Objetivo: Describir las características y el pronóstico de pacientes con diabetes mellitus (DM) tipo 2 en diálisis peritoneal (DP) y compararlo con el de los no diabéticos (NoDM). Métodos: Estudio de cohorte prospectivo de todos los pacientes incidentes en DP en el registro del Grupo Centro de DP (2003-2006). Se recogen datos basales, eventos cardiovasculares (CV) previos, ingresos, peritonitis, trasplantes y exitus. Resultados: Los 65 pacientes DM tipo 2 son mayores, con mayor tasa de eventos CV previos (60,9 vs. 17,7%) y peor control de la presión arterial al inicio de DP que los 376 pacientes NoDM. Los DM tipo 2 tienen una mayor tasa de hospitalización (1,1 [0,9-1,4] vs. 0,6 [0,5-0,7] ingresos por año en riesgo), pero similar eficacia de la DP y control de la anemia. Los DM tipo 2 tienen una supervivencia en técnica menor que los NoDM (870 vs. 1002 días; p = 0,009 según la estimación de Kaplan-Meyer) y una mayor tasa de mortalidad anual (13,7 vs. 4,1%; p = 0,021), con una HR de mortalidad de 2,5 [1,1-5,6] tras la corrección por la edad. La asociación entre DM tipo 2 y eventos CV previos excluye la variable DM tipo 2 del modelo multivariante. La probabilidad de supervivencia a los dos años es del 86,7% en NoDM y del 72,5% en DM tipo 2. Conclusión: Los DM tipo 2 presentan un mayor porcentaje de eventos CV previos y peor pronóstico vital. Los eventos CV previos pueden explicar gran parte de este riesgo.
INTRODUCTION
Traditionally, it was understood that patients with type 2 DM would benefit from certain advantages offered by PD. Improved control of volaemia and blood pressure, the continuous dialysis and the preservation of residual renal function (RRF) were a few of the advantages cited for PD.1 In addition, cardiovascular problems (CV), haemodynamic instability and the need for vascular access creation can make haemodialysis (HD) less suitable for these patients. However, metabolic problems associated with PD may have a harmful effect on patients with type 2 DM.1
The Spanish Society of Nephrology¿s (SEN) register of kidney patients reports an increased prevalence of DM in dialysis programmes, in keeping with the increase in metabolic and obesity problems in the general population, which makes this issue more relevant.2
Studies that attempted to compare the progress of patients on haemodialysis (HD) to those on PD have had ethical and methodological problems, and on some occasions, they even produced contradictory results. There seems to be a consensus that PD outcomes are better than on HD during the first two years, after which this tendency reverses.3-5 In addition, none of these studies makes any specific recommendations for DM patients.
For this reason, we have analysed the outcomes of our patients at the GCDP (Peritoneal Dialysis Centre Group) based on data for patients incident during three years (2003-2006). In particular, we have concentrated on the characteristics, outcomes and factors determining the prognosis of incident patients with type 2 DM.
PATIENTS AND METHODS
This was a multi-centre prospective observational epidemiologic study with systematic consecutive sampling and a maximum follow-up of three years. The study¿s primary objective was to compare the outcomes of patients undergoing PD who have type 2 DM with those who are not diabetic (Non-DM). Our secondary objective was to examine the management and characteristics of these patients and to identify possible risk factors.
The GCDP is made up of 18 public hospitals in the center of Spain which are responsible for the health of 8.8 million inhabitants in that area. During three years (from January 2003 to January 2006), data was collected from all incident PD patients from the start of PD and during follow-up until the treatment was stopped or death occurred. We recorded demographic parameters, aetiology, comorbidity, origin and whether the technique was freely chosen or imposed. Comorbidity was calculated using the Charlson Comorbidity Index (CCI), which gives a score based on 16 comorbid conditions and the patient¿s age, previously been validated for PD.6 Diagnoses of CV events are based on clinical criteria: stroke, peripheral artery disease, coronary artery disease and heart failure class II or higher using the NYHA classification. At the initiation of dialysis and then on a weekly basis we recorded data such as technique type, adequacy, residual renal function (RRF), peritoneal transport, treatment for anaemia and control of blood pressure (BP). Baseline data on adequacy and peritoneal kinetics were obtained between four and six weeks after the start of the treatment. Events such as peritonitis, hospitalisation or leaving the programme were recorded when they occurred. We assessed compliance with the standards recommended for adequacy, anaemia and BP control described in current guidelines.7
Database design, management and analysis were undertaken by the scientific committee with no participation of the companies that provide funding. A Data Manager audited and sorted out the data by ranges and rational practices. Statistical management and analysis were performed using SPSS software version 11.0. The group discussed interim analyses yearly.
Numerical variables were shown as mean and standard deviation (SD). Comparisons were made using the Student¿s t-test or the Chi-square test, according to the nature of the variables. Survival data was analysed using the Kaplan-Meier method, considering different events where applicable. In the patient mortality analysis, death is the event, and leaving the programme for any other reason (change of technique, recovery of renal function, transplant or transfer) is censored. For the analysis of PD technique failure, changing to HD is the event, and for the analysis up to first episode of peritonitis, this is considered the event. Survival data are shown as a mean survival probability and 95% confidence interval (CI). The Cox proportional hazard model was used to establish hazard ratio (HR) values. We included those variables with a p <0.1 for the univariate analysis in a backward stepwise regression model, based on the likelihood ratio statistic and verifying possible confounders. For the final model, we verified that there was proportionality in the risk level throughout the study.
All rates obtained (for mortality, hospitalisations and peritonitis) refer to the real time each patient was undergoing treatment and are shown with a CI of 95%.
COHORT DESCRIPTION
The cohort is composed of 469 patients between January 2003 and January 2006, with a mean follow-up period of 13.4 months (ranging from 2 to 36 months). The most relevant baseline characteristics were as follows: mean age 53.6 years (SD 16.1), 61.6% male, CCI 5.2 (SD 2.5), 19% diabetic and 23.7% had history of a previous CV event. Of this cohort, 65 type 2 DM patients and 380 non-DM patients were selected for the analysis; the 24 type 1 DM patients were excluded.
Before entering the PD programme, the patients selected have had the following events: 8.4% had an acute myocardial infarction, 12.8% had peripheral artery disease (1.6% with a major amputation), 4.8% had a stroke, and 7.1% had episodes of heart failure (NYHA class II or above). 89.9% suffered from high blood pressure, 83.6% were under treatment, 19.2% had haemoglobin levels (Hb) <11g/dl. 90.4% had chosen PD freely, and the rest were following medical advice and 36.9% of the patients were included on the transplant waiting list during the first six months.
The most prevalent aetiologies for chronic kidney disease were: glomerular disease 26.8%, diabetic nephropathy, ischaemic or renovascular disease 12.6%, interstitial nephropathy 14.2%, and adult polycystic kidney disease 11.5%. The initial technique was continuous ambulatory PD (CAPD) for 66.9% of the patients, and automatic PD (APD) for the rest. Table 1 shows additional descriptive data. At the end of the follow-up period, 21.0% of the patients had received a transplant, 6.6% had died, 7.5% had changed to HD and 1.5% had recovered renal function. The rest remained on PD. Contact was lost with three patients (0.7%).
RESULTS
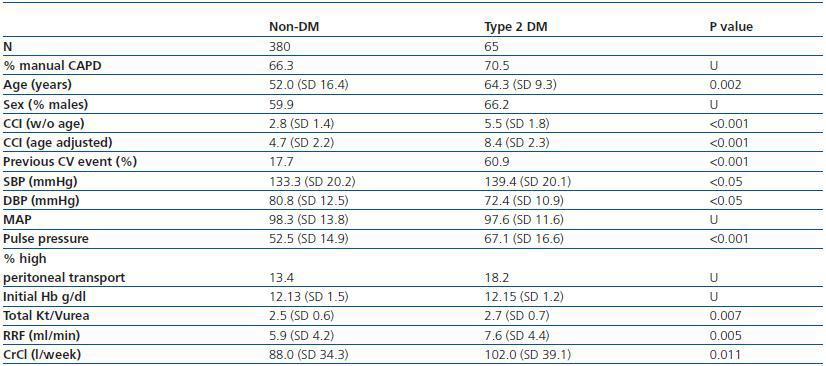
Baseline characteristics and compliance with standards: The clinical characteristics of patients with type 2 DM are significantly different from those from the Non-DM group (table 1). The type 2 DM group is older, with higher CCI, increased prevalence of previous CV events, and higher systolic BP and pulse pressure. However, they also have higher RRF and Kt/Vurea values and higher total weekly creatinine clearance (CrCl).
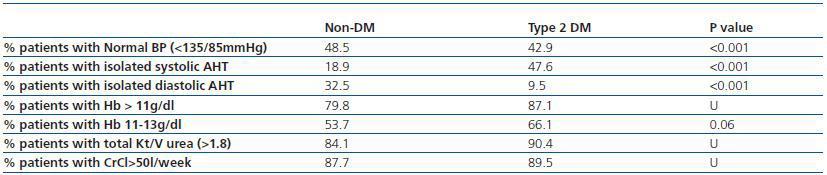
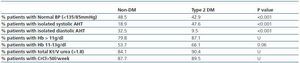
When we examined whether BP targets were achieved, we see that results are poorer among diabetics (table 2). However, there were no differences in other parameters, such as adequacy of dialysis or correction of anaemia.
Mortality: 28 patients died during follow-up, thus the overall annual mortality risk is calculated at 5.2% [95% CI, [3.7-7.8%]. The annual mortality rate for the type 2 DM patients was 12.4% [95% CI, 4.7-20.1% compared with 4.1% [95% CI, 2.1-6-0%] for the non diabetics. The causes of death in type 2 DM patients were 50% cardiac, 10% vascular, 20% infectious, 10% cancer and 10% from other causes. In non-diabetics, the leading cause of death was also CV (33% cardiac and 11.1% vascular).
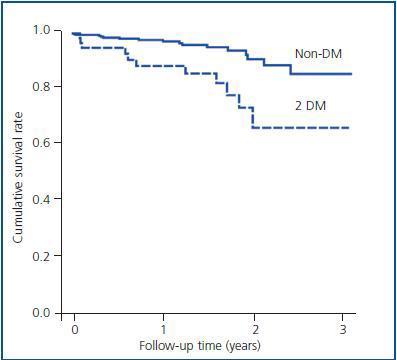
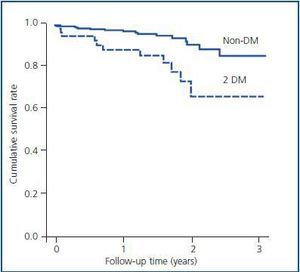
The survival rate for type 2 DM patients was significantly lower, as shown in figure 1 (log-rank 11.4 p = 0.001). The probability of surviving two years in non-DM patients is above 90%, while in type 2 DM patients the probability of surviving two years is only 68%. In the Cox proportional hazards model, the presence of type 2 DM indicated a higher risk of death (HR 2.5 [95% CI, 1.1-5.6], adjusted for age). When we introduce the history of a previous CV event in the model, DM loses significance within that model, due to the association between type 2 DM and CV disease and the latter¿s strong association with mortality. None of the analysed factors (blood pressure, effectiveness of PD, residual renal function or baseline haemoglobin level) were significant in the multivariate model.
Morbidity (hospitalisations and peritonitis): The annual risk of hospitalisation for the whole population was 0.67 [95% CI, 0.60-0.74].
Patients with type 2 DM had an annual risk of hospitalisation of 1.1 [95% CI, 0.9-1.3] compared with 0.6 [95% CI, 0.5-0.7] in non-diabetics.
Regarding loss of RRF, the type 2 DM group showed a similar reduction in GRF to that of the non-DM group: 1.6 (SD 6.3) ml/min per year vs. 1.5 (SD 3.4) ml/min per year.
Patients with type 2 DM tended to have a higher rate of peritonitis than the non-DM group, but his was not statistically significant. The annual risk of developing peritonitis in type 2 DM patients was 0.53 episodes [95% CI, 0.4-0.7] compared with 0.49 [95% CI, 0.4-0.5] in the Non DM group. The length of time elapsed before the first peritonitis episode was not different between the groups (log-rank 3, 7, p=0.2).
Technique survival: Type 2 DM patients had a lower technique survival rate (log-rank 6.7, p = 0.009), with an HR of 2.4 [1.2-4.9], without age, gender, imposed referral to PD or achieving guideline targets acting as confounders.
The probability of technique survival at two years was 86.7% in non-DM patients and 75.2% in DM 2 patients.
DISCUSSION
Our study provides current, reliable data on patient characteristics, achievement of guideline targets, hospitalisation and mortality rates in type 2 DM patients who undergo PD in our area. The prognosis for type 2 DM patients is worse than for the non-DM group, and the associated CV morbidity seems to be the most important predictor in our analysis.
For many years, DM has been the most common cause for entering dialysis in the United States8 and since 2007, the same is true in Spain.2 The progression of DM and its complications are associated with a number of abnormalities and a higher mortality rate, primarily due to CV causes, whether they undergo PD or HD.9 Therefore, it is not easy to recommend a particular modality of treatment since the prognosis does not seem to be better with HD. Most studies find that patients on PD have a mortality rate that is lower than or similar to mortality for those on HD during the first two years,5,10-12 with an increase in mortality after the second year,3-5 particularly for patients older than 65. Studies carried out in our country conclude that the dialysis technique chosen has no prognostic value when we correct for selection criteria and comorbidity.13 Furthermore, patients with CV disease seem to have a lower survival rate on PD than on HD.14-16 When sub-analyses are carried out for diabetic patients, some studies show better outcomes for PD1 and others for HD.1,17
Demographic characteristics in the Spanish population are comparable to those of European and Canadian studies than to studies from the United States. In fact, Registry datas how the prevalence of DM in U.S. to be as high as 45%, which makes it difficult to extrapolate their annual results to other cohorts.5 Unfortunately, the Spanish Registry of renal patients has no available data for detailed analyses of aspects such as comorbidity, achieving the recommended targets hospitalisation, etc. For these reasons, it is important to have studies like the one we are presenting, and they should be updated periodically as a reference for a particular period and geographical area.18,19
The hospitalisation rate in our study is somewhat lower than that cited recently in U.S. studies,17 and this may be because it only includes incident patients and because of a lower comorbidity. A Canadian study indicates that the hospitalisation rate increases with age and is higher for women and those with DM.20 In a previous analysis of our entire cohort, higher comorbidity (estimated by the CCI or prevalence of CV events) and lower baseline haemoglobin (Hb) was associated with a higher hospitalisation rate,7 which is similar to that for patients undergoing HD.21 The relevance of Hb as a risk marker is due to it being the only modifiable marker.
In the previously published report of the entire cohort, mortality was associated with higher comorbidity at the beginning of the treatment, whether using the CCI or the prevalence of DM or previous CV events as the variable.7 Although conflicting results do exist,20 most studies report that age and diabetes are independently associated with greater mortality.5,12,22-26 However, type 1 and 2 DM patients cannot be analysed as a single group, since their epidemiology and clinical presentation are completely different. We therefore decided to analyse the data from type 2 DM patients separately.
We did not use the Charlson comorbidity index in the current study because it is calculated using DM as a factor (the principal variable in this study). If we were to eliminate DM from the Charlson index, it would lose its validity. When we attempt to see which patient management factors make the difference between type 2 DM patients and non-diabetics, we find that the type 2 DM group has poorer pressure control, similar Hb levels and better PD efficiency at the expense of a higher initial RRF. Regarding the compliance with the guidelines recommendations, type 2 DM patients have poorer control of blood pressure, particularly systolic BP, and a non-significant tendency to have better control over anaemia and better PD efficiency. None of these factors, whether they are continuous or categorical variables (achieving objectives), proved to have prognostic influence in our study. All previous publications showed inconsistent results.27-30
We must recognise that the CCI has significant limitations. Among them, we can highlight the lack of a measure of severity of the illness, the fact that it was designed for the general population, and the time elapsed since it was created, in which drastic changes have occurred in the prognostic value of some illnesses such as AIDS. For these reasons, some authors have proposed adapting the comorbidity index to a patient on PD through a modification in its scoring,6 or by using specific comorbidity markers with a measure of severity.31 However, the Charlson comorbidity index is still the most widely used, and it allows us to establish comparisons with other studies on patients whether inside or outside of the field of dialysis. Clinical studies, such as this by our group, have yet to meet the challenge of designing a prognostic indicator that will be sensitive and specific enough for PD patients.
The important difference between non-DM patients and type 2 DM patients is the extent of CV damage before the start of PD. For this reason, when adjusting multivariate analyses, we observe that it is not possible to keep type 2 DM and the CV event in the same model. This is due to the association between the two being very pronounced; the prevalence of prior CV events is more than three times higher in type 2 DM patients than in non-diabetics. Baseline CV comorbidity is, therefore, the main factor determining survival for type 2 DM patients on PD.
It seems that this study¿s conclusions are what would be expected, but it is important to have current, well-founded data to corroborate and establish the importance of each of the risk factors.
The main limitation of this study is the number of cumulative deaths. A longer follow-up would enable us to register more events, although the average time undergoing PD treatment does not exceed two years according to other records with a longer follow-up time.18 Other factors that influence mortality, such as the patient¿s nutritional or inflammatory state, could not be evaluated due to the heterogeneity of data collected in different centres. However, we consider this study to be relevant due to its careful design and follow-up and its large sample size (for a PD study). In fact, most of the PD units in Spain have a low number of patients,18 which is why it is necessary to launch multi-centre initiatives in order to obtain sufficient statistical power.
To sum up, our data seems to confirm that type 2 DM patients have worse outcomes than non-diabetic patients. This is fundamentally due to higher comorbidity, and particularly to a higher prevalence of CV events prior to starting dialysis. Patients with type 2 diabetes start dialysis with a higher RRF, better total adequacy and good correction of anaemia and blood pressure over the course of the followup. All of these factors, which should improve patients¿ prognosis, cannot compensate for the weight of the CV comorbidity that developed before dialysis, and before the onset of DM itself.
We need more studies on the progress of these patients who undergo different modalities of renal replacement therapy in order to improve their prognosis.
Table 1. Characteristics of type 2 DM patients compared with non-diabetics. Shown as mean (standard deviation, SD) or as a percentage. Student's t-test,
Chi-square test or incidence rate ratio is used depending on the nature of the variables.
Figure 1.
Table 2. Achievement of recommended targets for HT, anaemia and PD adequacy by type 2 DM patients
compared with non-diabetics shown as percentages. Chi-square test applied depending on the nature of the
variables.