUCTION
Percutaneous renal biopsy (PRB) is a key diagnostic technique in the study of kidney disease, mainly in glomerular pathology. However, it is an invasive examination associated with considerable morbidity and which must be indicated on an individualised basis. As a result, there may be bleeding, haematomas, arteriovenous fistulae, high blood pressure (HBP), infection, puncture or damage to other organs and even death. There is a higher incidence of complications when the patient has HBP, a clotting disorder, small kidneys or cortical thinning1-3.
Minor complications occur in 10%-20% and major complications occur in 1.2%-6.6% of cases, according to European and American series4-8. This information is provided by old retrospective studies carried out by different medical teams (radiologists, nephrologists or urologists) using various media. Ultrasound use has been implemented in most centres in recent years. Patients are increasingly demanding more accurate and up-to-date information about the complications associated with invasive procedures.
The objective of our study was to prospectively assess the complications associated with PRB in native kidneys performed under ultrasound guidance by the nephrology team.
METHODS
We carried out a prospective study of the PRBs performed on native kidneys in our hospital from January 2009 to May 2013.
PRBs were carried out after the ultrasound was performed to locate the lower pole of the left kidney. To take samples, we used 16 Gauge semi-automatic needles, with a maximum of four attempts, and always under ultrasound guidance. We performed real-time ultrasound-guided biopsies3,9. The procedure was led and performed by the Nephrology team (generally a resident physician and a Nephrology specialist), without the participation of the Radiology or Urology teams.
The study variables were the following: baseline characteristics: sex, age and HBP; laboratory parameters: Pre- and post-PRB haemoglobin (Hb) and creatinine and proteinuria/24hr; and technique variables: number of punctures, minor and major complications, post-PRB low blood pressure, macroscopic haematuria, imaging tests and desmopressin administration. We indicated desmopressin use on an individualised basis in patients with stage IV-V renal failure and/or severe liver disease. We administered a dose of 0.4µg/kg for approximately 30 minutes before performing PRB. As regards complications associated with PRB, we classified minor complications as a decrease in Hb of more than 1g/dl and major complications as the need for post-PRB transfusion, arteriogram, embolisation, surgery or the occurrence of patient death.
At the time of the biopsy, each patient showed normal clotting and had discontinued, at least one week before, antiplatelet therapy or non-steroidal anti-inflammatory drugs. The PRB indications were individualised.
RESULTS
We performed 241 PRBs on native kidneys between January 2009 and May 2013. The mean age of the patients was 49 years old (±17), the majority were male (56%) and 58.1% had HBP.
With regard to the laboratory parameters, mean serum creatinine was 2.9mg/dl (±4.7), proteinuria was 2.3g/24h (±3.5), pre-PRB Hb was 12.2g/dl (±2.2) and post-PRB Hb was 11.9g/dl (±2.3).
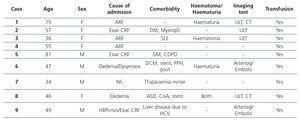
We carried out two punctures in 51% of cases. There was post-PRB low blood pressure in 10.8% and macroscopic haematuria in 5.8% of cases. We observed minor complications in 46 patients (19.1%) and major complications in 9 patients (3.7%), with imaging tests being performed in 5% of cases. There were no technique-associated complications in 186 patients (77.2%). Of the 241 patients included in the study, only 9 developed major complications, 4 were male and 5 female, between 34 and 81 years of age. All 9 received a post-biopsy blood transfusion (3.7%) and 2 required an arteriogram and embolisation (0.8%). The latter two had predisposing factors for bleeding: one of them was a patient with a stent that required antiplatelet therapy and the other had chronic liver disease (Table 1). In 21 patients (8.7%), we administered desmopressin due to stage IV-V renal failure and/or severe liver disease. The mean age of this group was 58.7±14.1 years old and mean serum creatinine was 6.2±4.1mg/dl, which were both significantly higher than in the remaining patients (p=.005 and p<.001 respectively). Furthermore, two of them (9.5%) had a major bleeding complication, which required a blood transfusion.
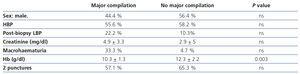
In the univariate analysis, patients who developed major complications had significantly lower pre-biopsy Hb than those who did not (Hb 10.3±1.3g/dl versus 12.3±2.2g/dl, respectively (P=.003). However, no relation was found with the other variables: sex, HBP, post-biopsy low blood pressure, serum creatinine, macrohaematuria and number of punctures (Table 2). None of these variables were associated with the development of minor complications in the univariate analysis (data not shown).
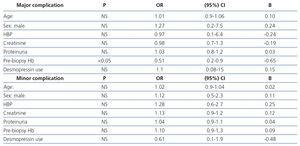
With regard to the multivariate analysis, only pre-biopsy Hb was an independent risk factor for developing major complications. Furthermore, none of the variables analysed (age, sex, HBP, serum creatinine, proteinuria, pre-biopsy Hb and desmopressin) were considered independent risk factors for developing minor complications (Table 3).
DISCUSSION
According to the results of this prospective study, we can observe that PRB is associated with a minor complication rate of 19.1% and a major complication rate of 3.7%. This information is necessary, since patients are demanding increasingly accurate and up-to-date information about the complications associated with invasive procedures. We should also bear in mind that the procedure has changed in recent years (increasingly fewer nephrologists perform it, normally with ultrasound guidance and using needles of a certain gauge).
The incidence of minor complications (19.1%) is similar to that previously published in the literature: 10%-20%4-8. These basically consist of decreases in Hb of more than 1g/dl, usually with no clinical consequences. These decreases in Hb are usually the expression of a small perirenal haematoma. Our results are probably at the higher limit due to the nature of data collection in a prospective study.
In retrospective studies, the major complication rates reported are 1.2%-6.6%4-8, with the figure in our study being 3.7% despite the fact that we included the requirement for a post-biopsy transfusion independently of whether or not another invasive technique was performed (arteriogram, embolisation, nephrectomy). All of the 9 patients who developed major complications received a post-PRB transfusion and only two had another complication (arteriogram and embolisation), and as such, if we excluded transfusions as a major complication criterion, the figure would be only 0.8% in our series (Table 1). We must highlight that there were no deaths, despite mortality secondary to this procedure having been estimated at 1/1000 cases1,2. In recent years, this procedure has become safer and we have achieved a significant reduction in the technique-associated death rate8,10,11.
These data must be related (as well as to the patients’ clinical characteristics) to factors involved in the procedure; that is, the experience of the doctor performing it, whether or not it is performed with ultrasound guidance and the needle gauge.
Few studies by nephrologists have analysed the complications associated with PRB in their centres5,8,12-14, among other reasons, because they do not always perform these procedures themselves. According to a survey carried out in Spain on tutors of Nephrology resident physicians in 2012, in 49% of cases, these procedures are performed by nephrologists themselves, in 42% by an external doctor and in 9% by others. In addition, in recent years, we have observed that the number of renal biopsies performed by nephrologists has continued to decrease (60% in 2007 versus 49% en 2012)15.
We always performed PRB under real-time ultrasound guidance and, although there are no current data in this regard, this is probably the case in most centres8.
Another aspect that influences complications from biopsies is the needle gauge. According to our experience, the use of 16 Gauge semi-automatic needles in comparison with those of 18 Gauge does not increase complications, but it does improve diagnostic efficiency5. Some authors report the use of 14 Gauge needles with better performance and without increasing complications16. However, others indicate that 14 Gauge semi-automatic devices are associated with an increased risk of bleeding after the procedure, and as such, the use of needles with a smaller gauge is recommended11,17. It is important to discontinue antiplatelet treatment prior to conducting PRB as this will lower the complication rate18.
The technique must be performed in the most suitable and safest way possible. We use 16 Gauge semi-automatic needles and carry out PRB under real-time ultrasound guidance. Furthermore, as an additional preventive measure, the patient is in complete bed rest for 24 hours9, we carry out blood pressure tests (every hour for the first 5 hours), we measure diuresis (we observe the characteristics of urine) and we carry out a blood test with a blood count. Post-PRB bleeding increases hospital costs; as such, we assess the pre-PRB administration of desmopressin in order to decrease the risk of bleeding and the size of the haematoma in patients who will undergo this procedure19. We used it in 21 patients (8.7%). However, two of them (9.5%) had a major bleeding complication and required a blood transfusion. As was expected, this patient group, despite prophylaxis with desmopressin, had a considerably higher complication rate (9.5%) than that of the general population (3.7%).
In conclusion, PRB continues to be a procedure that is not without risks, since minor complications occurred in 19.1% and major complications occurred in 0.8-3.7% of cases. Pre-PRB Hb is an independent risk factor for the development of major complications. It is necessary to carry out a risk-benefit assessment in each patient for an individualised indication of PRB.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Clinical characteristics of patients with major complications.
Table 2. Correlation of clinical variables with the occurrence of major complications (univariate analysis).
Table 3. Logistic regression analysis for the occurrence of major and minor complications.