To the Editor:
Central venous disease is a common issue in patients on haemodialysis following the creation of an arteriovenous fistula (AVF). The primary treatment of stenosis/occlusion of the central vein consists of recannalising the vein using endovascular techniques: percutaneous trans-luminal angioplasty (PTA) with or without stent placement. However, the venous patency produced by these procedures is limited, and on occasions, the fistula must be surgically closed due to symptoms of venous hypertension. We propose a simpler and less aggressive approach for closure, through ultrasound-guided thrombin injection.
CASE REPORT 1
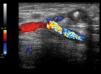
Our first patient was a 78-year old female on haemodialysis since 2009 with a left humerocephalic AVF. The patient developed oedema in the arm with the AVF, which produced progressively worsening pain and functional impairment. The patient was diagnosed with occlusion of the subclavian vein, and several attempts at PTA resulted in early recurrence. We decided to place a right central venous catheter and to close the AVF due to poor functioning. The AVF was annulled through ultrasound-guided injection of thrombin (Figure 1) into the cephalic vein, producing thrombosis. Ten days later, the oedema had disappeared and the artery was again patent with no symptoms.
CASE REPORT 2
Our second patient was a 74-year old female on haemodialysis since 2010 with a right humerocephalic fistula, which developed pain and increased volume of the right arm, producing functional impairment and poor functioning of the AVF (Figure 2). We performed a phlebography of the right arm, observing obstruction of the subclavian vein. We attempted to re-establish patency using endovascular techniques with no success. Given the progressively worsening symptoms, we decided to place a central jugular venous catheter and to close the AVF. We injected thrombin into the cephalic vein under ultrasound guidance approximately 4-5cm from the AVF and confirmed thrombosis. In a follow-up consultation 7 days later, the patient reported improvements in sensations of pain, although oedema remained. A Doppler ultrasound analysis revealed patency along the first few centimetres of the cephalic vein, but the rest of the vein was thrombosed up to the junction with the axillary vein. We performed another proximal injection, obtaining thrombosis of the entire cephalic vein. Seven days later, the oedema had disappeared (Figure 3). A follow-up Doppler ultrasound analysis confirmed occlusion of the cephalic vein and patency of the humeral artery.
DISCUSSION
Between 17% and 40% of patients on haemodialysis will develop central vein stenosis due to multiple cannalisations.1,2 This can produce incapacitating oedema due to venous hypertension in up to 40%-50% of cases.2,3 Initial treatment generally involves angioplasty with or without stent placement. However, the duration of this solution is limited, producing primary patency and assisted patency rates of 20%-30% and 60%-70%, respectively, after 12 months.3,4 In addition, more than 50% of patients will require subsequent interventions.5 Revascularisation through open surgery involves higher rates of morbidity, and surgical interventions produce a final patency that is similar to that produced by repeated endovascular procedures.6 Approximately 50% of patients on haemodialysis with central venous stenosis finally require ligation of the AVF, and this is particularly common in patients that produce no or only minimal initial responses to endovascular treatment.6 Closure of the fistula is commonly performed using surgical techniques, through dissection of the area of the anastomosis and ligation of the fistula under local anaesthetic. This intervention is not without risks, since it involves operating on an arm with oedema in an area that has already undergone multiple interventions due to complications of the AVF. In our case, we closed the AVF by injecting thrombin directly into the arterialised vein under ultrasound control. This provides the advantages of being more comfortable for the patient (avoids the need for subsequent interventions), is less expensive, and produces fewer complications.
For this procedure, we applied compression to the upper arm until flow to the fistula was completely occluded, thus preventing the possibility of migration of the thrombus, although even if this were to occur, it would not produce any clinical repercussions since the subclavian vein was also occluded. We used Doppler ultrasound guidance to locate the fistula and then continued 4-5cm distally along the vein in order to avoid accidental injection of thrombin into the artery. We then placed the needle into the arterialised vein in the direction of blood flow, in order to avoid migration of the thrombin towards the artery, and injected the thrombin until thrombosis was achieved. Finally, after removing compression, we placed a compressive bandage on the arm for 48 hours.
We performed this technique on two obese patients, after several failed attempts at re-establishing patency and with symptoms that incapacitated the patients. In both cases, the AVF was closed with no complications. This is a simple, fast, inexpensive, and comfortable technique for the patient and physician, and should be taken into account as a treatment alternative when planning to close an AVF.
Conflicts of interest
The authors state that they have no potential conflicts of interest related to the content of this article.
Figure 1. Humerocephalic anastomosis following the injection of thrombin
Figure 2. Internal right humerocephalic arteriovenous fistula with severe oedema and erythematous areas
Figure 3. Clear improvement following closure of the arteriovenous fistula