According to all clinical guidelines, autologous arteriovenous fistula (AVF) in the upper limb is the vascular access of choice for haemodialysis,1–3 although a high percentage of them (up to 50%) will not mature or be used.4 For this reason, multiple intraoperative tools have been proposed to try to predict patency and future maturation, with immediate postoperative flow measured by Doppler ultrasound being one of the most useful.5–9 However, this technique has important limitations; it is operator-dependent and requires dedicated equipment and training. As an alternative method to predict flow and maturation, the use of thermal cameras has been proposed, due to their ease of use, reproducibility and low cost. Thermal cameras could help to change the surgical strategy within the same intraoperative period, and prevent patients from leaving the surgical area with access routes destined to fail.
The aim of our study was to demonstrate a decrease in distal temperature following the creation of an AVF during the immediate postoperative period, and a negative correlation between this temperature change and AVF flow. We conducted a prospective observational study over a six-month period, including patients with stage IV-V chronic kidney disease who were candidates for native AVF creation in our centre, under local anaesthesia and without previous access.
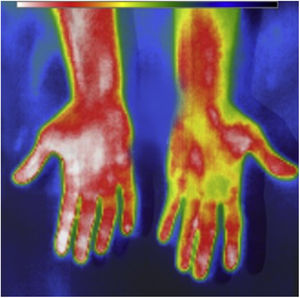
Temperature was measured using a portable thermal camera (Fig. 1) and fistula flow was measured by Doppler ultrasound, pre-operatively and immediately post-op, using the hand on the non-operated side as a control. For the flow calculation we used the formula: Qa (ml/min) = Area in cm2 (0.785 × D2, in cm2) × mean velocity (cm/s) × conversion factor (0.06).2,3 Univariate analysis was performed using parametric tests; Chi-square and t-test for paired samples for the study of pre-post temperature and flow changes in each arm. The t-test for independent samples was used to compare the relative temperature changes between the two arms.
We included a total of 52 patients, whose characteristics are shown in Table 1. The temperature in the hand on the operated arm decreased by 0.91 °C (±2.34) post-intervention (p = 0.003), and the relative change in temperature between the two hands was −1.15 °C (p = 0.015). Flow in the proximal humeral artery increased by 621.6 ml/min (±548.5; p < 0.001). There was a trend towards higher flow velocity in the AVF at lower postoperative hand temperature. However, this correlation was not statistically significant (R = −0.117, p = 0.418).
Characteristics.
| Characteristics | n = 52 | Percentage |
|---|---|---|
| Age (years) | 67.3 | (SD ± 13.9) |
| Sex | ||
| Female | 21 | 40.4 |
| Male | 31 | 59.6 |
| Comorbidities | ||
| Dialysis | 18 | 34.6 |
| Diabetes | 20 | 38.5 |
| HT | 49 | 94.2 |
| DLP | 27 | 51.9 |
| Coronary heart disease | 6 | 11.5 |
| Treatment | ||
| Antiplatelet therapy | 10 | 19.2 |
| Anticoagulation | 2 | 3.8 |
| AVF | ||
| Side | ||
| Left | 45 | 86.5 |
| Right | 7 | 13.5 |
| Type | ||
| Distal | ||
| Radio-cephalic | 28 | 53.8 |
| Proximal | ||
| Brachial-cephalic | 20 | 38.5 |
| Brachial-basilic | 2 | 3.8 |
| Brachial-perforating | 2 | 3.8 |
AFV, arteriovenous fistula; HT, hypertension; SD, standard deviation; DLP, dyslipidaemia; SD, standard deviation.
The other variables analysed, including demographics, comorbidities and the characteristics of the fistula performed, were not statistically significantly in relation to the relative change in temperature. A linear regression was also performed with the variables analysed to identify independent prognostic factors that could be predictors of AVF flow, with temperature changes being excluded as a predictor.
By way of discussion, we know that creating an AVF preferentially distributes arterial flow to the low resistance venous territory rather than the distal arterial system of the limb, due to the increased distal peripheral resistance, and this could result in a decrease in temperature of the ipsilateral hand due to hypoperfusion. Our results, both in the comparison of pre- and post-surgery temperatures and in the relative temperature change in the hand on the operated arm, showed that these changes occur immediately after creation. However, we did not find a relationship between this decrease in temperature and the increase in postoperative fistula flow which would enable us to associate them and recommend their use as a predictor of AVF flow or its subsequent maturation.
In a previous study,10 a thermal camera was also used to measure temperature distal to the AVF (as a binary factor for cooling or non-cooling of the limb), and significantly predicted correct maturation and patency of the AVF with a sensitivity of 96% and 96% and a specificity of 68% and 69% respectively. However, they did not compare temperature change with postoperative flow. Our results, even when redoing a secondary analysis by binary groups (cooling or not) do not support this relationship (p = 0.331), so we believe if it is not significantly related to intraoperative fistula flow, it is unlikely to be useful as a predictor of maturation.
In conclusion, we found that there was a decrease in distal temperature following the creation of the fistula in the hand on the operated arm. However, according to our results, this change was not significantly related to AVF flow and temperature changes are therefore unreliable as a predictor of maturation.