El Salvador has the highest renal failure mortality rate in the Americas. Five healthcare providers offer renal replacement therapy (RRT) in the country. The national RRT prevalence has never been reported.
AimsTo determine the RRT prevalence in El Salvador and some basic characteristics.
MethodsThe association of nephrology coordinated a nationwide cross-sectional survey during the third quarter of 2014. 31 renal centres participated in the survey, covering 99.5% of patients.
ResultsNational RRT prevalence: 595 per million population (pmp), N=3807, average age 50.4 years old, 67.5% male. By modality: peritoneal dialysis (PD) 289pmp, haemodialysis (HD) 233pmp, with functioning kidney transplantation 74pmp (living donor only). Social security covers 25% of the population but treats 49.7% of RRT patients. Generally, higher prevalence was observed in municipalities with renal centres or located on the coast or lowlands. Ninety-five per cent of HD patients receive fewer than 3 weekly sessions. Of PD patients, 59% do not belong to a continuous outpatient or automated programme, and 25% still use rigid catheter. Aetiology of chronic kidney disease: unavailable/undetermined 50%, hypertension 21.1%, diabetes 18.9%, glomerulonephritis 6.7%, obstructive causes 1.2%, tubulointerstitial 0.9%, polycystic 0.4% and other 0.7%.
DiscussionDespite the increase in RRT services, the prevalence is lower than the Latin American average (660pmp). Three quarters of HD and PD patients are under-dialysed. Obsolete RRT techniques are still used. The presence of Mesoamerican nephropathy influences the demographic characteristics (many young patients, two-thirds male, high prevalence in lowlands and coastlands).
El Salvador presenta la mortalidad por fallo renal más alta de América. Cinco proveedores de servicios de salud ofrecen tratamiento sustitutivo renal (TSR) en el país. La prevalencia nacional de TSR nunca ha sido reportada.
ObjetivosConocer la prevalencia de TSR en El Salvador y algunas características básicas.
MétodosLa asociación de nefrología coordinó una encuesta nacional transversal durante el tercer trimestre de 2014; 31 centros renales participaron, que cubrían el 99,5% de los pacientes.
ResultadosPrevalencia nacional de TSR: 595 por millón de población (pmp), N=3.807, edad promedio 50,4 años, 67,5% hombres. Por modalidad: diálisis peritoneal (DP) 289 pmp; hemodiálisis (HD) 233 pmp; con trasplante renal funcionante 74 pmp (donante vivo solamente). La seguridad social cubre el 25% de la población, pero atiende al 49,7% de los pacientes en TSR. Generalmente observamos prevalencias más altas en municipios con centros renales, costeros o de zonas bajas. Un 95% de los pacientes en HD reciben menos de 3 sesiones semanales. Un 59% de los pacientes en DP no están en continua ambulatoria o programas automatizados y un 25% todavía utilizan catéter rígido.
Etiología de la enfermedad renal crónica: no reportada/desconocida 50%, hipertensión 21,1%, diabetes 18,9%, glomerulonefritis 6,7%, obstructivas 1,2%, tubulointersticiales 0,9%, poliquísticas 0,4%, otras 0,7%.
DiscusiónA pesar del incremento de servicios de TSR, la prevalencia es inferior al promedio latinoamericano (660 pmp). Un 75% de los pacientes en HD y DP están infradializados. Todavía se utilizan técnicas anticuadas. La presencia de la nefropatía mesoamericana influye las características demográficas (muchos jóvenes, 2/3 hombres, alta prevalencia en zonas bajas y costeras).
El Salvador's territory covers 20,742 square kilometres and it had a population of 6,401,240 residents in 2014.1 It is divided administratively into 14 departments and 262 municipalities and its largest cities are San Salvador (the capital), San Miguel, and Santa Ana. Chronic kidney disease (CKD) is a serious public health problem,2 in part due to the growing population with diabetes mellitus and hypertension, but mainly due to an epidemic of chronic kidney disease of unknown cause called Mesoamerican nephropathy (MeN),3,4 which was first described in the main reference hospital in the country's public health system in 1999.5 According to the latest available figures from the Pan American Health Organization (PAHO), from 2008, El Salvador ranks first for kidney failure deaths (N17–N19) in America, with an age-adjusted rate of 61.6 annual deaths per 100,000 population.6 However, there is little information available about end-stage renal disease (ESRD) patients on renal replacement therapy (RRT) due to the lack of an official registry.
According to a PAHO study, the healthcare system is characterised by being fragmented into 5 service providers (subsystems), inadequately funded, with little coordination and low coverage that emphasises curative measures for kidney disorders. This fragmentation occurs in the absence of integration-related mechanisms between the subsystems, which sometimes results in duplicated and overlapping responsibilities and actions, with important consequences such as concentrating patients in medical facilities from different subsystems in the same geographic zones or the total absence of services in others.7 The theoretical subsystem population coverage is: Ministry of Public Health (MINSAL) 72%, Salvadoran Social Security Institute (ISSS) 25%, Military Health Command (COSAM) 2%, Salvadoran Institute for the Wellbeing of Teachers (ISBM), and private healthcare services 1%.8 Nevertheless, in practice, a large part of the population is deprived of effective coverage.7
Since there is no national registry of ESRD patients on RRT, the Nephrology and Hypertension Association of El Salvador (ANHAES) annually reports the prevalence data from ESRD patients on RRT estimated from nephrology clinic reports to the Latin American Dialysis and Transplantation Registry of the Latin American Society of Nephrology and Hypertension (SLANH). A complete and systematic count has never been done, and therefore the true prevalence is unknown. Given the serious problem of CKD and the need for more precise data, the ANHAES proposed determining the national prevalence of RRT during the third quarter of 2014, as well as learning some of the basic characteristics of these patients.
Materials and methodsANHAES requested the collaboration of all clinical nephrologists from all the subsystems. All agreed to participate. A list was made of the renal care centres providing RRT, counting 31: 14 hospitals, 4 medical units, and 13 clinics. Of these, 18 are in San Salvador, 5 in San Miguel, and 4 in Santa Ana.
In 2014, several RRT services were offered in differing proportions by all the subsystems: MINSAL provides free RRT and cares for the paediatric population in a single public hospital in San Salvador and to the population over 13 years of age in 3 hospitals located in the 3 largest cities. Children are offered haemodialysis (HD), peritoneal dialysis (PD) with a soft catheter, and occasionally, transplantation. The population over 13 years of age is initially treated with intermittent peritoneal dialysis (IPD) with a hard catheter; some patients later switch to IPD with a soft catheter, continuous ambulatory PD (CAPD), or to partial HD (fewer than 8hours per week), but there is no kidney transplant programme for adults. The ISSS cares for contributing members with formal employment and their family members in 2 hospitals and 4 medical units located in the 3 largest cities, initially offering automated or manual hospitalised IPD with a soft catheter, CAPD, or automated PD (a pilot programme). It also offers HD, generally partial, and has a permanent transplant programme for its adult population. COSAM exclusively offers HD, generally partial, in a hospital in the capital where it cares for the military and their family members. The private healthcare services offer HD, generally partial, in 7 hospitals and 13 small clinics in several cities around the country, as well as transplantation in 3 hospitals. Lastly, the ISBM gives coverage to teachers in the public sector and their family members; it does not have its own facilities, but instead contracts HD services, also generally partial, and transplantation services from the other providers. All transplants in the country are from living donors.
A previously designed and validated standardised instrument was used to collect data with the following variables: age, sex, municipality and department of origin, dialysis modality and frequency, type of vascular or peritoneal access, and ESRD aetiology. Cross-sectional data was collected during the third quarter of 2014. All 31 RRT centres participated, which covers 99.5% of the country's estimated patients. All the data were handled in a coded, anonymous format to ensure patient privacy. The data were processed in SPSS 19.0, with in-process quality controls. The data were analysed using the mean and standard deviation for descriptive analyses or interquartile ranges and percentages for qualitative analyses. Prevalence was expressed as a per million population (pmp) rate.
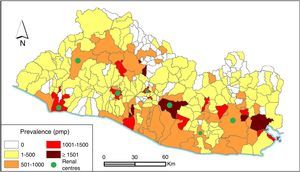
FindingsThree thousand eight hundred seven (3807) patients were counted for a RRT prevalence of 595pmp. Information about the department and municipality of origin was obtained for 84.2% (N=3204) of the patients. The departments with the highest prevalence were San Vicente (774pmp), La Paz (763pmp), and San Miguel (702pmp). The prevalence by municipality for 84% of the patients, as well as the presence of RRT centres, is shown in Fig. 1.
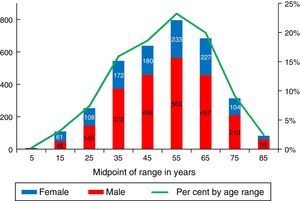
Information about the age and sex was obtained for 91% (N=3452) of the patients. The mean age was 50.4±16 years (Fig. 2) and 67.5% (N=2339) were men; these characteristics were mostly similar in all the subsystems and renal care centres. Sixty-five per cent (65%) of the patients were between the ages of 20 and 59 years, and 32% were over 60. The prevalence in patients under 18 years was 13pmp (N=85; 2.5%).
The proportion of patients per subsystem was: ISSS 49.7%, MINSAL 38.6%, private services 9.3%, COSAMs 1.2%, and ISBM 1.2%. The number of patients per RRT modality in each subsystem is shown in Fig. 3.
The most common RRT modality is PD (289 pmp; N=1848; 48.5%). Of them, 35.7% (N=660) are in CAPD and 48.5% undergo dialysis once per week, 10.6% as needed, and 5.2% 2 or more times per week. In total, 74.6% have a soft catheter and 25.4% use a hard catheter. All the patients with hard catheters belong to MINSAL.
HD is the second most common modality (233pmp; N=1488; 39.1%). Of them, 4.8% undergo dialysis 3 times per week; 68.7% 2 times; 24.5% once, and 2% occasional. In all, 52.2% of the patients have an arteriovenous fistula and 47.8% have catheters, of which 52.8% are temporary catheters and 47.2% are permanent tunnelled catheters.
Patients with functioning kidney transplants (FKT) are the least common modality (73.6pmp; N=471; 12.4%), all from living donors. The ISSS cares for 90.7% of the patients with a FKT and MINSAL for 4.9%, mostly coming from the children's hospital.
The ESRD aetiology was either not reported or was unknown in 50% (N=1903) of the cases. The reported aetiologies were: HTN 21.1%, DM 18.9%, glomerulonephritis 6.7%, obstructive causes 1.2%, tubulointerstitial nephritis 0.9%, polycystic kidney disease 0.4%, congenital and other 0.7%.
DiscussionIn summary, during the third quarter of 2014 there were 3807 patients on RRT in the country, for a prevalence of 595pmp. Sixty-five per cent of the patients were between 20 and 59 years of age, and two thirds were men. Notably, nearly half (44%) of the patients on RRT are men between 20 and 59 years old. PD was the most common modality, although few were in modern programmes and hard catheters are still used in a quarter of them, in MINSAL. Interestingly, we found that social security cared for half of the country's patients on RRT and 91% of the patients with FKT, even though it only covers a quarter of the population.
Based on the ANHAES estimates, this study included at least 99.5% of the patients; therefore, we consider that the true prevalence of RRT in El Salvador has been successfully reported for the first time, and demographic information was also recorded for a good portion of them.
The prevalence of ESRD is increasing globally. In the U.S., the prevalence of patients on RRT is 1901pmp, approximately 70% in HD and 30% with FKT. The main causes of ESRD are diabetes (43.9%) and hypertension (27.8%). The prevalence is the same for both sexes in stage 4 and 5 CKD. It is more common in adults over 70 years of age and the use of healthcare resources is very high.9
According to the SLANH's Latin American Dialysis and Transplantation Registry, the mean Latin American prevalence for patients on RRT for 2010 was 660pmp. The unequal distribution of the availability of services in the region was emphasised, since the RRT prevalences are positively correlated with the gross domestic product of each country. As a result, some countries report figures under 200 pmp while others report figures over 1000pmp. The mean Latin American prevalences per modality are: HD 413pmp, PD 135pmp, and FKT 111pmp. The SLANH estimates that there is unmet demand and, as a result, many patients do not receive RRT, that two thirds of ESRD cases are caused by DM and HTN, and that the remaining third consists of other causes, unknown aetiology, or glomerulonephritis. It also estimates that 40% of the patients are over 60 years old and that fewer than 2% are under 20.10,11
MeN was first identified when it was observed that a high percentage of incident patients on RRT in the main public hospital of El Salvador did not fit the typical epidemiological profile (older patients of both sexes with diabetes and hypertension).5 The cause of this CKD remains under investigation and many subsequent studies confirmed that it mostly presents in young, male patients who work in the hot regions along the coast of the Pacific Ocean, and that it was not exclusive to El Salvador, but that the unusual prevalence of patients with such profile extended throughout the region.3–5,12–20
In 2003, a cross-sectional study was conducted in 8 hospitals in El Salvador recording characteristics of 830 patients on RRT out of the estimated total of 1200. The ESRD aetiology was unknown or indeterminate in 67% of the cases, it was more common in men (71.3%), the most common age range was between 50 and 59 years, and the departments with the highest prevalence were La Paz (253 pmp), San Miguel (181pmp), and San Vicente (180pmp).21 Eleven years after this first characterisation, the patient population on RRT has tripled (N=3807). The aetiology continued to be unknown or not reported in 50% of the cases, the mean age remained around 50 years, most patients were men (67.5%), still doubling the number of female patients, and the departments with the highest prevalence continued to be the same. It is noteworthy that the municipalities with the highest prevalence are generally those with RRT centres, those along the coast, and those located at low altitudes above sea level on the bank of the Lempa River. The few coastal municipalities that showed a low prevalence are generally poor municipalities with mountainous elevations, which could force the patients to migrate to seek treatment. However, we should stress that information was not obtained on the municipality of origin for 16% of the patients, and therefore the rates could be higher than shown.
This epidemiological profile (young, adult males from coastal regions) is similar to the MeN epidemic, as was reported in Guatemala, Costa Rica, and Nicaragua, neighbouring countries also affected by the epidemic.3–5,17–19
Based on the reports from the nephrology clinics, the ANHAES estimates that the annual incidence of ESRD in El Salvador exceeds 400pmp, a heavy burden for a developing country. It is reasonable to assume that, due to the presence of the epidemic, the prevalence of patients on RRT should be much higher. However, despite the notable increase in the number of patients on RRT since 2003, the prevalence for 2014 (595pmp) is 10% lower than the Latin American average, short by 65 patients pmp to reach that figure and surely much more to meet the true need: we have a supply deficit, a large unmet demand.
There is very scarce access to transplantation outside the Social Security, in part because there is no national transplant organisation coordinating all the subsystems and in part because no subsystem procures cadaver donor organs. The organ supply could be expanded considerably if these alternatives were put into place.
It is important to note that for 2014 only 41% of the PD patients received optimal treatment (CAPD, APD, or other modern modality) and that fewer than 5% of HD patients underwent it 3 times per week. Three quarters of the RRT patients on dialysis (HD or PD) did not receive adequate dialysis (N=2509, 75%). If we count RRT prevalence as only those receiving ideal PD or HD and the patients with a FKT, it drops to 203pmp. The other 392 patients pmp are not receiving adequate treatment, which expands yet again the gap of unmet demand.
All of the above undoubtedly contributes to the high mortality attributed to the country2 and must surely also be associated with other comorbidities not assessed in this report, such as anaemia, secondary hyperparathyroidism, infections, cardiovascular complications, etc.
Thanks to the support of the PAHO and SLANH, the healthcare authorities and ANHAES are working jointly to implement a national dialysis and transplantation registry that will enable a better way to learn information about these patients and that will more effectively help to tackle the MeN epidemic. Moreover, attempts are underway to improve the quality and accessibility of the RRT services, as well as initiating a national transplantation programme coordinated between all the healthcare subsystems, including cadaver donor organs in the near future. Lastly, a national plan to promote kidney health and CKD prevention is also on the works. There is no doubt that the nation's best bet is prevention, as well as research into the causes of MeN to fight it at its source and decrease the incidence.
FundingThis study was financed by the ANHAES.
Conflicts of interestThe authors declare that there are no conflicts of interest.
The ANHAES thanks all the nephrologists in El Salvador who participated in this study. We also thank Dr Catharina Wesseling for her valuable comments on a previous version of the manuscript and Alexandre Ribó for his support with the geographic information system.
Please cite this article as: García-Trabanino R, Trujillo Z, Colorado AV, Magaña Mercado S, Henríquez CA, On behalf of the Asociación de Nefrología e Hipertensión Arterial de El Salvador (ANHAES). Prevalencia de pacientes con tratamiento sustitutivo renal en El Salvador en 2014. Nefrologia. 2016;36:631–636.