Rivaroxaban is approved for preventing stroke and systemic embolism in adult patients with non-valvular atrial fibrillation (NVAF), with one or more risk factors. It is recommended that the Cockcroft-Gault (CG) equation be used for the dosing of this drug.1 However, the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation is the method of choice for determining kidney function and is the equation used by the majority of laboratories in Spain.2 There are discrepancies in values calculated using the two equations which may cause errors in prescribed doses of rivaroxaban.3,4 Prescription of inappropriate doses is linked to an adverse cardiovascular prognosis.5 The objective of our study was to identify groups of patients in whom the CKD-EPI and CG equations can be used indiscriminately with a low risk of prescription error.
An observational, retrospective study was conducted of patients with atrial fibrillation or atrial flutter seen at a cardiology clinic between November 2012 and December 2014. Patients with metal stent implantation or moderate to severe rheumatic mitral stenosis, for whom serum creatinine levels in the past 12 months were not available, or for whom body weight was not recorded at the clinic, were excluded.
A total of 571 patients were enrolled, with a mean age of 69 years (±13.6 years), CHA2DS2VASc 2.8±1.7 and HAS-BLED 1.2±0.8. (CHA2DS2VASc is: Congestive heart failure, Hypertension, Age, Diabetes mellitusStrokeVascular disease, Age, Sex.HAS-BLED is: Hypertension, Abnormal renal and liver function, Bleeding, Labile INRs, Elderly, Drugs or alcohol.) Table 1 shows the patients’ baseline characteristics
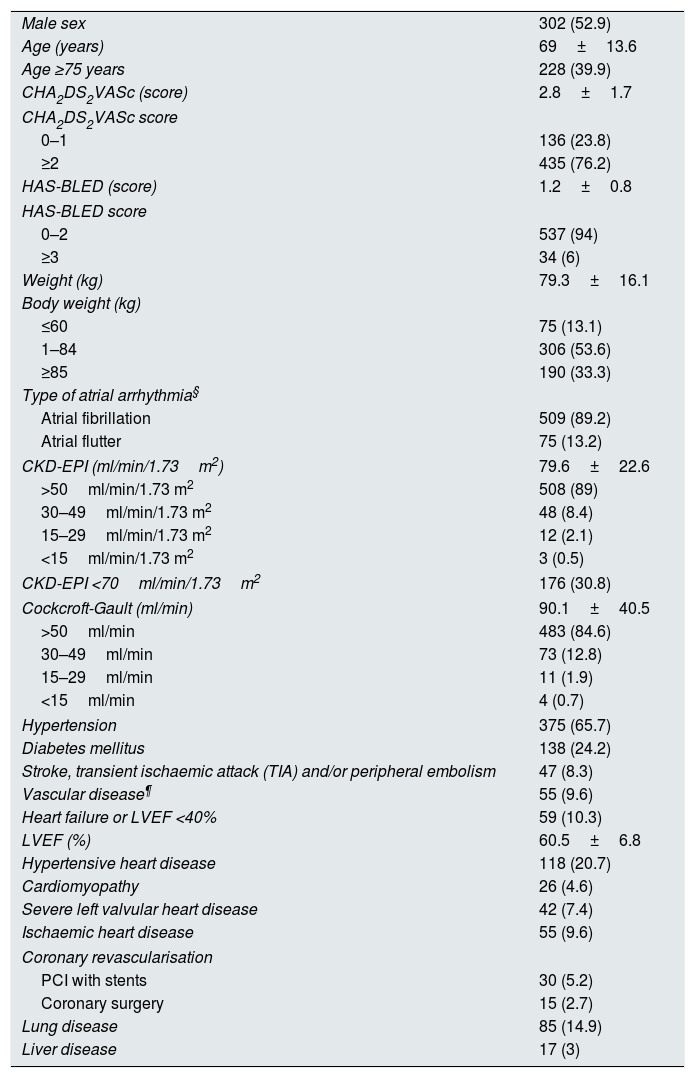
Clinical data corresponding to the sample (n=571).
| Male sex | 302 (52.9) |
| Age (years) | 69±13.6 |
| Age ≥75 years | 228 (39.9) |
| CHA2DS2VASc (score) | 2.8±1.7 |
| CHA2DS2VASc score | |
| 0–1 | 136 (23.8) |
| ≥2 | 435 (76.2) |
| HAS-BLED (score) | 1.2±0.8 |
| HAS-BLED score | |
| 0–2 | 537 (94) |
| ≥3 | 34 (6) |
| Weight (kg) | 79.3±16.1 |
| Body weight (kg) | |
| ≤60 | 75 (13.1) |
| 1–84 | 306 (53.6) |
| ≥85 | 190 (33.3) |
| Type of atrial arrhythmia§ | |
| Atrial fibrillation | 509 (89.2) |
| Atrial flutter | 75 (13.2) |
| CKD-EPI (ml/min/1.73m2) | 79.6±22.6 |
| >50ml/min/1.73 m2 | 508 (89) |
| 30–49ml/min/1.73 m2 | 48 (8.4) |
| 15–29ml/min/1.73 m2 | 12 (2.1) |
| <15ml/min/1.73 m2 | 3 (0.5) |
| CKD-EPI <70ml/min/1.73m2 | 176 (30.8) |
| Cockcroft-Gault (ml/min) | 90.1±40.5 |
| >50ml/min | 483 (84.6) |
| 30–49ml/min | 73 (12.8) |
| 15–29ml/min | 11 (1.9) |
| <15ml/min | 4 (0.7) |
| Hypertension | 375 (65.7) |
| Diabetes mellitus | 138 (24.2) |
| Stroke, transient ischaemic attack (TIA) and/or peripheral embolism | 47 (8.3) |
| Vascular disease¶ | 55 (9.6) |
| Heart failure or LVEF <40% | 59 (10.3) |
| LVEF (%) | 60.5±6.8 |
| Hypertensive heart disease | 118 (20.7) |
| Cardiomyopathy | 26 (4.6) |
| Severe left valvular heart disease | 42 (7.4) |
| Ischaemic heart disease | 55 (9.6) |
| Coronary revascularisation | |
| PCI with stents | 30 (5.2) |
| Coronary surgery | 15 (2.7) |
| Lung disease | 85 (14.9) |
| Liver disease | 17 (3) |
Qualitative variables are expressed in terms of n (%). Quantitative variables are expressed in terms of mean±standard deviation. PCI: Percutaneous coronary intervention. LVEF: Left ventricular ejection fraction. (CHA2DS2VASc is: Congestive heart failure, Hypertension, Age, Diabetes mellitusStrokeVascular disease, Age, Sex.HAS-BLED is: Hypertension, Abnormal renal and liver function, Bleeding, Labile INRs, Elderly, Drugs or alcohol.)
§ A single patient may present atrial fibrillation and atrial flutter.
¶ Peripheral artery disease, myocardial infarction and/or atheromatous plaques in aorta.
Using the CKD-EPI equation, 41 patients (7.2%) would receive inappropriate dosing of rivaroxaban (nine due to underdosing and 32 due to overdosing). In particular, 509 (89.1%) would receive 20mg daily, 59 (10.3%) would receive 15mg daily and three (0.5%) would have a contraindicated prescription. Using the Cockcroft-Gault formula (CG), 487 individuals (85.3%) would receive a daily dose of 20mg, 80 (14.0%) would receive a daily dose of 15mg and four (0.7%) would have a contraindicated prescription.
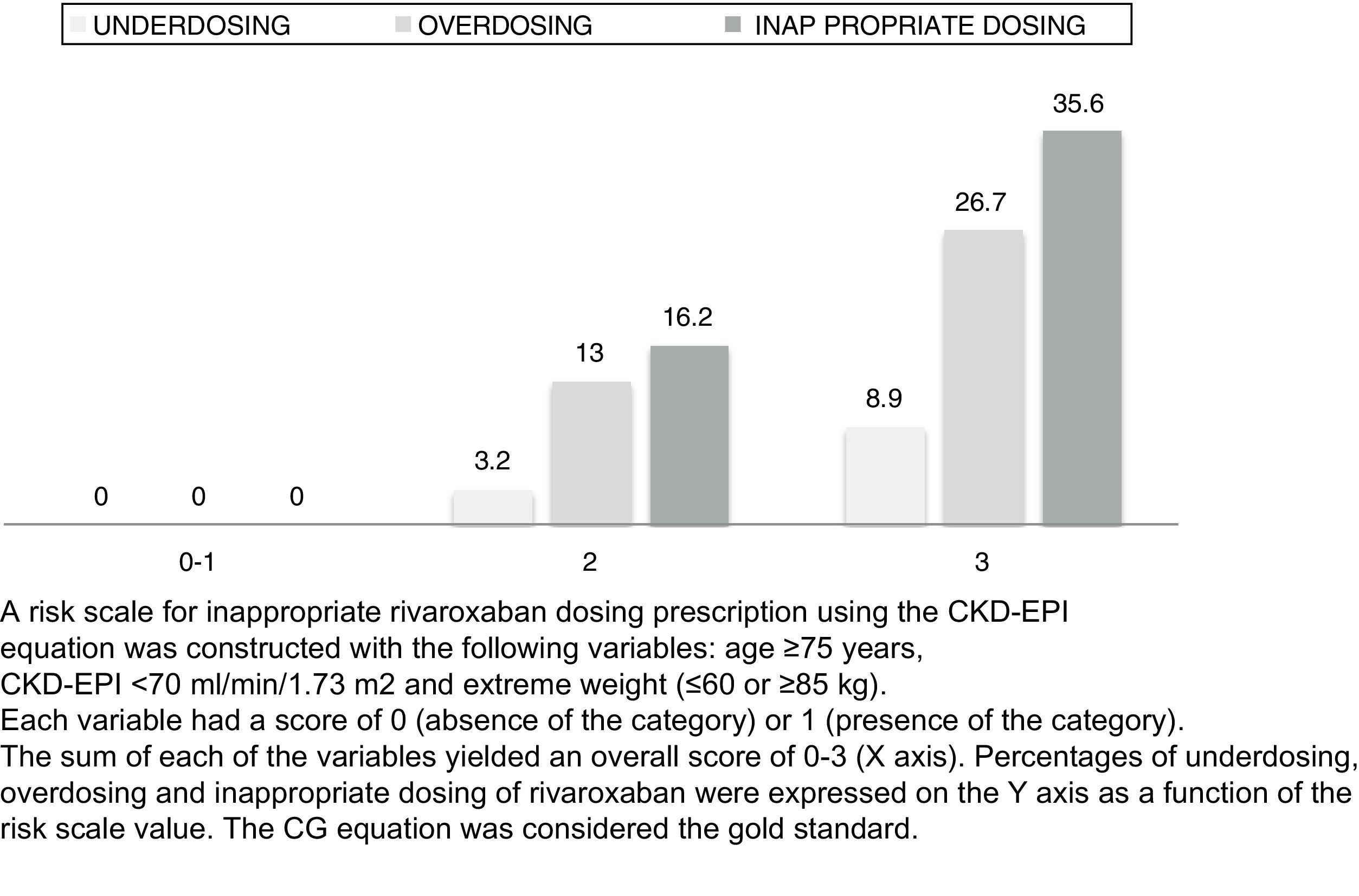
In the univariate analysis, variables linked to a higher likelihood of receiving inappropriate dosing were the CHA2DS2-VASc scale (p<0.001), HAS-BLED ≥3 (17.6% versus 6.5%; p=0.028), creatinine (p<0.001); age (p<0.001), weight (p<0.001) and CKD-EPI (p<0.001). Among patients with dosing discrepancies, CKD-EPI values were 56.44±10.93ml/min/1.73m2 (p10=43.6; p90=68.9). In the multivariate analysis, significant predictive factors for receiving inappropriate dosing were extreme weight ≤60kg or ≥85kg (2.5 95% confidence interval [CI] 1.2–5.3; p=0.013), age ≥75 years (7.4 95% CI 2.7–20.4; p<0.001) and CKD-EPI <70ml/min/1.73m2 (23.1 95% CI 6.9–77.7; p<0.001).
A scale was constructed with these variables wherein one point was assigned to each value present (Fig. 1). A score ≥2 identified patients susceptible to receiving inappropriate dosing with a sensitivity of 100%, a specificity of 70.2%, a positive predictive value (PPV) of 20.6% and a negative predictive value (NPV) of 100%. The receiver operating characteristic (ROC) curve was 0.88 (95% CI 0.85–0.92) (p<0.001). In these patients, estimated creatinine clearance (eCrCl) and estimated glomerular filtration rate (eGFR) should be determined and, in the event that such discrepancy is confirmed, more specific testing should be done (24-h urine creatinine clearance) and the risk/benefit ratio individually assessed of selecting a high or low dose or a different direct oral anticoagulant (DOAC) with no dosing discrepancies depending on the formula used.6 In individuals with less than two criteria, the CKD-EPI and CG equations can be used indiscriminately. Hence, using this scale, calculation using the CG equation could be limited to 34.9% of patients.
The sample size was small, especially in patients with stage 3–5 kidney disease, and this might have limited the statistical power. Larger studies will be needed to confirm the external validity of our results.
FundingAlejandro Isidoro Pérez Cabeza and Francisco Ruiz Mateas declare that they have received consulting fees from Bayer Hispania, S.L.
Please cite this article as: Pérez Cabeza AI, Górriz JL, Bravo Marqués R, Chinchurreta Capote PA, López Tejero S, González Correa JA, et al. Factores de predicción de dosificación inadecuada de rivaroxabán utilizando la ecuación de CKD-EPI. Nefrologia. 2021;41:216–218.