Preimplantation renal biopsy provides potentially valuable information about post-transplant renal function.
ObjectiveTo assess the prognostic value of preimplantation kidney biopsy from older donors in determining 1-year post-transplant estimated glomerular filtration rate MDRD-4 (eGFR).
MethodsWe evaluated a cohort of 124 renal transplant recipients from deceased donors ≥60 years old, performed at our centre between March 2008 and May 2012. Biopsies were assessed by applying the score proposed by O’Valle et al. The overall score was stratified into 3 levels: 0–3, 4–5 and 6–8 points. Kidneys scoring >8 points were discarded. A total of 77% of the donors were ≥70 years.
ResultsOne year post-transplant, mean eGFR (SD) was lower in transplant recipients with 6–8 points (38.5 [14.1]ml/min/1.73m2) than in the group scoring 4–5 points (46.3 [15.7] [p=0.03]) and the group scoring 0–3 (49.6 [12.5] [p=0.04]). Seven patients (19%) had eGFR <30ml/min/1.73m2 1 year post-transplant in group 6–8 vs 8 (14%) in group 4–5 and none in group 0–3. In the logistic regression, OR (95% IC), to determine patients with 1-year post-transplant eGFR (<30ml/min/1.73m2), delayed graft function (6.3 [1.9–21.3]) and acute rejection (5.8 [1.1–31]), were significant. The adjusted OR of biopsy score group 6–8 vs 0–5, was 2.2 (0.7–7.3).
ConclusionsAllografts with higher pathologic score in preimplantation renal biopsy were associated with a worse 1-year post-transplant eGFR. Delayed graft function and acute rejection were significant risk factors for 1-year post-transplant low eGFR.
La biopsia renal preimplante puede aportar información útil evolutiva postrasplante.
ObjetivoAnalizar el valor pronóstico de la biopsia renal de donantes de edad avanzada respecto al filtrado glomerular estimado MDRD-4 (FGe) al año del trasplante.
MétodosEstudiamos a 124 receptores de trasplante renal de donantes fallecidos de ≥60 años, con biopsia renal preimplante. Los trasplantes fueron realizados en nuestro centro, entre marzo del 2008 y mayo del 2012. Las biopsias se valoraron según el baremo propuesto por O’Valle et al. y se categorizaron en 3 grupos: 0-3, 4-5, 6-8 puntos. Se descartaron los riñones con una puntuación >8. El 77% de los donantes tenía ≥70 años.
ResultadosEl FGe medio (DE) del grupo 6-8 al año del trasplante: 38,5 (14,1) mL/min/1,73m2 fue menor que el del grupo 4-5: 46,3 (15,7) (p=0,03) y del grupo 0-3: 49,6 (12,5) (p=0,04). Se registraron 7 (19%) pacientes con FGe<30mL/min/1,73m2 en el grupo 6-8 vs. 8 (14%) en el grupo 4-5 y ninguno en el grupo 0-3 (p=0,17). En el análisis de regresión logística, OR (IC 95%), que valoró los pacientes con FGe<30mL/min/1,73m2 al año del trasplante, la función retrasada del injerto (6,3 [1,9-21,3]) y el rechazo agudo (5,8 [1,1-31]) fueron significativos. La puntuación del daño histológico de las biopsias, grupo 6-8 vs. 0-5, presentó un OR ajustado no significativo de 2,2 (0,7-7,3).
ConclusionesLos riñones con mayor afectación histológica presentaron un menor FGe al año del trasplante. La función renal retrasada del injerto y el rechazo fueron factores de riesgo significativos de un bajo FGe al año del trasplante.
Kidney transplant represents the best option for replacement kidney therapy for patients who develop advanced chronic kidney disease. However, the supply of young donors, who are theoretically ideal, is limited, and does not cover the demand among patients on the waiting list for a kidney transplant. This imbalance has resulted in the growing use of older donors, often with associated morbidity such as hypertension and diabetes. Good clinical results are obtained with these organs provided that these grafts are suitably and receptors are adequate.1–4
Several scales have been developed with the aim of assessing the quality of donors’ kidneys and to determine their viability and post-transplant function. The Organ Procurement and Transplantation Network/United Network for Organ Sharing (OPT/UNOS) defined the concept of expanded donor criteria, but the prognostic utility of these criteria is limited, as the concept takes into consideration heterogeneous clinical profiles with different clinical outcomes.5,6 Other indexes stratify graft survival more precisely, but have a moderate discriminatory value.7–11 The donor's kidney biopsy provides information that may improve the prediction of functional outcome. However, the results that have been published are controversial and have not been widely used.12,13
At Hospital Universitario Cruces in 2008, kidney biopsy of deceased older donors was incorporated into the protocol to ensure the quality of the kidney grafts being used. This study analysed the clinical results obtained and specifically assessed the relationship between histological lesions and glomerular filtration rate one year after transplant.
Patients and methodsStudy designA retrospective cohort study of 124 kidney transplant recipients. The transplants were performed at our centre between March 2008 and May 2012, with grafts from donors ≥60 years of age deceased of brain death, with a preimplantation kidney biopsy. Clinical course data was collected until May 2013, or death or graft loss in case that one of these occurred prior to that time.
Donor kidney biopsyA biopsy was performed in all donors ≥70 years of age and in those 60–69 years of age with a prior history of HTA or diabetes. In all cases, macroscopic state of the kidneys was adequate and the MDRD-4 estimated glomerular filtration rate (eGFR) was >60ml/min/1.73m2. Wedge biopsies were performed to obtain kidney samples, which were manually embedded in paraffin. Fixation in formaldehyde was speeded, when necessary, in an oven at 60–70°C. The samples were sliced to 3–4μm and stained with haematoxylin–eosin and periodic acid–Schiff. Histological lesions were assessed by one of a team of 5 pathologists at our centre by using the scale proposed by O’Valle et al.14,15 (Table 1). Kidneys with a cumulative score >8 and those with a partial assessment of 3 in lesions of glomerulosclerosis, hyaline arteriolopathy or myointimal elastosis were discarded. Kidneys with a score >5 were allocated to recipients >60 years of age. All others were considered to be fit for any adult recipient. In the study period, a total of 39 grafts were discarded as they did not fullfill to the histological criteria established.
Pre-implantation histological kidney lesion scoring.
| Glomerulosclerosis |
| 0. Absence |
| 1. 0%–10% |
| 2. 11%–20% |
| 3. >20% |
| Glomerular capsular fibrosis |
| 0. Absence |
| 1. 0%–15% |
| 2. 16%–40% |
| 3. >40% |
| Cystic glomeruli |
| 0. Absence |
| 1. 0%–15% |
| 2. 16%–40% |
| 3. >40% |
| Hyaline arteriolopathy |
| 0. Absence |
| 1. Non-occlusive in <50% of arteries |
| 2. Non-occlusive in >50% of arteries |
| 3. Occlusive in >50% of arteries |
| Myointimal elastosis |
| 0. Absence |
| 1. Thickening of the intima that reduces the lumen >0%–20% |
| 2. Thickening of the intima that reduces the lumen >21%–50% |
| 3. Thickening of the intima that reduces the lumen >50% |
| Tubular atrophy |
| 0. Absence |
| 1. Atrophy <4/20 fields (×40) |
| 2. Atrophy 4–10/20 fields (×40) |
| 3. Atrophy >10/20 fields (×40) |
| Interstitial fibrosis |
| 0. Absence |
| 1. Fibrosis <3/20 fields (×40) |
| 2. Fibrosis 3–8/20 fields (×40) |
| 3. Fibrosis >8/20 fields (×40) |
Quadruple initial therapy with corticosteroids, mycophenolic acid, tacrolimus and induction with two 20mg doses of basiliximab intravenously was prescribed for days +0 and +4 from the transplant. 6-Methyl-prednisolone, 125mg IV was administered during the surgical procedure, 60mg/day were administered intravenously during the first 3 days and then 30mg/day of prednisone was given orally with a subsequent progressive reduction down to 5mg/day in the first 3 months. The initial dose of tacrolimus was 0.1mg/kg/day orally, with subsequent adjustments to maintain levels of 6–8ng/ml. Patients also received 1500mg/day of mycophenolate mofetil or 1080mg/day of mycophenolate sodium orally in 3 doses. Episodes of acute rejection were treated with boluses of 250mg of 6-methyl-prednisolone intravenously for 3 consecutive days.
Definition of variablesThe following donor variables were included in the study: age, gender, weight, height, creatinine on admission and prior to blood draw, HTA, diabetes, cause of death, score for each individual histological component, and cumulative score for histological lesions. The following recipient variables were included: age, gender, cause of kidney disease, method of replacement treatment prior to transplant, previous transplants and historical and current rate of panel reactive antibodies (PRA). The following baseline and evolutionary transplant variables were included: HLA A-B-DR incompatibilities, cold ischaemia, delayed graft function, acute rejection, death, restart of dialysis, tacrolimus and creatinine levels (first month, 3 months, a year, 2 years and 3 years), and proteinuria/creatinine ratio one year after transplant.
Delayed graft function was defined as a need for dialysis in the first week after transplant. The date of the last dialysis session was accepted as the initiation of functional recovery. Clinical episodes treated with IV boluses of 6-methyl-prednisolone were recorded as acute rejections. The cumulative score for histological lesions was categorised arbitrarily, but to optimise statistical analysis, there were classified into 3 groups: 0–3 points, 4–5 points and 6–8 points.
The primary outcome variable was glomerular filtration rate one year after transplant, which was estimated by means of the MDRD-4 equation. Its mean value, its categorical distribution (<30, 30–59, ≥60ml/min/1.73m2) and the incidence of patients with an eGFR<30ml/min/1.73m2 were analysed.
Statistical analysisQuantitative variables were described using the mean and standard deviation (SD) or median and quartiles (Q1–Q3) in case of a non-normal distribution. Categorical variables were expressed in terms of absolute frequencies and percentages. The association between categorical variables were analysed using the chi-squared test or Fisher's exact test, according to the expected values. Graft survival was estimated using the Kaplan–Meier method. Mean eGFRs one year after transplant for the histological groups were 0–3 points, 4–5 points and 6–8 points. They were compared by means of the ANOVA test, with post hoc comparisosns, if in the overall test was p<0.05. The relationship between histological score and incidence of patients with an eGFR<30ml/min/1.73m2 one year after transplant was assessed using logistic regression analysis. In the univariate analysis, the histological score and the clinical variables potentially influencing this result were assessed. In the multivariate model, the histological score, which remained fixed, and the variables that had a p<0.20 in the univariate analysis were assessed. The variables with a higher p-value were progressively removed from the model until a model was obtained in which all the predictive variables showed a p<0.05. Statistical analyses were performed with the IBM-SPSS 20.0 program.
ResultsTable 2 shows the clinical and demographic characteristics of the study patients. 77% of donors were ≥70 years of age; 45% had HTA, and 14% had diabetes. 89% of recipients were ≥60 years of age. The eGFR of all the donors was >60ml/min/1.73m2. Table 3Table 3 specifies the distribution of histological lesions from the preimplantation kidney biopsies. These showed a median (Q1–Q3) of 48 glomeruli (32–71) and 2 arteries (1–3). No arteries were visualised in 11 biopsies (9%). In total, 19 biopsies (15%) obtained a score of 0–3 points, 63 biopsies (51%) obtained a score of 4–5 points and 42 biopsies (34%) obtained a score of 6–8 points.
Baseline, clinical and demographic characteristics of transplant donors and patients.
| Variable | Total transplants, N=124 |
|---|---|
| Donor's age (years) | |
| Mean (SD) | 72.5 (4.9) |
| 60–69 | 29 (23) |
| 70–80 | 95 (77) |
| Male donors, N (%) | 53 (43) |
| Donor's cause of death, N (%) | |
| Cerebral haemorrhage | 107 (86) |
| Traumatic brain injury | 10 (8) |
| Other | 7 (6) |
| Donors with a prior history of HTA, N (%) | 56 (45) |
| Donors with a prior history of diabetes, N (%) | 17 (14) |
| Donor's creatinine, mg/dl, mean (SD) | 0.67 (0.17) |
| Donor's MDRD-4 glomerular filtration rate, ml/min/173m2, mean (SD) | 107 (28) |
| Recipient's age (years) | |
| Mean (SD) | 66.8 (6.3) |
| <60 | 14 (11) |
| 60–69 | 68 (55) |
| 70–79 | 42 (34) |
| Male recipients, N (%) | 84 (68) |
| Cause of kidney disease, N (%) | |
| Unknown | 29 (23) |
| Glomerular | 21 (17) |
| Vascular | 22 (18) |
| Polycystitis | 23 (19) |
| Diabetes | 10 (8) |
| Other | 19 (15) |
| Method of dialysis, N (%)a | |
| Haemodialysis | 82 (71) |
| Peritoneal dialysis | 36 (29) |
| Time in pre-transplant dialysis, months, median (Q1–Q3) | 26 (17–41) |
| Recipient's current PRA, N (%) | |
| Negative | 104 (84) |
| 1–50 | 17 (14) |
| 51–100 | 3 (2) |
| Patients with previous kidney transplant, N (%) | 12 (10) |
| HLA A-B-DR incompatibilities, N (%) | |
| 0–2 | 23 (19) |
| 3–4 | 92 (74) |
| 5–6 | 9 (7) |
| Cold ischaemia, hours, mean (SD) | 18.4 (3.3) |
| Biopsy score, N (%) | |
| 0–3 | 19 (15) |
| 4–5 | 63 (51) |
| 6–8 | 42 (34) |
Distribution of histological lesions from preimplantation kidney biopsies.
| Type and grade of histological lesions | Total biopsies, N=124 (%) |
|---|---|
| Glomerulosclerosis | |
| 0 | 11 (9) |
| 1 | 85 (68) |
| 2 | 27 (22) |
| 3 | 1 (1) |
| Capsular fibrosis | |
| 0 | 81 (65) |
| 1 | 42 (34) |
| 2 | 1 (1) |
| 3 | 0 |
| Cystic glomeruli | |
| 0 | 83 (67) |
| 1 | 38 (30) |
| 2 | 2 (2) |
| 3 | 1 (1) |
| Hyaline arteriolopathy | |
| 0 | 83 (67) |
| 1 | 40 (32) |
| 2 | 1 (1) |
| 3 | 0 |
| Myointimal elastosis | |
| 0 | 25 (20) |
| 1 | 77 (62) |
| 2 | 11 (9) |
| 3 | 0 (0) |
| Not available | 11 (9) |
| Tubular atrophy | |
| 0 | 8 (7) |
| 1 | 107 (86) |
| 2 | 9 (7) |
| 3 | 0 |
| Interstitial fibrosis | |
| 0 | 19 (15) |
| 1 | 99 (80) |
| 2 | 6 (5) |
| 3 | 0 |
Table 4Table 4 shows both the overall results and the results obtained in each of the histological categories. Following transplantation, 68% of grafts functioned immediately, 8% never functioned and all others functioned after a mean of 10 days. A total of 8% of patients received boluses of corticosteroids due to a suspicion of acute rejection. Four patients (3%) died during the first year after the transplant. A total of 14 patients (11%) lost the graft in that period of time, in 8 cases due to arterial or venous graft thrombosis (4 from the 6–8 histological group and the other 4 from the 4–5 histological group). Four patients from the 6–8 histology group lost the graft with evidence of fibrosis, tubular atrophy and non-specific chronic vascular lesions. Overall survival for the grafts, excluding deaths, was 89% after the first and second year and 84% after the third year.
Overall and grouped post-transplant clinical outcomes according to histological biopsy score.
| Results | Biopsy score | Total | ||
|---|---|---|---|---|
| 0–3 | 4–5 | 6–8 | ||
| No. of transplants | 19 | 63 | 42 | 124 |
| Immediate graft function, N (%) | 14 (74) | 45 (71) | 25 (60) | 84 (68) |
| Clinical rejections in the first year, N (%) | 1 (5) | 7 (11) | 2 (5) | 10 (8) |
| Deaths in the first year,. N (%) | ||||
| Infectious causes | 0 | 3 (5) | 0 | 3 (2) |
| Pancreatitis | 1 (5) | 0 | 0 | 1 (1) |
| Total | 1 (5) | 3 (5) | 0 | 4 (3) |
| Graft losses in the first year, N (%) | ||||
| Graft thrombosis | 0 | 4 (6) | 4 (10) | 8 (6) |
| Surgical bleeding | 0 | 0 | 1 (2) | 1 (1) |
| Haemolytic-uraemic syndrome | 0 | 0 | 1 (2) | 1 (1) |
| Fibrosis and tubular atrophy | 0 | 0 | 4 (10) | 4 (3) |
| Total | 0 | 4 (6) | 10 (24) | 14 (11) |
| Graft survival, excluding deaths. N at risk (survival [%]) | ||||
| Month 12 | 18 (100) | 56 (93.7) | 32 (76.2) | 106 (89) |
| Month 24 | 14 (100) | 33 (93.7) | 15 (76.2) | 62 (89) |
| Month 36 | 12 (100) | 27 (84.8) | 6 (76.2) | 45 (84) |
The relationship between the score obtained in the pre-implantation kidney biopsy and eGFR one year after transplant was analysed in 110 patients. A total of 14 patients were discarded from the analysis: Four due to death in the first year post-transplant, 8 because graft thrombosis, one due to haemolytic-uraemic syndrome and one owing to graft loss associated with post-operative bleeding. A total of 4 patients from the 6–8 group who lost the graft with already reported lesions from fibrosis and tubular atrophy were included. These patients were assigned a filtration rate of 10ml/min/1.73m2 one year after transplant. Eighteen patients (16%) obtained a cumulative score of 0–3 points, 56 patients (51%) obtained values of 4–5 points and 36 patients (33%) obtained an assessment of 6–8 points. The biopsies showed a median (Q1-Q3) of 48 glomeruli (33–73) and 2.3 arteries (1–3). No arteries were visualised in 9 biopsies (8%). The age of the donors with a score of 6–8 was greater than all other groups, without significant differences being recorded in any of the other baseline clinical or demographic characteristics analysed. Regarding clinical outcomes, the incidence of patients with delayed graft function was 4 (22%) in the 0–3 group, 14 (25%) in the 4–5 group and 11 (31%) in the 6–8 category (p=0.80). The time of initiation of graft function was similar in the 3 groups. Nine patients had acute rejection: one (6%), 6 (11%) and 2 (6%), in the 0–3, 4–5 and 6–8 groups respectively (p=0.72). Graft survival 3 years after transplant, excluding deaths, was 100% in the 0–3 group, 91% in the 4–5 group and 89% in the 6–8 group (Table 5Table 5).
Clinical characteristics of the 110 transplants included in the post-transplant renal function analysis.
| Variable | Biopsy score | p | ||
|---|---|---|---|---|
| 0–3 | 4–5 | 6–8 | ||
| No. of transplants (%) | 18 (16) | 56 (51) | 36 (33) | |
| Donors’ age, years, mean (SD) | 71.4 (4.3) | 71.3 (5.3) | 74.3 (3.9) | 0.01 |
| Male donors, N (%) | 5 (28) | 20 (35) | 15 (42) | 0.45 |
| Donors’ cause of death, N (%) | ||||
| Cerebral haemorrhage | 16 (89) | 52 (93) | 27 (75) | 0.06 |
| Traumatic brain injury | 0 | 2 (3.5) | 6 (17) | |
| Other | 2 (11) | 2 (3.5) | 3 (8) | |
| Donors with a prior history of HTA, N (%) | 7 (39) | 25 (45) | 18 (50) | 0.72 |
| Donors with a prior history of diabetes, N (%) | 0 | 8 (14) | 7 (19) | 0.11 |
| Donor's creatinine, mg/dl, mean (SD) | 0.61 (0.10) | 0.65 (0.16) | 0.71 (0.19) | 0.11 |
| Donor's MDRD-4 glomerular filtration rate, ml/min/1.73m2, mean (SD) | 112 (22) | 109 (28) | 105 (30) | 0.64 |
| Cold ischaemia, hours, mean (SD) | 18.7 (2.9) | 18.3 (3.8) | 18.4 (3.4) | 0.95 |
| Recipients’ age, years, mean (SD) | 64.8 (6.2) | 66.9 (6.4) | 67.7 (6.3) | 0.28 |
| Male recipients, N (%) | 10 (56) | 38 (68) | 28 (78) | 0.25 |
| Retransplants, N (%) | 3 (17) | 5 (9) | 2 (6) | 0.44 |
| HLA A-B-DR incompatibilities, N (%) | ||||
| 0–2 | 4 (22) | 13 (23) | 3 (8) | 0.08 |
| 3–4 | 11 (61) | 40 (72) | 32 (89) | |
| 5–6 | 3 (17) | 3 (5) | 1 (3) | |
| Current PRA, N (%) | ||||
| Negative | 15 (83) | 50 (89) | 31 (86) | 0.36 |
| 1–50 | 3 (17) | 6 (11) | 3 (8) | |
| >50 | 0 | 0 | 2 (6) | |
| Method of dialysis, N (%) | ||||
| Haemodialysis | 10 (56) | 40 (71) | 28 (78) | 0.23 |
| Peritoneal dialysis | 8 (44) | 16 (29) | 8 (22) | |
| Delayed graft function, N (%) | 4 (22) | 14 (25) | 11 (31) | 0.80 |
| Time of start of effective function, days, mean (SD) | 10.7 (5.6) | 10.5 (6.1) | 9.1 (6.9) | 0.84 |
| Clinical rejection in the first year, N (%) | 1 (6) | 6 (11) | 2 (6) | 0.72 |
| Graft survival, excluding deaths. N at risk (survival [%]) | ||||
| Month 12 | 18 (100) | 56 (100) | 32 (89) | 0.14a |
| Month 24 | 14 (100) | 33 (100) | 15 (89) | |
| Month 36 | 12 (100) | 27 (91) | 6 (89) | |
| Month 12 proteinuria/creatinine, N (%) | ||||
| <0.3 | 14 (78) | 34 (62) | 22 (73.3) | 0.63 |
| 0.3–1 | 4 (22) | 16 (29) | 7 (23.3) | |
| >1 | 0 | 5 (9) | 1 (3.3) | |
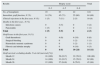
Regarding eGFR, the primary study outcome, statistical differences were detected. Mean (SD) eGFR for the 6–8 group (38.5 [14.1]ml/min/1.73m2) was lower than that reached in the group with a score of 4–5 (46.3 [15.7]ml/min/1.73m2 [p=0.03]) and that achieved in the 0–3 group (49.6 [12.5]ml/min/1.73m2 [p=0.04]). Similarly, a significant correlation (p=0.04) was detected between biopsy score and categorical distribution of eGFR one year after transplant. Patients with a higher score had a more unfavourable distribution (Table 6Table 6).
Association between score for lesions from preimplantation biopsies and MDRD-4 estimated glomerular filtration rate (ml/min/1.73m2) one year after transplant.
| Variables | Biopsy score | p | ||
|---|---|---|---|---|
| 0–3 | 4–5 | 6–8 | ||
| No. of transplants | 18 | 56 | 36 | |
| Glomerular filtration rate, mean (SD) | 49.6 (12.5) | 46.3 (15.7) | 38.5 (14.1) | 0.01a |
| Glomerular filtration rate categorised into functional stages, N (%) | ||||
| <30b | OR | 8 (14) | 7 (19) | |
| 30–59 | 14 (78) | 38 (68) | 28 (78) | |
| ≥60 | 4 (22) | 10 (18) | 1 (3) | 0.04c |
The incidence of patients with poor renal function one year after transplant, eGFR<30ml/min/1.73m2, was 7 (19%) in the 6–8 group, 8 (14%) in the 4–5 group and zero in patients with a score of 0–3. These differences were not statistically significant (p=0.17). In the univariate logistic regression analysis, which analysed the incidence of patients with an eGFR<30ml/min/1.73m2 one year after transplant, the variables that showed a correlation with a p-value<0.20 were dialysis method (haemodialysis vs peritoneal dialysis), delayed graft function, acute rejection, donor HTA, donor diabetes mellitus and final biopsy histological score. Tubular atrophy, interstitial fibrosis, hyaline arteriolopathy and myointimal elastosis assessed individually also had a p<0.20. Delayed graft function was the only variable that had a statistically significant association (p<0.05). In the final multivariate model (Table 7Table 7), the variables that showed a significant correlation were delayed graft function and acute rejection. The score for histological damage for the biopsies, the 6–8 group vs the 0–5 group, had a non-significant adjusted OR of 2.2 (95% CI, 0.7–7.3). In these regression analyses, the biopsy score was categorised into 2 groups, 0–5 and 6–8, owing to the fact that none of the patients in the 0–3 group had an eGFR<30ml/min/1.73m2.
DiscussionWe have presented the results of a follow-up study of 124 transplant recipients of a kidney from older donors in whom a preimplantation kidney biopsy had been performed. The overall results achieved in terms of mortality, graft survival, graft thrombosis, initial graft functioning, acute rejection and glomerular filtration rate were consistent with those reported in the literature in transplants performed with a similar clinical profile.3,16
The main aim of our study was to assess the relationship between the degree of severity of the histological lesions from the kidney biopsies performed and eGFR one year after transplant. The studies that have examined the prognostic value of preimplantation kidney biopsy are heterogeneous in terms of both methodology and results obtained. Glomerulosclerosis of the donor was the most evidenced initial lesion. Impairment ≥20% was associated with poorer graft clinical course.17,18 According to the data from the OPTN/UNOS, with 2096 kidneys biopsied, only the kidneys with glomerulosclerosis <6% had slightly better graft survival after 5 years than all other groups.19 Vascular and tubular-interstitial lesions also were associated with worse clinical course outcomes.20–22 With the aim of improving the prognostic utility, several scales have been proposed to produce an overall score for prior kidney lesions. The most widely used are that of Pirani–Remuzzi23 and the Maryland Aggregate Pathology Index (MAPI).24 Scales based on the Banff criteria have also been used, but at this time there is no specific proposal for this group.25–30 All of them, with their limitations and their methodological differences, show a correlation between the severity of the histological lesions and the functional evolution of grafts, in terms of both glomerular filtration rate and graft survival. However, analysis of the ROC curves from the studies conducted has shown that their discriminatory capacity with respect to graft survival is moderate, with area-under-the-curve values of 0.7–0.8.12,13,31–33 The scale by O’Valle et al.14,15 used in this study was an empirical proposal developed by pathologists from Spain and specifically designed to assess chronic histological damage from donors’ kidney biopsies. The biopsies were processed in paraffin, in a procedure that takes more time and resources than freezing but allows a better assessment of the different kidney compartments.34
Mean eGFR and incidence of patients with an eGFR<30ml/min/1.73m2 one year after transplant were the primary outcomes of our study. These variables have already been used previously in other publications, as they are prognostic factors with a major impact on the survival of kidney grafts in the medium to long term.29–33,35–38 In our results, grafts with a score of 6–8 reached a mean glomerular filtration rate one year after transplant lower than that achieved in the other 2 groups. This was also the group that recorded a greater incidence of grafts with a low eGFR<30ml/min/1.73m2 one year after transplant, although this difference was not statistically significant. The association between the severity of the histological impairment from the preimplantation biopsy and evolutionary eGFR of the graft has already been reported in other publications.29–33 In our analysis, delayed graft function and acute rejection were significantly associated with poor renal function one year after transplant, eGFR<30ml/min/1.73m2. Patients from the 6–8 group had a slightly greater incidence of delayed graft function, which could have influenced this group's worse renal function. Some studies have shown a correlation between preimplantation kidney lesions of the donor, incidence of delayed function and evolution of the glomerular filtration rate of the graft.21,22,27 The incidence of acute rejections was low, and very similar, in the 3 groups analysed.
In interpreting the results obtained, some considerations and limitations should be identified: 1. The histological criteria used in graft acceptance ruled out the use of kidneys with more severe histological impairment; this hindered assessment of their impact on the results. 2. In the analysis of glomerular filtration rate one year after transplant, patients who died or lost the graft in the first year after the transplant were excluded, with the exception of 4 graft losses that were considered to be related to the quality of the kidneys implanted, with non-specific lesions of fibrosis and tubular atrophy in the post-transplant biopsy. These patients were assigned an eGFR of 10ml/min/1.73m2. Graft thromboses were considered to be technical complications not directly related to preimplantation parenchymal lesions. 3. The variability between the diseases that the biopsies analysed was not controlled. 4. Arteries were not observed in 9 biopsies. Hence, these biopsies were not scored in terms of myointimal elastosis. This points to a potential error in classification that may have included some of these transplants in a lower histological group than the one to which they belonged. This fact could have reduced the clinical differences found between the groups with higher and lower histological severity. 5. The number of patients analysed limited the power of the statistical analyses performed.
With the results of the present study, it may be concluded that overall transplant outcomes of older kidney donors, with the acceptance and allocation criteria used, were adequate. Kidneys with greater structural damage in the preimplantation biopsy, a histological score of 6–8, had a worse renal function one year after transplant. This may lead to worse medium and long term graft survival, as has already been reported in previous studies.30–33 Delayed graft function was a significant variable that determine the incidence of grafts with poor renal function one year after transplant. This is a matter that calls for intervention to improve the results obtained. Acute rejection also had an impact on subsequent function of grafts, but the impact in our series was very low.
In our opinion, the use of kidneys with chronic structural damage has negative effects on transplant outcomes, but these negative effects may be acceptable in many cases, especially in older recipients. It is difficult to determine the threshold for histological damage that precludes transplant. In our study, we established a precautionary threshold similar to that used in other histopathological scales.23,28,29 Allowing kidneys with more histological impairment would increase the number of grafts available, but with some presumably worse overall results. Pre-implantation biopsy has its limitations. It requires locally available trained pathologists, its individual functional prognostic value is moderate and it may rule out viable kidneys. However, despite these weaknesses, preimplantation kidney biopsy makes it possible to determine the severity of the donor's kidney lesions. This is information that we consider to be useful, especially in older donors and donors with associated vascular morbidity. It complements the usual clinical–laboratory donor assessment and macroscopic graft assessment, and aids in decision-making regarding acceptance and allocation of kidneys to be transplanted with more criteria. Future initiatives should rigorously validate one of the existing scales or modifications thereof and arrive at a consensus on their use as a guarantor of the quality of our activities.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to thank the transplant coordinators at Hospital Universitario Cruces for their collaboration in obtaining donor data.
Please cite this article as: Amenábar JJ, Camacho JA, Gómez-Larrambe N, Visus T, Pijoan JI, González del Tánago J, et al. Valor pronóstico de la biopsia renal preimplante en donantes fallecidos de edad avanzada en la función renal al año del trasplante. 2016;36:33–41.