Acquired copper deficiency is a rare disorder that has been described as being associated with gastric bypass surgery, gastrectomy, excessive zinc intake or administration of total parenteral nutrition without adequate copper contributions.1,2
Copper deficit causes different haematological and neurological alterations, such as pancytopenia, myelopathy and peripheral neuropathy, as well as skeletal alterations such as osteoporosis.2 Although it is rare, its incidence has increased as a result of the increase in bariatric surgery, since the absorption of copper is carried out in the stomach and the proximal duodenum.3
We present the case of a patient under treatment with chronic haemodialysis, who presented severe pancytopenia associated with copper deficiency secondary to a malabsorption syndrome due to gastric bypass surgery.
The patient is a 61-year-old man with chronic kidney disease secondary to diabetic nephropathy and hyperfiltration, on chronic haemodialysis since September 2016. In October 2015, he underwent gastric bypass surgery, subsequently developing short bowel syndrome with malabsorption.
Laboratory tests at the start of haemodialysis showed: normocytic/normochromic anaemia (Hb 10.6g/dl, Ht 33.5%, MCV 96.4, MCH 30.4), thrombocytopaenia (platelets 107,000), normal white blood cells (5,170, normal formula), transferrin 104mg/dl (normal 200–360), ferritin 397ng/ml (normal 20–300), iron 27μg/dl (normal 65–175) and transferrin saturation 18%. Levels of vitamin B12 and folic acid were normal.
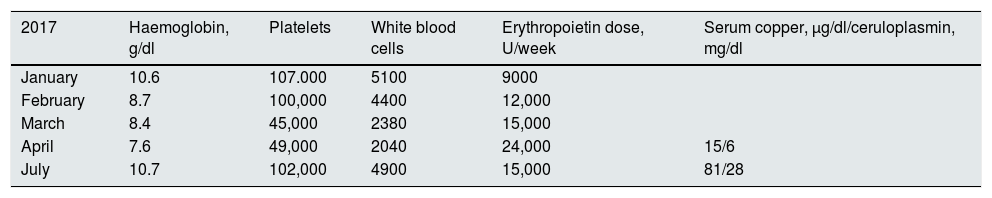
Treatment was started with intravenous iron 200mg/month and erythropoietin 9000U/week. Progressive anaemia has been observed since February 2017, despite a progressive increase in the weekly dose of erythropoietin, as well as increased thrombocytopaenia and leukopenia (Table 1). The reticulocyte count and blood smear were normal. Given the suspicion that pancytopenia was secondary to a copper deficit due to his history of gastric bypass, serum copper was tested, and showed low levels of 15μg/dl (normal 75–150), in addition to ceruloplasmin, which was 6mg/dl (normal 20–60). Serum zinc was normal: 84μg/dl (60–150).
Evolution of haemoglobin, platelets, white blood cells and the weekly dose of erythropoietin.
| 2017 | Haemoglobin, g/dl | Platelets | White blood cells | Erythropoietin dose, U/week | Serum copper, μg/dl/ceruloplasmin, mg/dl |
|---|---|---|---|---|---|
| January | 10.6 | 107.000 | 5100 | 9000 | |
| February | 8.7 | 100,000 | 4400 | 12,000 | |
| March | 8.4 | 45,000 | 2380 | 15,000 | |
| April | 7.6 | 49,000 | 2040 | 24,000 | 15/6 |
| July | 10.7 | 102,000 | 4900 | 15,000 | 81/28 |
We started treatment with oral copper supplements (copper sulphate, 2mg+copper carbonate, 1mg), observing progressive improvement in haematological alterations, as well as normalisation of copper and ceruloplasmin levels after 3 months of treatment. However, given the persistence of the malabsorption syndrome, it was decided to reverse the gastric bypass in September 2017.
Hypocupraemia is a rare finding in haemodialysis patients, and in most cases, normal or elevated levels have been described in the general population.4 The case presented here developed severe pancytopenia secondary to copper deficit, as a consequence of gastric bypass surgery, with no neurological alterations, since these are usually preceded by haematological alterations.5 The recovery of the haematological symptoms was fast and practically complete after copper supplementation. However, recovery is usually incomplete in cases of neurological involvement.
Considering that the incidence of copper deficit has increased as a result of the increase in gastric bypass surgery, and given that the neurological alterations may be irreversible, we recommend the determination of serum copper in these patients, mainly if they present haematological alterations that point to this nutritional deficit.
Please cite this article as: López Melero E, Ruíz-Roso G, Botella I, Ortego Pérez S, Delgado M, Fernández Lucas M. Pancitopenia secundaria a déficit de cobre en un paciente en hemodiálisis. Nefrología. 2019;39:451–452.