Introducción: Los estudios sobre adhesión a la restricción de líquidos muestran alta variabilidad en los datos de prevalencia debido a los distintos métodos de medida de la ganancia interdiálisis (GID) y los criterios de punto de corte utilizados. Objetivos: Describir la prevalencia de adhesión a la restricción hídrica según la GID diaria (criterio: ≤ 1 kg) y la GID diaria ajustada al peso seco (PS) (criterio: PS < 70 kg, GID = 1 kg/día; PS > 70 y ≤ 80 kg, GID = 1,1 kg/día; PS > 80 y ≤ 90 kg, GID = 1,2 kg/día; PS > 90 kg, GID = 1,3 kg/día); y estudiar la asociación entre este indicador objetivo y la conducta de adhesión referida por el paciente. Pacientes y métodos: 146 pacientes. Edad media: 66,1 años (desviación típica [DT]: 13,6; rango: 25-88); un 66,4% varones. Estudio longitudinal con un mes de seguimiento. Variables: sociodemográficas. Clínicas. GID diaria. Conducta de adhesión referida, evaluada mediante entrevista por personal entrenado ajeno al servicio, con la pregunta «Para evitar complicaciones entre las hemodiálisis: ¿Durante el último mes, ha tomado usted menos de un litro de líquidos al día? (0 = Ningún día; 10 = Todos los días)». Los pacientes fueron clasificados como cumplidores a partir de valores ≥ 5. Análisis estadístico: descriptivo, pruebas de correlación, χ2 y procedimientos Crosstabs, curva ROC (receiver operating characteristics) y análisis de regresión logística. Resultados: La prevalencia de adhesión «objetiva» a la restricción de líquidos fue 61% (GID diaria media ≤ 1 kg) y 73% (GID diaria media ajustada al peso seco). La prevalencia de adhesión referida (56,2%) se asoció a la GID diaria media ajustada al peso seco (χ2 = 31,34; p = 0,000). En los pacientes con adhesión objetiva ajustada al peso, la prevalencia (PR) de los que se declaran cumplidores es 1,65 veces la de los que se declaran no cumplidores (PR = 1,65; intervalo de confianza [IC] del 95%: 1,29 a 2,11). El modelo final que estima esta asociación incluye edad (mayor), peso seco (menor), potasio (menor), tiempo en hemodiálisis (HD) (menor) y su interacción con la adhesión referida (F = 50,70; p = 0,000; R2 = 44%). La sensibilidad de la conducta de adhesión referida para detectar adhesión objetiva ajustada al peso seco es de un 89%; la especificidad, 58%; el poder de clasificación es del 85% (área bajo la curva de la curva ROC = 0,85; IC 95%: 0,78 a 0,92). La probabilidad de adhesión objetiva ajustada al peso en los pacientes que se declaran cumplidores es 9 veces superior a la de los que refieren ser no cumplidores, para aquellos con tiempo en HD de 2,3 años (PORp25 = 9,16; IC 95%: 2,58 a 32,51); 6 veces para tiempo en HD de 4,7 años (PORP50 = 6,16; IC 95%: 2,12 a 17,92); y 3 veces para tiempo en HD de 8,2 años (PORp75 = 3,44; IC 95%: 1,32 a 8,96). Conclusiones: La prevalencia objetiva de adhesión a la restricción de líquidos fue de 73 y 61% según se considerase o no ajuste al peso seco, respectivamente. La GID absoluta diaria ajustada al peso parece un buen indicador de adhesión en la medida que permite individualizar la pauta de ingesta prescrita. La asociación entre GID ajustada al peso seco y la conducta referida de adhesión permite tener en cuenta la perspectiva de los pacientes, junto con los datos que aportan los indicadores objetivos, lo que puede favorecer el ajuste del punto de corte individual de la GID diaria y suministra información útil para establecer pautas de intervención dirigidas a mantener y aumentar la adhesión.
Introduction: Studies of adherence to fluid restriction show high variability in prevalence data, as different methods of measuring IWG (interdialysis weight gain) and cut-off criteria are used. Objectives: To describe the prevalence of adherence to fluid restriction using daily IWG (criterion: ≤1Kg) and daily IWG adjusted for dry weight (DW) (cut-off point adjusted criterion: DW<70kg, IWG=1kg/day; DW>70kg and ≤80kg, IWG=1.1kg/day; DW>80kg and ≤90kg, IWG=1.2kg/day; DW>90kg, IWG=1.3kg/day) and to study the association between this objective indicator and adherence behaviour as reported by patient. Patients and method: Our study included a total of 146 patients with a mean age of 66 years (SD: 13.6 years; range: 25-88 years), 66% of which were male. Ours was a longitudinal study with one month of follow-up. We collected both sociodemographic and clinical variables and mean daily IWG. Patient-reported adherence behaviour was assessed through an interview by a trained staff member from outside the department who asked the following question: “In order to avoid complications between haemodialysis sessions: during the last month, how many days did you ingest less than 1 litre of fluid per day?” (0= no days; 10= every day). A score ≤5 led to categorisation of patients as compliant with treatment. Statistical analysis included descriptive analysis, correlation test, chi-square and Crosstabs, ROC curve and logistic regression procedures. Results: Prevalence of “objective” adherence to fluid restriction was 61% (mean daily IWG≤1kg) and 73% (mean daily IWG adjusted for dry weight). Reported adherence (prevalence: 56.2%) was associated with IWG adjusted for weight (chi-square =31.34; P=.000). In patients with objective adherence adjusted for weight, the prevalence of reported adherence was 1.65 times that of non-adherence (PR=1.65; 95% CI: 1.29-2.11). The final model for estimating the association between reported adherence behaviour and daily adjusted IWG included: age (higher), dry weight (lower), potassium (lower), time on haemodialysis treatment (less) and its interaction with reported behaviour (F=50.70; P=.000; R2=44%). The sensitivity of reported adherence behaviour for detecting objective adherence adjusted for dry weight was 89%; specificity was 58%, and the overall classification power was 85% (AUC=.85; 95% CI: 0.78-0.92). The probability of objective adherence adjusted for weight in patients who claimed proper adherence was 9 times higher than in non-compliant patients in patients who had been on HD for 2.3 years (PORp25=9.16; 95% CI: 2.58-32.51); 6 times higher in patients on HD for 4.7 years (PORP50=6.16; 95% CI: 2.1217.92); and 3 times higher in those on HD for 8.2 years (PORp75=3.44; 95% CI: 1.32-8.96). Conclusions: Prevalence of adherence to fluid restriction was 73% and 16% depending on daily IWG adjusted/not adjusted for dry weight, respectively. Absolute daily IWG adjusted for weight seems a good indicator of adherence, as it allows for a personalised fluid restriction regimen. Significant association between this objective indicator and reported adherence behaviour supports a combination of patient approach and objective data, which can help with the adjustment of the individual cut-off for daily IWG. This also provides useful information for designing intervention strategies to maintain and increase adherence.
INTRODUCTION
Controlling fluid intake is essential for proper self-care of kidney patients on haemodialysis (HD). However, clinical experience has shown that, compared to attendance to HD sessions or fulfilment of drug prescription, this is the factor with the highest level of non-compliance.1-5
In the medical literature, the appropriate total daily fluid intake of HD patients with anuria varies from restrictive indications (0.5-0.9 litres/day6,7) to much more permissive recommendations.2 In our environment, the standard consensus prescription is a maximum intake of 1 litre/day in anuric patients. This indication takes into account the basic needs of the body and the water content of normal dietary foods.8 Recent studies have supported this prescription, because over-hydration may be defined as extracellular water >15%, which is associated with hypertension and decreased survival.9 In addition, through bioelectrical impedance analyses, it has been shown that normal hydration in renal patients is established at approximately 2 litres between sessions, this being the optimal gain for reducing intradialysis adverse events by 75%, and the risk of mortality by 50%.9-11
There is a general widespread agreement that weight gain between haemodialysis sessions (interdialytic weight gain, or IWG) is directly correlated with fluid intake, and as such, is a good indicator for adherence to fluid restrictions.3 There is a high variability in the results regarding adherence to prescription, since various methods have been used to measure IWG and different criteria and cut-off points are employed to establish adherence.
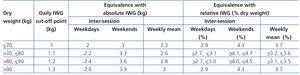
One method for establishing adherence is to determine IWG in relative terms, calculating the percentage increase in inter-HD weight adjusted for the dry weight of each patient, whether calculated between two sessions or as a mean over a longer period of time. These measurements are based on the fact that the tolerable quantity for total fluid intake that avoids short- and mid-term complications varies based on dry weight: the higher the weight, the higher the weight gain percentage allowed between sessions. Furthermore, studies have shown that the higher the IWG, the better the nutritional status (using protein catabolic rate as an indicator).1,12-16 Among other findings, these studies reported that when IWG is less than 3% of total dry weight, there is a risk of malnutrition,15 although when weight gain is >5.7%, the risk of mortality increases by 35%.1 Although it has not been clearly established, the results do support personalisation of fluid intake prescriptions and the adoption of permissive criteria for weight gain.1,12,17 In this sense, the primary advantage of relative estimates is that they allow for personalising the prescriptions for each patient and allow for greater fluid intake in patients with greater total body weight. With an upper limit of 5.7%, the results for adherence show prevalence rates between 82% and 97%,1,12 (92.5% in Spain12).
IWG can also be calculated as an absolute value, whether between two sessions or over the course of several sessions, estimating mean IWG. In this vein, several authors have established the adherence criterion that mean IWG should not surpass 2.5kg.9,18-20 The prevalence of adherence when analysed under this criterion is 58%.18 Another method is to estimate absolute daily weight gain between two sessions (daily IWG) and then the mean weight gain during a period of time; in this case, normal values are established at ≤0.9kg/day,21,22 or ≤1kg/day.8,23,24 Under this criterion, prevalence values range between 51%23 and 57.8%.25 This method also allows for establishing adherence criteria that comply with the 1 litre prescription given to patients. However, even for patients that are highly motivated to adhere to fluid prescriptions, it is difficult to accurately quantify 1 litre of total fluid intake per day.3 In addition, adherence can vary widely; for example, it has been shown that adherence is higher during weekends.26 As such, estimating IWG as a mean of absolute daily gains for a long period of time is more appropriate, since this provides a more precise indicator for adherence, as compared to values taken from only 2 or 3 days between sessions.25 In addition, in order to avoid an excessively restricted water intake in heavy patients, we could make adjustments both in the prescription for fluid intake and the cut-off points used, according to patient weight. This would have to take into account the 3% and 5.7%1,15 limits for dry weight relative percentages as a weekly mean increase, and an absolute mean difference between sessions of 2-3 litres.10,11 In this sense, we cannot find recommendations for adjusting prescriptions based on absolute values, except for the proposal that when dry weight is <50kg, the adherence criterion should be 0.7kg.24
With this in mind, our first objective was to determine the prevalence of adherence to fluid restrictions based on daily IWG, using a daily IWG less than or equal to 1kg as the criterion for adherence. Secondly, considering the limits described above, we tried to develop a personalised system for the cut-off point of IWG in terms of dry weight, and to analyse the prevalence of adherence using the value of daily IWG adjusted for dry weight.
In addition to these objectives, it is important to take into consideration adherence as perceived by the patients.19 It has been shown that the perception a patient holds regarding his/her disease (the perceived control over the disease, the anticipated consequences, the mental toll of the treatment and measures prescribed, concern about consequences, etc.) significantly influences the actions they will take, including adherence to prescribed behaviours.27-29 Several studies have examined adherence as reported by patients and reported a significant correlation with objective indicators.30-34 However, correlation is not equivalent to concordance between the two forms of measurement. We have not found a single study that demonstrated whether what the patient reported coincided with the results from the objective form of assessment.
As such, our third objective was to examine the relationship between these two forms of measurement, establishing the capacity of the subjective adherence report to correctly classify patients as determined using the objective indicator of adherence. Using the patient approach, together with the information provided by objective indicators, may favour the individual adjustment of daily IWG cut-off points. This may also provide useful information for establishing interventions designed to increase adherence.
PATIENTS AND METHOD
Ours was a longitudinal study with a one-month follow-up period during which we monitored the weight of patients between HD sessions. We contacted a total of 170 patients with anuria that were undergoing treatment in the HD units at two different centres. The inclusion criteria were:
- No comprehension difficulties. Five patients were excluded for not complying with this requisite.
- No intercurrent disease during the previous month. Three patients were excluded.
- Since there were patients that for various reasons could partially recover residual diuresis, we excluded patients with mean gains of 500ml/24 hours or less. A total of 11 patients were excluded based on this criterion.
A total of 151 patients that complied with all inclusion criteria were invited to voluntarily participate in the study, they were explained the objectives of the research, the confidentiality of results, and guaranteed anonymity. Five patients chose not to participate.
The final study sample was composed of 146 patients treated at the Clínica Vistahermosa (39.0%) and the Hospital Perpetuo Socorro (61.0%) in Alicante. Mean patient age was 66.1 years (standard deviation [SD]: 13.6 years; range: 25-88 years) and 66.4% were male. We observed no differences in age based on sex.
We took the following variables into account for our study:
Sociodemographic variables: age and sex
Clinical variables:
- Time on HD: time elapsed between the patient’s entry into an HD programme and the start date of the study.
- Dry weight: patient’s weight in the absence of any immediate complications from the HD session (mainly cramping, oedema, and dyspnoea). Although this measurement is quite stable, it is usually adjusted for these complications in clinical practice. The parameter used is the mean dry weight over the period of one month.
- Nutritional status: for this parameter, we used a combination of body mass index and serum albumin.
- Serum potassium: due to its association with adherence to dietary and fluid intake restrictions.
- Kt/V was registered as an indicator for proper dialysis treatment.
- Daily interdialytic weight gain (daily IWG): the mean value for daily weight loss, which in this study was estimated over a one month period.
In order to determine the prevalence of adherence, we first applied the criterion of daily IWG equal to or less than 1kg, obtaining a binary variable that categorised patients as adherence (yes/no), based on exceeding this cut-off value or not. We performed a second grouping by adjusting this criterion for dry weight, and the classification of adherence (yes/no) was based on a different daily IWG cut-off point for each patient’s dry weight value. This system, based on clinical experience, weight gain limits, and hydration status,1,10,11,15 is displayed in Table 1.
- Relative weight gain (relative IWG): we calculated the percentage increase of mean dry weight based on relative gains between sessions over the 1-month period. In order to determine prevalence, and following more permissive criteria,1,2,14 we applied the cut-off point of relative IWG at ≤5.7%.
- Reported adherence behaviour: adherence as reported by the patient was evaluated through a personal interview. We reminded the patient of the fluid intake restriction (1 litre maximum, including liquid and solid intake) and asked him/her to score compliance using an 11-point scale in item “In order to avoid complications between haemodialysis sessions: during the last month, how many days did you ingest less than 1 litre of fluid per day? (0 = no days; 10 = every day).”
Patients were classified as compliant if they obtained a score of 5 or higher, which also was converted into a binary yes/no value for reported adherence.
Reported adherence behaviour and other sociodemographic variables were collected through interviews performed by trained personnel from outside of the department. All other variables were collected using clinical histories.
STATISTICAL PROCEDURE
We used SPSS statistical software version 19.0 for all statistical analyses. We applied the descriptive statistics package as well as a frequencies package. Comparative analyses were performed using Student’s t-tests. We also obtained Spearman’s or Pearson’s correlation coefficients for quantitative variables. Qualitative variables were assessed using chi-square tests.
In order to analyse the association between the objective indicator (daily IWG) and reported adherence behaviour, we used the corresponding binary variables. First, we used the Crosstabs procedure to obtain a significance value for the correlation between chi-square tests and likelihood ratios and the estimated prevalence ratio (PR) and prevalence odds ratio (POR) values. Secondly, we performed two logistic regression analyses, considering the dependent variable to be the two aforementioned classifications of daily IWG, and the independent binary variable was the reported adherence (yes/no). We obtained adjusted goodness of fit indices (R2) using Nagelkerke’s method. We applied a 95% confidence interval. The results for sensitivity and specificity were obtained using ROC curves. In order to perform a more precise evaluation of the association, we also performed a third regression analysis for examining possible confounding and modifying factors using a backwards stepwise regression model, using the likelihood ratio test and applying the ConfounReg command.35
RESULTS
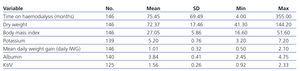
Table 2 summarises the clinical variables assessed. We only observed significant differences between male and female patients for Kt/V values (t=-2.253; P=.027) and dry weight (t=2.193; P=.031). Mean time on haemodialysis was 75.4 months (SD: 69.5 months; 25th percentile: 2.3 years; 50th percentile: 4.7 years; 75th percentile: 8.2 years).
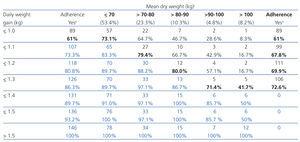
Mean daily IWG in the overall sample was 1.01kg (SD: 0.32kg). Applying the first classification criteria of a mean daily IWG≤1kg, the prevalence of adherence was 61%, while for the second criteria of an IWG cut-off point adjusted for dry weight adherence was 72.6% (Table 3). This adjusted criterion was equivalent to a relative IWG of 3.1%-3.7% (Table 1). There were no differences observed according to gender. The group classified as adherent to adjusted IWG restrictions was older (t=4.888; P=.000), had lower dry weight (t=-2.151; P=.008), lower potassium levels (t=-2.815; P=.006), and had been on HD for a shorter period (t=2.016; P=.046).
In terms of reported adherence behaviour, the mean patient score was 5.25 (ST: 4.14; 8-10: 45.2%; 0-2: 37.9%). The two measures of adherence, the “objective” indicator and the subjective value of patient-reported behaviour, were significantly correlated (r=-0.45; P=.000). Applying the cut-off value of ≥5, the prevalence of reported adherence to treatment was 56.2%. The prevalence of adherence in female patients (67.3%) was higher than that reported by male patients (50.5%) (chi square =3.746; P=.05).
The binary logistic regression analysis, which evaluated reported adherence as the only predictor of objective adherence, improved the data uncertainty explained percentage (R2=20.4%) and the overall classification power (area under the curve [AUC]=71%) when applying weight-adjusted IWG (Table 4). The contingency analysis of binary variables that classified patients according to the two measures of adherence revealed that 87.8% of patients who reported adherence also complied with the objective measure of weight-adjusted adherence, while only 53.1% of those who reported non-adherence fulfilled the objective variable requirement. Among patients that were declared adherent by the objective analysis, patients with self-reported adherence were 1.65 times more than patients who declared they were non-adherent (PR=1.65; 95% CI: 1.30-2.11) (Table 4).
The third logistic regression analysis explored the role of possible confounding and modifying factors in the association between weight-adjusted IWG and reported behaviour. The final model that predicted “objective” patient adherence based on reported adherence included reported adherence, age, dry weight, potassium levels, time on HD, and interaction with reported adherence (chi square =50.70; degrees of freedom [df]=6; P=.000; R2=44%; n=139). The results show that, with a 95% confidence level, patients that classify themselves as compliant with the fluid restriction are 9 times more likely to be objectively classified as adherent than self-declared non-compliant patients when time on HD is 2.3 years (PORp25=9.16; 95% CI: 2.58-32.51), this is 6 times more likely in patients on HD for 4.7 years (PORp50=6.16; 95% CI: 2.12-17.92), and 3 times more likely in patients on HD for 8.2 years (PORp74=3.44; 95% CI: 1.32-8.96).
This model improves the sensitivity of reported adherence behaviour for detecting objective weight-adjusted adherence, which is 89%, and the rate of correct classification: 80%. The specificity is 58%. The overall classification power of the model with the ROC curve is 85% (AUC=0.85; 95% CI: 0.78-0.92).
DISCUSSION
One of the primary objectives of this study was to establish the prevalence of adherence to fluid restrictions in chronic kidney patients on HD. The importance of adjusting recommendations for fluid restrictions is clearly established. However, clinical and empirical experience has demonstrated variability in these prescriptions, the indicators and criteria for adherence used, and therefore, in the currently available results regarding the prevalence of adherence.
In this study, we selected absolute daily IWG as the indicator for adherence, which is the most precise measure and most closely related to the prescribed restrictions. As the first cut-off criterion, adherence was established at IWG≤1kg/day, based on daily clinical experience, guideline recommendations,8 and studies that have shown the importance of this value in reducing blood pressure, intradialytic complications, and mortality.10,11,22,24,25 According to definition, the prevalence of adherence was 61%. These results are similar to those from other studies involving calculations of absolute IWG.14,18,25
The most commonly used measure in these situations is relative IWG, which allows for a wider range of normal values (2.9%-5.7%) based on different tolerance levels for each patient.2,12,17 In the case of relative estimates with a 5.7% limit for interdialytic relative dry weight gain, the prevalence of adherence ranges between 83% and 97%,2,12 and 98% in our study. This would mean that virtually all our patients complied with prescribed fluid restrictions, and this is evidently not the case, based on clinical experience.
The primary advantage of relative estimates is the flexibility they provide for prescribing restrictions and establishing criteria for adherence based on dry weight. Applying this to absolute measurements, we studied the prevalence of adherence based on daily IWG, but adding an adjustment for patient weight. In addition, the positive correlation between IWG and dry weight also indicates the need for performing this adjustment to the cut-off value. Our data revealed a prevalence of adherence of approximately 73%. This is a realistic method for following the recommendations from other authors that propose a personalised prescription for fluid intake, as well as for determining which patients comply with adherence or not based on patient dry weight.
The second objective of this study was to evaluate the perception of each patient regarding adherence to fluid restrictions, and to analyse the association of this perception with an objective indicator. Firstly, the results demonstrate that more than half believe that they do comply with fluid restrictions to some degree, and more than one third reported to be fulfilling a high level of compliance. In other studies using scales based on the responses to 431,33 or 724 questions, adherence to treatment as reported by patients ranges between 26% and 63%. This self-evaluation method was significantly correlated with the objective indicator in our study, as in others studies24,31,33; however, these results do not imply a high level of concordance between these two types of assessment.
The predictive value of subjective behaviour assessments improves when we perform a statistical adjustment in the logistic regression analysis. The sensitivity of this measure also improves when dealing with weight-adjusted IWG. Thus, by applying the ROC curve analysis and controlling confounding and modifying variables, we obtained an AUC of 85%, which implies that perceived adherence has a good predictive value for the objective indicator. These results support the use of perceived adherence as another indicator to take into account when adjusting fluid restrictions and evaluating results. The levels of sensitivity (89%) and specificity (58%) also show that reported behaviour is a better tool for detecting true positives than true negatives. It could also be expected that patients may want to project a social image of compliance, such that when the report is of adherence to the prescription, the objective indicator in many cases may show the opposite. We observed results to the contrary: when a patient reported compliance, there was a very high probability that his/her daily IWG did not exceed the cut-off point established based on dry weight. In addition, we observed that many patients reported non-compliance when the objective indicator showed the opposite. The prevalence of perceived behaviour was always lower than the objective results for all patients grouped by dry weight. It is possible that the fact that the interviews were performed by personnel from outside of the department may have eliminated the bias potentially created by patients responding as they think health professionals would want them to.
Despite the positive results, concordance between these two measures was not 100%. Several factors could explain the discrepancy between perceived behaviour and objective measures of adherence. We must remember that although a prescribed behaviour is followed, the expected result is not always obtained. Such may be the case for interdialytic session weight gain, which is an objective indicator, but one that is not equivalent to adherence to fluid restrictions. Absolute daily IWG is the result of patient behaviour, but is only one of the possible consequences that could arise from following the prescribed recommendations. Obviously, patients that do comply with fluid intake restrictions based on the prescribed recommendations should have a daily IWG close to the cut-off point that corresponds to their dry weight. However, there are many reasons for which, despite compliance with prescriptions, these actions may not always result in a daily IWG of 1.0-1.3kg. Biological factors such as sweating, ambient temperature, and diet can all produce discrepancies. In addition, there may be errors due to the perception of thirst, difficulties in quantifying fluid contents of foods and accurately measuring daily fluid intake, among others.36 We can also refine the adjustments based on other longitudinal studies that evaluate the results in terms of short, mid, and long-term morbidity.
As regards the possible factors associated with adherence, we observed that older patients had lower weight gains and higher perceived compliance values. Several studies have also observed that age is a predictive factor37 or is related to the indicator for fluid intake,38 although others39 failed to show such correlations. In any case, the analysis of correlations between subjective behaviour and the objective indicator shows this to be a confounding factor to be controlled.
In our study, the total time spent on HD treatment was not linearly correlated with the objective indicator. It is possible that chronic adherence to fluid restriction prescriptions does not change drastically over time, once an initial period of adaptation has elapsed. It has been shown, for example, that patients demonstrate a greater level of adherence at the start of treatment,7,38 specifically during the first 6 months, with decreases in the following 3 years.3 However, other studies have shown that patients with good short-term compliance also have good long-term compliance.31,40 Currently, no longitudinal studies have been performed that clarify how adherence to prescribed treatment varies through time with control on other related factors, such as maintenance of residual diuresis and consequent fluid elimination during initial periods.3 However, we observed that the perception of adherence is greater with less time on HD. This factor also modulates the relationship between reported behaviour and the objective indicator adjusted for dry weight. In this manner, the association between perceived compliance and adherence is much greater in patients on HD for less than 2 years, decreases in patients on HD for approximately 4.5 years, and is clearly lower in patients on HD for >8 years. This result does not show that, as time passes patients are less compliant with prescribed fluid restrictions, but rather that the concordance between perceived compliance and “objective” adherence to restrictions is lower. It may be that the conscious control of dietary restrictions, fluid intake, etc. gives way to an automatic control resulting from habituation and an incorporation of changes into daily routines. This result demonstrates the importance of reinforcing patient perception of compliance and reviewing perceived non-adherence that may be misguided. Secondly, it is not precisely the exact measurement of a litre, which can be prescribed but is difficult to apply and measure in real life, but rather the adjustments made by the patient during the first period of time on HD based on his/her perception of compliance with fluid restrictions that take precedent. Finally, health professionals play a particularly important role in the first years following the start of HD by adjusting a personalised IWG based on weight and the perception of compliance held by the patient.
The results of this study allow us to conclude that absolute daily IWG adjusted for patient dry weight is a good indicator for adherence to fluid restrictions, since it facilitates a more precise estimate, a personalised fluid restriction prescription based on weight, and better adjustment to the nutritional needs of each patient. Adherence as reported by patients also has a high capacity for classifying patients according to the subjective indicator, and is much greater during the first two years on HD. This is all very relevant information for health professionals, since the first few years in which a patient starts an HD programme require an adjustment of an objective indicator (personalised IWG based on weight) and a subjective indicator (the patient perception of adherence).
Acknowledgements
We would like to thank Antonio Llopis, Lola Arena, and the staff of the Clínica Vistahermosa and Hospital Perpetuo Socorro Hospital in Alicante, for their collaboration in data collection.
We would also like to thank Irene Portilla, Paola Reyes, and Patricia Sánchez for their efficient collection of data from interviews with patients at both hospitals.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Proposed cut-off points for daily interdialytic weight gain adjusted for dry weight as a criterion for adherence
Table 2. Clinical variables
Table 3. Prevalence of adherence according to daily interdialytic weight gainª
Table 4. Contingency analysis and binary logistic regression. Reported behaviour and objective indicator of adherence