Introducción: El sobrepeso y la obesidad se asocian a un mayor riesgo cardiovascular y mayor mortalidad en la población general, y existen datos controvertidos en la población en diálisis. Las adipoquinas (leptina, adiponectina) producidas en los adipocitos podrían jugar un papel en dicho proceso, así como los parámetros inflamatorios (proteína C reactiva [PCR], interleuquina 6 [IL-6]) pueden ser marcadores del mismo. Por otro lado, alcanzar el peso seco es hoy uno de los principales objetivos de adecuación en diálisis porque la sobrehidratación sí es un claro predictor de mortalidad. El objetivo de este trabajo es analizar la composición corporal mediante la técnica de bioimpedancia espectroscópica en pacientes en hemodiálisis (HD), evaluar la prevalencia de sobrepeso y sobrehidratación y su posible relación con adipoquinas, parámetros inflamatorios y nutricionales, técnica de HD (convencional [HDC], hemodiafiltración on line [HDF-OL]) y necesidades de eritropoyetina. Métodos: En un estudio observacional transversal, se ha realizado una bioimpedancia espectroscópica pre-HD en mitad de la semana a 77 pacientes en HD extrahospitalaria: 56 HDC y 21 HDF-OL. Se considera sobrepeso cuando el índice de masa corporal (IMC) es ≥ 25 kg/m² y sobrehidratación cuando ésta normalizada al agua extracelular es superior a 0,15. Se han analizado los parámetros clínicos y bioquímicos y se ha determinado IL-6, leptina y adiponectina. Se han comparado estos datos entre los pacientes con y sin sobrepeso, normo y sobrehidratados y con ambas técnicas de HD. Resultados: El 50% de los pacientes cumplen criterios de sobrepeso y el 21% están sobrehidratados pre-HD. Los pacientes con sobrepeso tienen una proporción de grasa y agua extracelular superior (p < 0,001). Los niveles de leptina (p = 0,001) y de PCR (p = 0,036) son más elevados, y los de adiponectina, más reducidos (p = 0,003). Existe correlación inversa entre el IMC y la masa magra (p = 0,01). Los marcadores nutricionales (prealbúmina, albúmina, proteínas totales, creatinina y transferrina) guardan relación con la masa magra (p = 0,05). Al comparar las dos técnicas de HD, se observa menor proporción de grasa en la HDF-OL (p = 0,049) sin diferencias en el grado de sobrehidratación. En el análisis univariante, la edad, la grasa, el cociente agua extracelular/intracelular, la leptina, la hipoadectinemia, la menor masa muscular y la técnica de HDC fueron predictores de sobrepeso. En el análisis multivariante, la hipoadectinemia (odds ratio [OR]: 0,86; intervalo de confianza [IC]: 0,76-0,98), la masa muscular (OR: 0,89; IC: 0,84-0,94) y la técnica de HDF-OL (OR: 0,20; IC: 0,04-0,99) predicen la ausencia de sobrepeso. Conclusión: Este estudio observacional subraya la alta prevalencia de sobrepeso en la población en HD extrahospitalaria y el hecho de que éste está en relación con la grasa y el agua extracelular. Además, se acompaña de mayor inflamación y de niveles superiores de leptina e inferiores de adiponectina. La utilización de la técnica de HDF-OL se asocia a menor sobrepeso por menor proporción de grasa. La bioimpedancia puede ser un arma más en el proceso de toma de decisiones ante los cambios de peso de los pacientes en diálisis.
Introduction: Overweight and obesity are associated to a higher cardiovascular risk and mortality in the general population and conflicting findings exist in the dialysis population. Adipokines (Leptin, adiponectin) produced in adipocytes may play a role in that process, and inflammatory parameters (CRP, IL-6) may be markers for it. Nevertheless, obtaining dry weight is today one of the main aims of adequacy in dialysis because overhydration is a clear mortality predictor. Objectives: The aim of this study was to analyse body composition using an impedance spectroscopy technique in patients on haemodialysis (HD): and evaluate overweight and overhydration prevalence and its possible relation with adipokines, inflammatory and nutritional parameters, HD technique (Conventional [CHD], on-line haemodiafiltration [OL-HFD]) and erythropoietin needs. Methods: In a cross-sectional observational study, a pre-HD multifrequency bioimpedance spectroscopy (BIS) was performed in the middle of the week on 77 HD outpatients: 56 CHD and 21 OL-HFD. Patients were considered overweight when Body Mass Index (BMI) was ≥25kg/m² and overhydrated when overhydration normalised for extracellular water was higher than 0.15l. Clinical and biochemical parameters were analysed and IL-6, leptin and adiponectin levels were determined. This information was analysed in overweight and non-overweight, regular and overhydrated patients and both HD techniques. Results: 50% of patients fulfilled overweight criteria and 21% were pre-HD overhydrated. Overweight patients had a superior fat and extracellular water content (P<.001). Leptin (P=.001) and CRP (P=.036) levels were higher and adiponectin levels were lower (P=.003). An inverse correlation did exist between BMI and lean mass (P=.01). Nutritional markers (prealbumin, albumin, total proteins, creatinine and transferrin) were related to lean mass (P=.05). Comparing both HD techniques, a lower fat content was observed in OL-HFD (P=.049) without overhydration differences. In the univariate analysis, age, fat, extracellular/intracellular water ratio, leptin, hipoadiponectinaemia, lower lean mass and CHD technique were predictors of overweight. In the multivariate analysis, hipoadiponectinaemia (OR: 0.86; IC: 0.76-0.98), lean mass (OR: 0.89; IC: 0.84-0.94) and OL-HFD technique (OR: 0.200; IC: 0.04-0.99) predicted the absence of overweight. Conclusion: This observational study emphasises the high prevalence of overweight in the outpatient haemodialysis population, as long as overweight is related with fat and extracellular water. Furthermore, it is accompanied by higher inflammation and leptin levels and lower levels of adiponectin. The use of the OL-HFD technique is associated to less overweight and fat content. Bioimpedance may prove to be a valuable ally for decisions regarding weight changes in dialysis patients.
INTRODUCTION
Chronic renal failure (CRF) is a health problem which is often accompanied by high mortality of cardiovascular origin1 but this relation has not been clearly established. Among the possible factors which should be taken into consideration are hypertension (HTN) and overweight-obesity.
The abnormal state of overhydration in dialysis patients has been related to HTN, left-ventricular hypertrophy and other adverse cardiovascular effects,2 and poses a proven risk of mortality. Thus, improving dry weight is currently one of the main objectives of adequate dialysis.3
In the general population, overweight and obesity are increasingly prevalent conditions and they are associated with higher cardiovascular risk and increased mortality.4 However, in some (but not all) studies into the survival of patients on haemodialysis (HD) the phenomenon of “paradoxical obesity” or reverse epidemiology occurs, where a higher body mass index (BMI) is accompanied by better survival rates.5 In this complex population some findings have suggested that the relation between adiposity and cardiovascular risk factors does not follow the same pattern as in the normal population. In fact, stage 5 CRF non-overweight patients frequently have dyslipaemia and inflammation.6
Adipose tissue is a complex organ, with pleiotropic functions beyond the mere storage of energy. It is related with the secretion of a number of proteins (adipokines), including leptin and adiponectin and also cytokines such as interleukin-6 (IL-6). Today, we know that adipose tissue plays an important role in the production of these molecules in the catabolic uraemic medium through its influence on systemic inflammation and uraemic anorexia.7 Leptin regulates the appetite and the energy catabolism. Its serum concentration is a good indicator of fat mass (FM) both in obese patients8-11 and non-obese patients with CRF.12 It is considered an average molecular weight (16 000 Daltons) uraemic toxin and its elimination is greater with high flux membranes and with haemodiafiltration techniques (HDF).10,11 Adiponectin is a hormone secreted almost exclusively by adipocytes which has, in contrast, anti-atherogenic and anti-inflammatory properties. Adiponectin levels are reduced in obese subjects.12
Among the inflammation markers, C-reactive protein (CRP) is, furthermore, a cardiovascular risk marker in the general population13 and in dialysis patients,14 as is the plasmatic level of some cytokines such as IL-6.15
The bioimpedance spectroscopy (BIS) analysis is a non-invasive method, useful both for measuring body fluid and for evaluating FM and lean mass, which is really the expression of muscle mass. It has been validated recently in the population in HD3 especially in order to determine the dry weight.
This study analyses the body composition of HD patients through BIS, evaluating the prevalence of overweight and overhydration in an HD outpatient population and its possible relation to HD technique (conventional [CHD] and on line liquid replacement [OL-HDF] haemodiafiltration), adipokines (leptin, adiponectin), inflammatory (CRP, IL-6) and nutritional parameters (prealbumin, albumin, total proteins, cholesterol, transferrin) or needs of erythropoiesis-stimulating factors to maintain adequate haemoglobin (Hb) levels.
PATIENTS AND METHODS
This study includes a cross-sectional sample of 77 clinically stable patients on HD (n=77) from an outpatient unit of a health centre forming part of the Hospital Severo Ochoa. In the sample, 56 patients underwent conventional dialysis (CHD) with a medium flux polysulfone membrane (n=56), while 21 patients underwent the OL-HDF with a high flux polysulfone membrane and with minimum liquid replacement of 18 litres (n=21). The study was approved by the hospital’s ethics committee. All the patients were invited to take part; they all accepted and were included in the study after signing the consent form. The minimum length of the dialysis session with either technique was 4 hours, with a frequency of three times per week. We used ultra pure water and its quality was assessed monthly by colorimetric kinetics (European Pharmacopoeia VI edit. Methods).
The aetiology of the CRF was: chronic glomerulonephritis (18%), interstitial nephropathy (14%), polycystic disease (6%), nephroangiosclerosis (19%), diabetic nephropathy (19%), idiopathic (11%) and other causes (12%). Comorbidity was assessed in each patient using Charlson's16 comorbidity index. Some 21% of patients were diabetic and 24% had a history of cardiovascular disease.
Biochemical parameters
Blood samples were taken on an empty stomach, before the second weekly dialysis session, after 20 minutes in a semi-seated position. The vacutainers were kept cold and placed immediately on ice, then they were centrifuged at -4ºC and the serum was stored at -40ºC until the analysis. The measurements of serum creatinine, cholesterol, total proteins, albumin, transferrin, prealbumin and CRP were analysed using methods approved by the Biochemistry Department of the Hospital Severo Ochoa. The parathormone was measured by chemiluminescence (reference values: 16-87pg/ml).
Leptin levels were determined in lithium-heparin plasma using the Human Leptin ELISA kit (Mediagnost; sensitivity of 0.01ng/ml, specificity and interanalysis accuracy of 7.5% and intra-analysis accuracy of 4.35%. Reference values: Females, 50th percentile for BMI=24: 10ng/ml; males, 50th percentile for BMI=24: 2.55ng/ml).
Adiponectin was determined in lithium-heparin plasma using the Adiponectin ELISA kit (Mediagnost; sensitivity of 0.6ng/ml, specificity and interanalysis accuracy of 6.7% and intra-analysis accuracy of 4.7%. Reference values: Females: 4-19.4μg/ml; males: 2-13.9μg/ml).
The IL-6 was determined in lithium-heparin plasma using the Human IL-6 immunoassay (R&D Systems; sensitivity of 0.7ng/ml, specificity and interanalysis accuracy of 6.4% and intra-analysis accuracy of 4.2%. Reference values: 3.12-12.5ng/ml).
Inflammation was defined as levels of IL-6 or CRP above the mean value (>12.5ng/ml and >5.05ng/ml, respectively).
The erythropoietin resistance index was defined as the weekly dose of erythropoietin (U/kg pre-dialysis/dose) divided by the level of Hb in g/dl.
The patient’s dry weight was determined following clinical criteria and was adjusted immediately after each dialysis session.
The patient was considered to be overweight when BMI was higher or equal to 25kg/m².
Measurement of bioimpedance
This was performed immediately before the second dialysis session of the week. All patients were measured and weighed. The BMI was calculated. A multifrequency unit was used (Body Composition Monitor, BCM, Fresenius Medical Care). Extracellular water was determined in litres (ECW), intracellular water (ICW), total body water (TBW), total lean tissue mass in kg (LTM) and relative lean tissue mass as a percentage (rLTM %), fat mass in kg (FAT) and relative fat mass as a percentage (FAT %), ECW/ICW and ECW/TBW ratios, body cellular mass in kg (BCM), phase angle (Phi50), overhydration (OH) in liters.
The BCM calculates OH as the difference between the predicted ECW and the true ECW. This method is based on the hypothesis of the constant properties in tissue hydration, assuming that OH in dialysis patients is primarily expressed in an expanded extracellular space. OH is defined in the range of normality from the 10th to the 90th percentile of the healthy population, varying from –1l to +1l.17 Patients with OH values over the 90th percentile (+1.1l) are considered overhydrated, while those with values below the 10th percentile (–1.1l) are considered depleted. The state of OH is normalised for ECW (OH/ECW), thereby dividing the patients into a normally hydrated group or an overhydrated group. OH was defined as an OH/ECW ratio over 0.15.3
Statistical analysis
All statistical analyses were conducted using the version 12 SPSS program (SPSS Inc. Chicago). The normally distributed variables were expressed as mean ± standard deviation, and the variables that did not follow a normal distribution as median and range (minimum and maximum). Categorical variables were also expressed as a number and percentage. Comparisons between groups were performed using the Student’s t-test, the Mann-Witney or chi-square test, depending on the type of variable. The Pearson or Spearman correlations were used for the univariate analysis, depending on the nature of the variable. A simple and multiple logistic regression analysis was used to assess the influence of several variables on the presence of a BMI≥25kg/m². In the multivariate analysis all variables presenting a statistically significant correlation with the BMI were included and the step forward method was used to select the variables, the likelihood ratio being the criterion for the inclusion of a variable in the model. A probability value below 0.05 was used as significance criterion.
RESULTS
General characteristics, levels of adipokines, nutritional and inflammatory parameters and analysis of body composition of our population on haemodialysis
This study included 77 patients coming from a single outpatient HD unit: 56 were treated with CHD and 21 with OL-HDF.
Thirty-nine patients (50%) fulfilled overweight criteria (BMI≥25kg/m²). Their weight was 77±11kg, and that of the non-overweight patients was 57±7.66kg (P=.001).
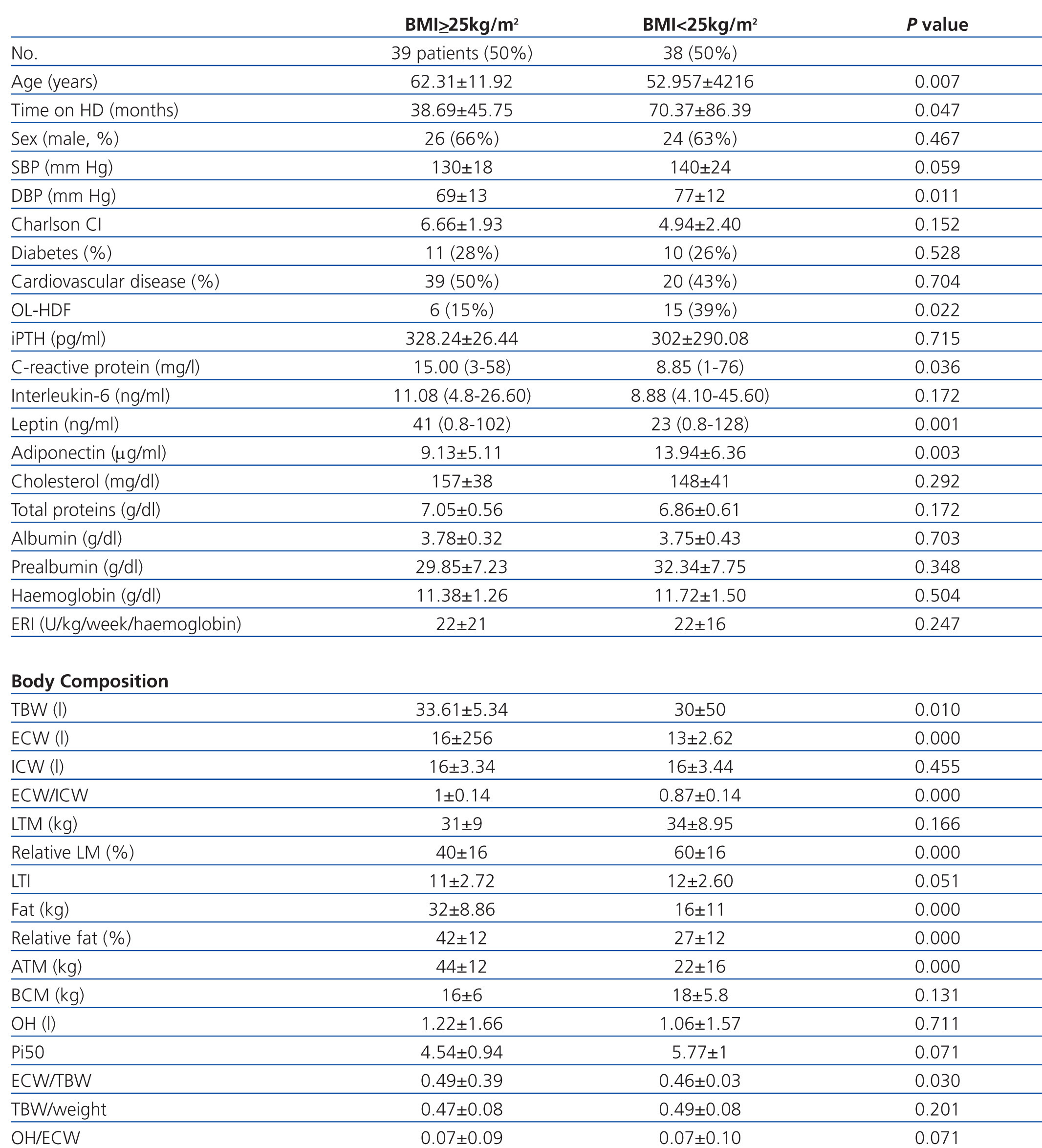
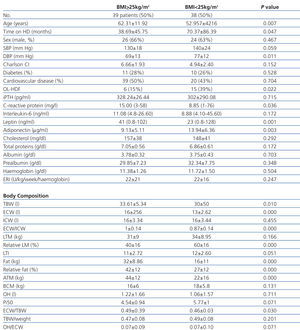
When comparing overweight and non-overweight patients (Table 1), we observed that overweight patients were older, had been on dialysis for less time, had lower diastolic blood pressure and used conventional HD techniques more often. The percentage of diabetics was not higher among overweight patients. Their CRP and leptin levels were higher while the adiponectin levels were lower, and there were no differences in the nutritional parameters or in erythropoietin needs.
In the analysis of body composition, overweight patients had a greater fat content, more ECW and a lower lean mass.
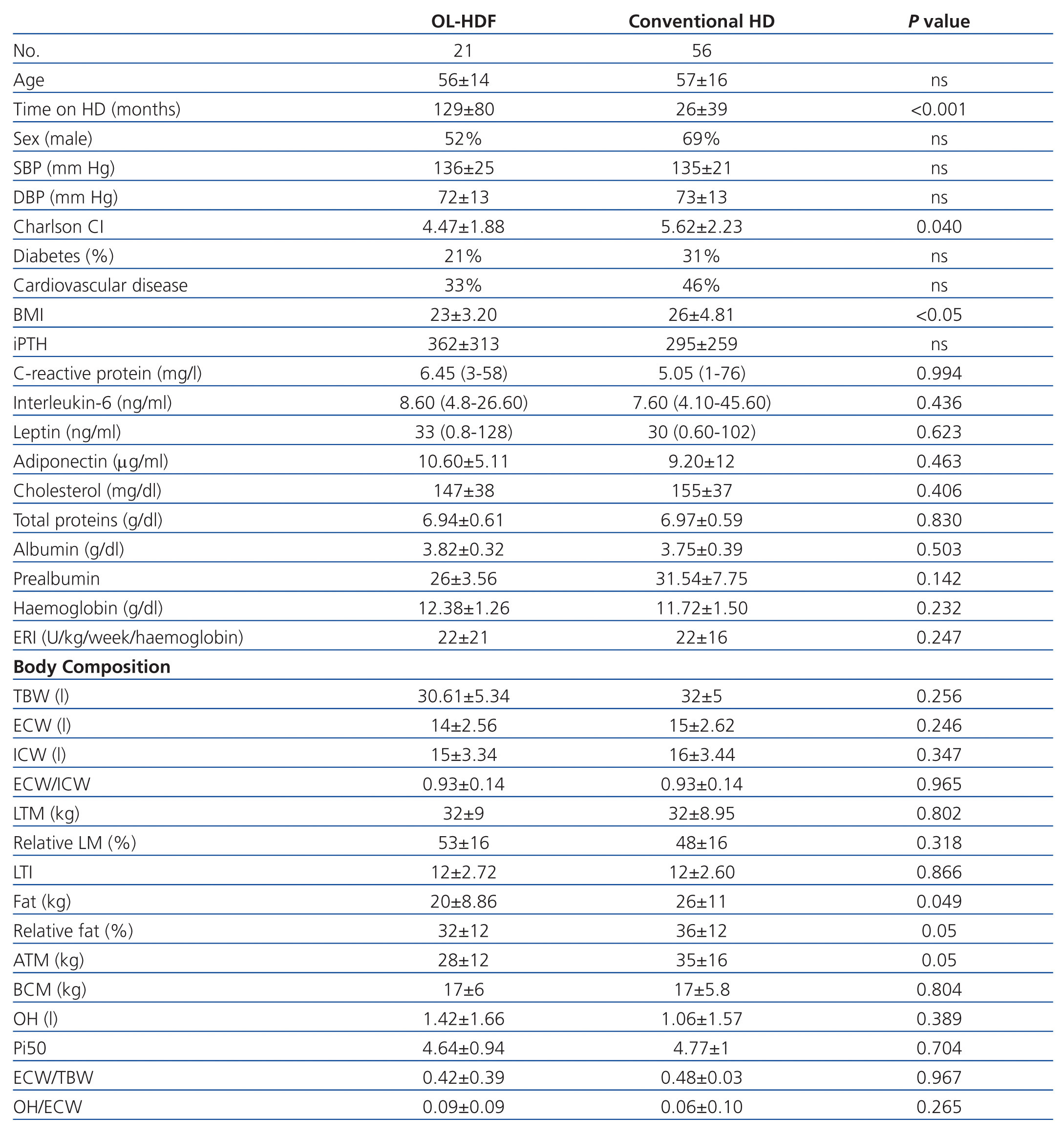
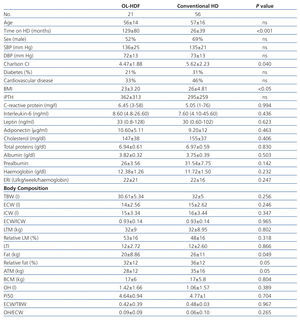
When comparing this data according to the HD technique (Table 2), we observed that the quantity of fat was lower in the group of patients who underwent OL-HDF. The HD time was greater, but the comorbidity and BMI were lower in those treated with OL-HDF. Levels of adipokines, nutritional and inflammatory parameters, and erythropoietin needs were not different between the two techniques.
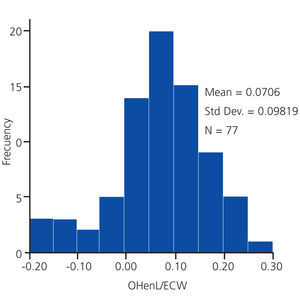
The distribution of the patients’ state of hydration is shown in Figure 1.
Some 16 patients were overhydrated (20.7%). When comparing over- and normo-hydrated patients, overhydrated ones had a higher Charlson comorbidity index (6.37±2.50 vs 5.03±2.04, P=.029), lower diastolic blood pressure (60±70 vs 76±12, P=.015), showed a tendency towards a higher ECW (15±5.15 vs 14±1.89, P=.255) and lower ICW (15±2.93 vs 16.35, P=.530), meaning that the ECW/ICW ratio (1.05±0.18 vs 0.90±0.11, P=.049) and OH normalised for ECW (0.20±0.05 vs 0.05±0.06, P<.001) were higher. Surprisingly, pre-HD weight was lower (61.49±10.9 vs 69.40±14.37, P=.044). The other clinical, biochemical or bioimpedance parameters did not show differences between the two groups.
Overall, 30% of patients had high levels of leptin, 10% high levels of IL-6 and only 1% had levels of adiponectin below the minimum values. Leptin levels were higher in females (26ng/ml; range: 1.4-128) than in males (4.70ng/ml; range: 2.20-58) (P<.01). There were no significant differences by gender in IL-6 and adiponectin levels.
Univariate correlations of adipokines, nutritional and inflammatory markers and parameters of body composition with the body mass index
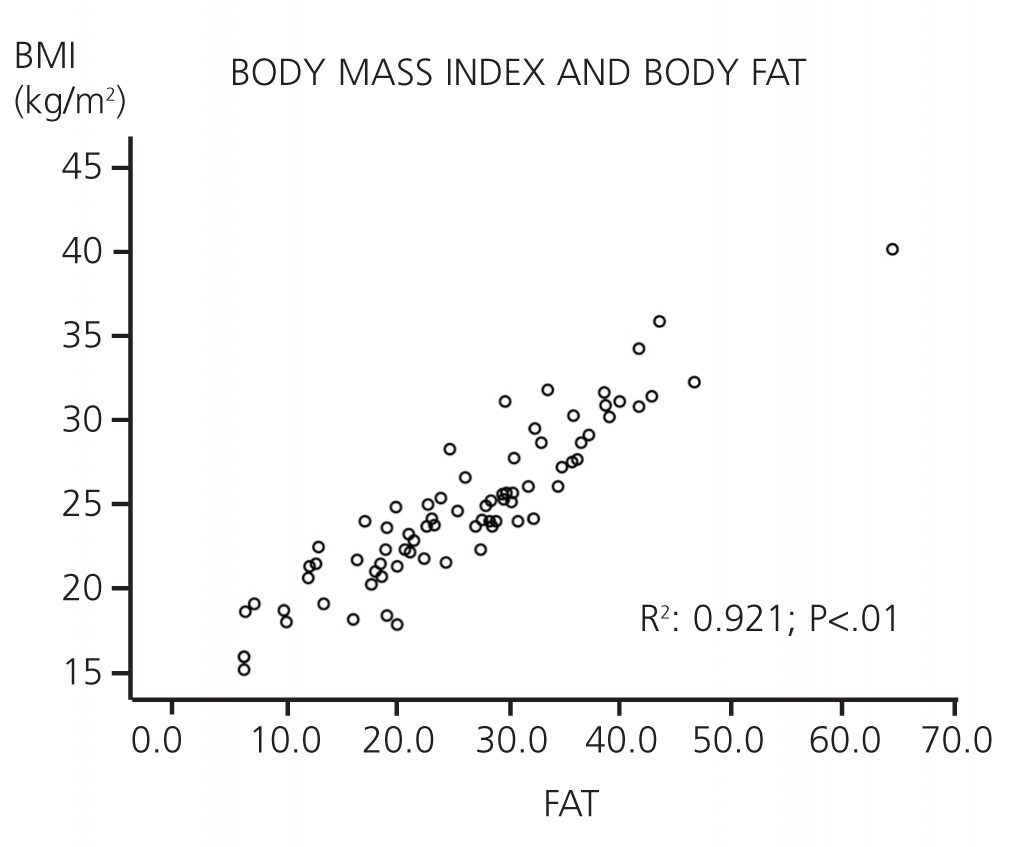
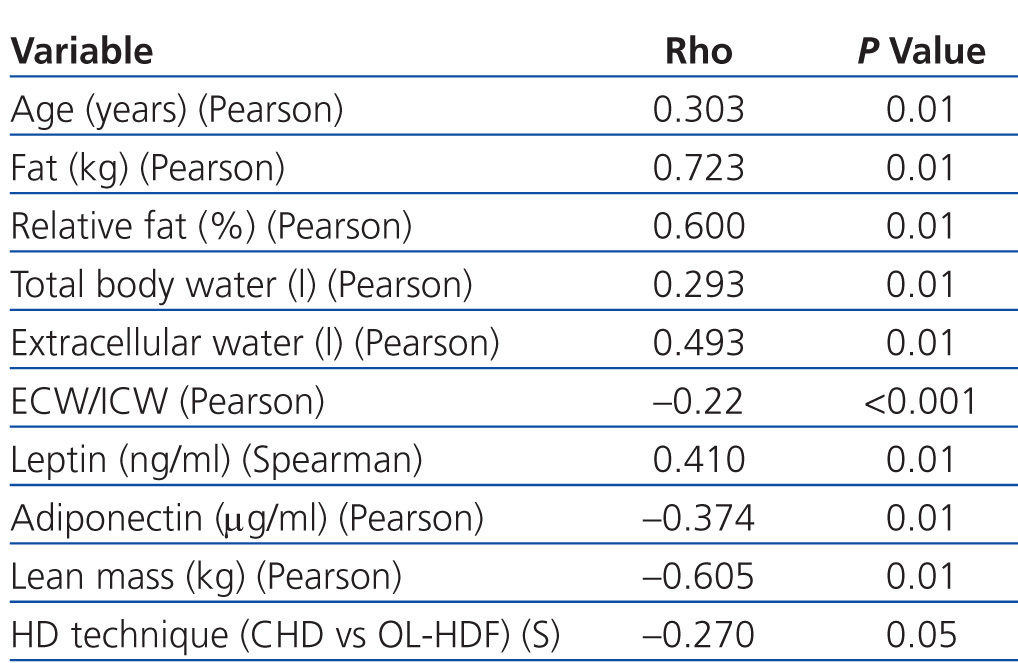
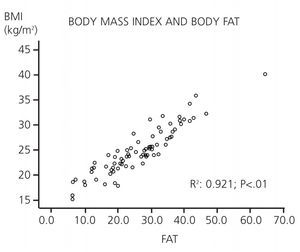
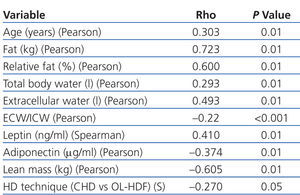
- There is a correlation between BMI and age (Pearson, P=.01), fat (Pearson, P<.001; Figure 2), body water (Pearson, P=.01) and leptin (Spearman, P=.01), and a negative correlation with lean mass (Pearson, P<.01), adiponectin (Pearson, P=.01) and HD technique (Spearman, P=.05) (Table 3). There is no correlation between BMI and normalised OH.
- CRP levels have a positive correlation with total fat (Spearman, P<.05) and IL-6 relates to age (Spearman, P<.05).
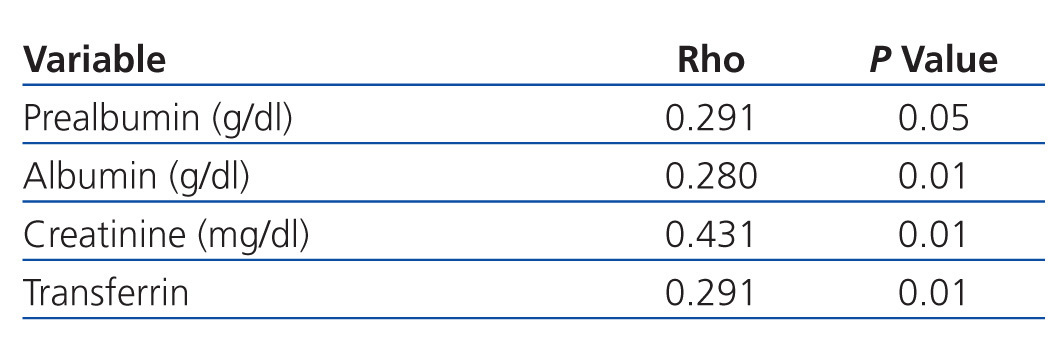
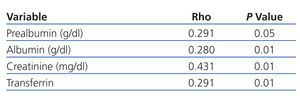
- Of the nutritional markers, prealbumin (Pearson, P<.05), albumin (Pearson, P<.05), total proteins (Pearson, P<.05), creatinine (Pearson, P<.01) and transferrin (Pearson, P<.01) relate to total and relative lean mass (Pearson, P<.05) (Table 4).
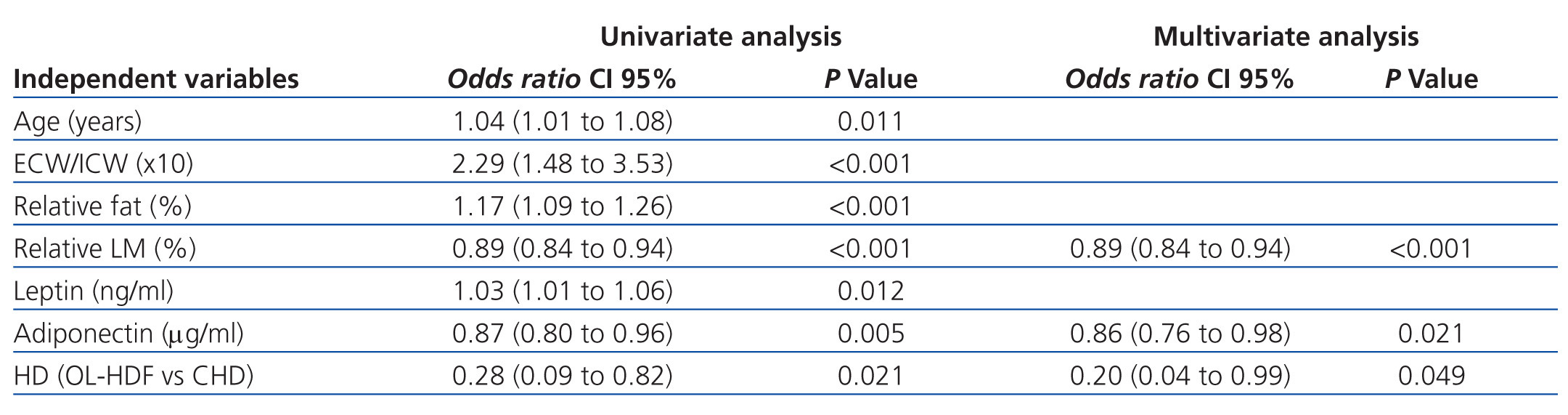
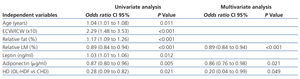
Univariate and multivariate multiple linear logistic regression analysis: possible predictive factors of overweight
The data from this section are shown in Table 5.
- In the univariate analysis, age, ECW/ICW ratio, relative fat and lean mass, leptin, adiponectin and HD technique (OL-HDF) were predictors of overweight.
- In the multivariate analysis, we introduced BMI≥25kg/m² as the dependent variable and the variables that had been predictors of BMI in the univariate analysis as independent variables. For each percentile point increase in lean mass, the risk of overweight dropped by 11% (odds ratio [OR]: 0.89; confidence interval [CI]: 0.84-0.94); for each percentile point increase in adiponectin, the risk of overweight decreased by 12% (OR: 0.86; CI: 0.76-0.98) and with HD technique (OL-HDF), the risk of overweight decreased by 80%, although the CI was very wide (OR: 0.20; CI: 0.04-0.99).
DISCUSSION
This observational study analyses the body composition of a population of HD outpatients and reveals, firstly, the high prevalence of overweight (50%), which was greater than OH (21%) and due mainly to a greater fat content. Furthermore, our results suggest that the different HD techniques could have an effect on body composition. Specifically, OL-HDF is associated with lower body fat than conventional HD, regardless of other confounding variables. We are aware of the small size of our sample, particularly with regard to OL-HDF patients, and the limitations of the observational nature of our design, but we hope that these results may be confirmed in subsequent studies. We are unaware of any publications showing this association between HD technique and body fat and overweight. The reason that the OL-HDF may contribute to reducing FM could be related to the finding that the serum concentration of leptin may be influenced by the type of membrane, achieving better purification with high flux10 membranes and haemodiafiltration with on-line reinfusion.11 Although we did not observe it, leptin is known to suffer a rebound effect related to the instant clearing of the solute,10 which could explain our results, as a consequence of possibly better purification in OL-HDF.
It has been argued whether the relation between adiposity and vascular risk factors in HD patients could be related to the leptin produced by the adipose tissue.18,19 This adipokine has a direct influence on blood pressure and may result in vascular damage through a central effect and a direct effect on the vessels and the heart.20 In contrast, several studies have suggested that the reduced levels of adiponectin and abdominal fat deposits21 are in fact responsible for vessel damage, finding an inverse relationship between adiponectin levels and BMI or FM.22 It is, furthermore, the adiponectin which has the predictive value of overweight and acts as a cardiorenal protector agent12 with anti-atherogenic and anti-inflammatory properties, especially the active form, high molecular weight adiponectin.22 There is an inverse relation with visceral abdominal fat in HD7 patients; this is the type of fat that is related to inflammation, malnutrition and an increase in mortality.22 Hipoadiponectinaemia is thought to be one of the mechanisms through which the accumulation of fat produces atherosclerosis. In fact Zocalli et al demonstrated that the group of patients on HD with lower adiponectin serum levels had a higher rate of cardiovascular events during the one-year follow-up.23 It seems that visceral fat would directly inhibit the secretion of adiponectin by the adipocytes.24 In our patients, the percentage of subjects with hipoadiponectinaemia was very low and there were no differences in the plasma levels of adiponectin depending on the type of membrane used. However, the levels of adiponectin were significantly lower in our overweight patients, and in this group there was a higher proportion of patients with cardiovascular problems, although this did not reach statistical significance.
Our findings confirmed a direct relationship between FM and leptin levels and BMI, and an inverse relationship between FM and adiponectin levels.
The greater survival of patients with a higher BMI observed in some studies could in fact suggest the existence of greater lean mass owing to greater protein intake.25 In our patients there was an inverse relationship between BMI and lean mass that can perhaps be explained by a more sedentary lifestyle that usually goes with obesity, as happens in the general population. The biochemical nutritional parameters studied related to lean mass. The better the nutrition, the higher the lean mass and the lower the BMI, while the worse the nutrition, the higher the fat content and the BMI. Lean mass was a predictive factor of the absence of overweight in our study.
OL-HDF has been associated to less inflammation,26 a more efficient elimination of uraemic toxins,27,28 a lower rate of cardiovascular events26 and better levels of 25 OH vitamin D.29 It is possible that the lower levels of fat in our patients on OL-HDF could explain the above mentioned facts.
While there is no evidence that the high flux membrane or the HDL-OL technique improve the prognosis of patients on dialysis, there seems to be a tendency towards this in some studies.30-33 It has not yet been clarified whether the improvement of the prognosis of OL-HDF patients is due to the use of high flux membranes or ultra pure water.31-36 Recent studies have not been able to demonstrate the benefit of OL-HDF over the control of anaemia, nutrition, mineral metabolism and the control of blood pressure or volume.37 We have observed that patients on OL-HDF had less fat but we have not observed differences in the state of hydration, the control of blood pressure, the needs of erythropoiesis-stimulating agents or nutritional parameters.
Finally, the greater prevalence of inflammation in CRF patients has been related to an increase in the expression of the leptin gene.38 In our experience, the inflammation measured by CRP is directly related to the increase in body fat and the BMI, and inversely related to adiponectin levels. We did not find a relationship between inflammatory markers and the extracellular volume as some studies suggested.12,39 Approximately 21% of our HD patients were overhydrated before dialysis, which is similar to the prevalence in other hospitals with a similar policy to ours concerning ideal weight.40 We found no differences in lean mass or FM between OH and non-OH patients.
We conclude that overweight in HD patients has a high prevalence (50%) and that the different HD techniques are associated to differences in body composition.
Our findings suggest that, in addition to restricting water and salt, we should recommend physical exercise to our patients.
The OL-HDF technique could reduce one of the factors of cardiovascular risk: overweight due to increased body FM.
Bioimpedance allows continuous assessment of the different parameters of body composition and it may prove to be a valuable ally for decisions regarding weight changes in dialysis patients.
Acknowledgements
We would like to thank Fresenius Medical Care for supplying the bioimpedance unit and financing the determinations of the adipokines.
We also would like to thank Dr Fernando García López for his help reviewing this paper.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Figure 1. Distribution of the state of normalised overhydration for extracellular water.
Figure 2. Correlation (Pearson) between body mass index and total fat in 77 haemodialysis patients.
Table 1. Clinical characteristics, levels of adipokines, nutritional and inflammatory markers and analysis of body composition of patients according to their BMI
Table 2. Clinical characteristics, levels of adipokines, nutritional and inflammatory markers and analysis of body composition of patients depending on the haemodialysis technique
Table 3. Bivariate correlation between body mass index and the study variables
Table 4. Binary correlation (Pearson) between lean mass and nutritional markers
Table 5. Univariate and multivariate multiple linear logistic regression analysis: possible predictive factors of overweight