Patients with renal disease on renal replacement therapy with hemodialysis require anticoagulation of the extracorporeal system and heparin is the most common.
Heparin-induced thrombocytopenia (HIT), a serious condition, occurs in patients exposed to heparin, regardless of the dose and route of administration, with a reported prevalence of around 5%.1,2
This condition is due to the development of autoantibodies against endogenous platelet factor 4 (PF4), which causes platelet activation, which in turn causes arterial and venous thrombosis in some severe cases.3
There are 2 types of HIT: type I, without significant decrease in platelet count or thrombosis; and type II, where there is thrombocytopenia with thrombosis, requiring the suspension of heparin and the use of another anticoagulant to treat thrombosis.
The presentation of HIT in hemodialysis patients motivates the search for alternatives for anticoagulation, such as the use of predilution hemodiafiltration (HDF), continuous infusion of saline solution, use of citrate as an anticoagulant and even a change of modality to peritoneal dialysis.
The prevalence of HIT in hemodialysis patients may be up to 4%, although the presence of PF4 antibodies is higher in dialysis patients.4–6
The use of citrate as an anticoagulant is common practice in continuous renal replacement therapy and requires the use of calcium replacement.7 There are isolated reports of the use of citrate without calcium replacement in extended dialysis in patients with acute kidney failure.8
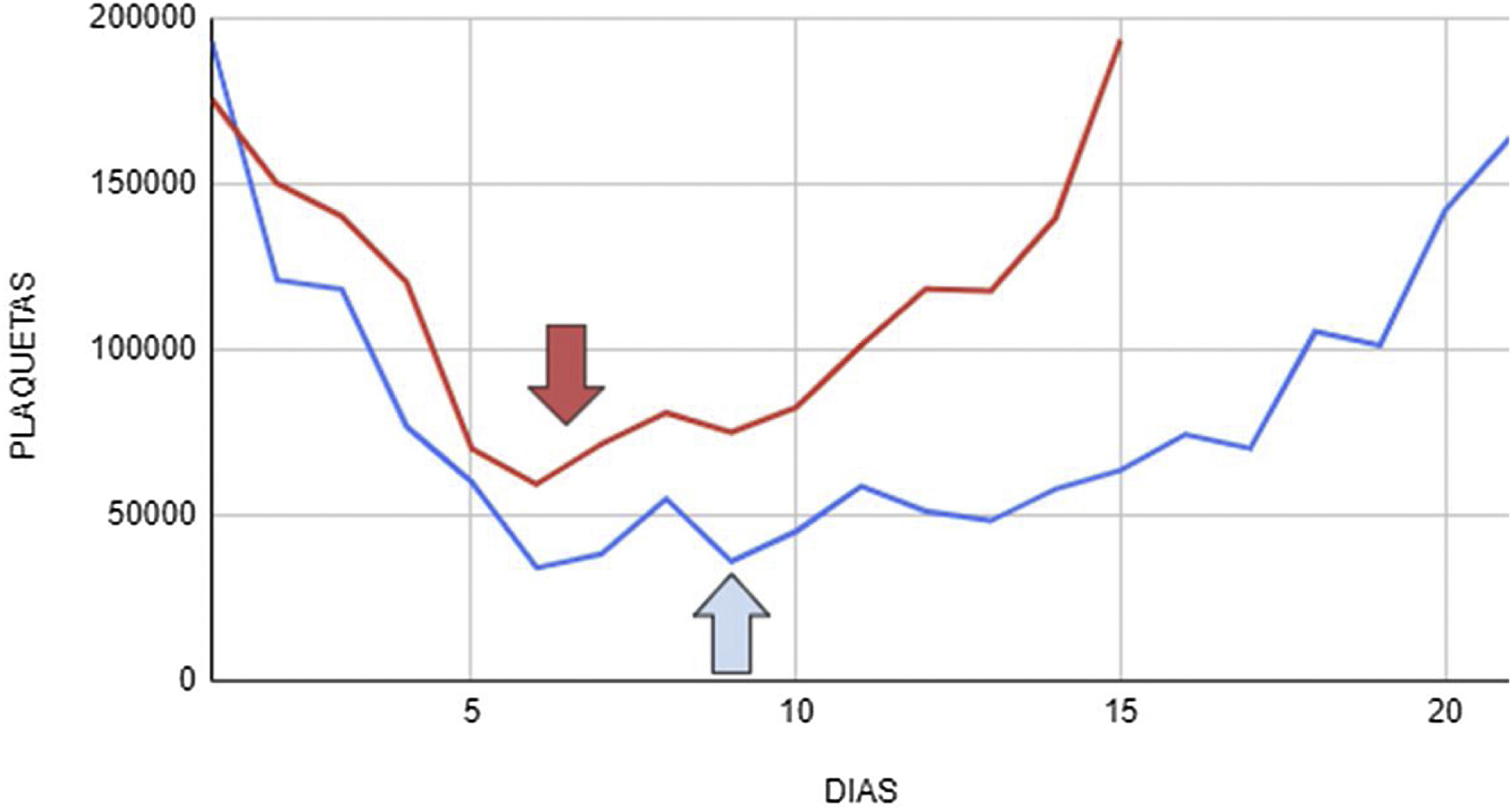
Online HDF is an increasingly common hemodialysis modality in patients with chronic kidney disease (CKD). We present two clinical cases of patients with CKD on chronic hemodialysis with a history of HIT, with the use of citrate as anticoagulant implemented during online HDF without calcium replacement.Case A A 68-year-old male patient with a diagnosis of ANCA-p positive pauci-immune glomerulonephritis. With the progressive use of sodium heparin during dialysis sessions his platelet count decreased (Fig. 1) with positive anti-PF4, so we discontinued heparin, starting citrate as an anticoagulant to maintain chronic hemodialysis. An 81-year-old female patient with a diagnosis of immune-mediated extra-capillary glomerulonephritis. With the progressive use of sodium heparin during dialysis sessions her platelet count progressively dropped (Fig. 1), with positive anti-PF4 and thrombosis of the right internal jugular vein, so we diagnosed HIT, discontinued heparin and started citrate as an anticoagulant.
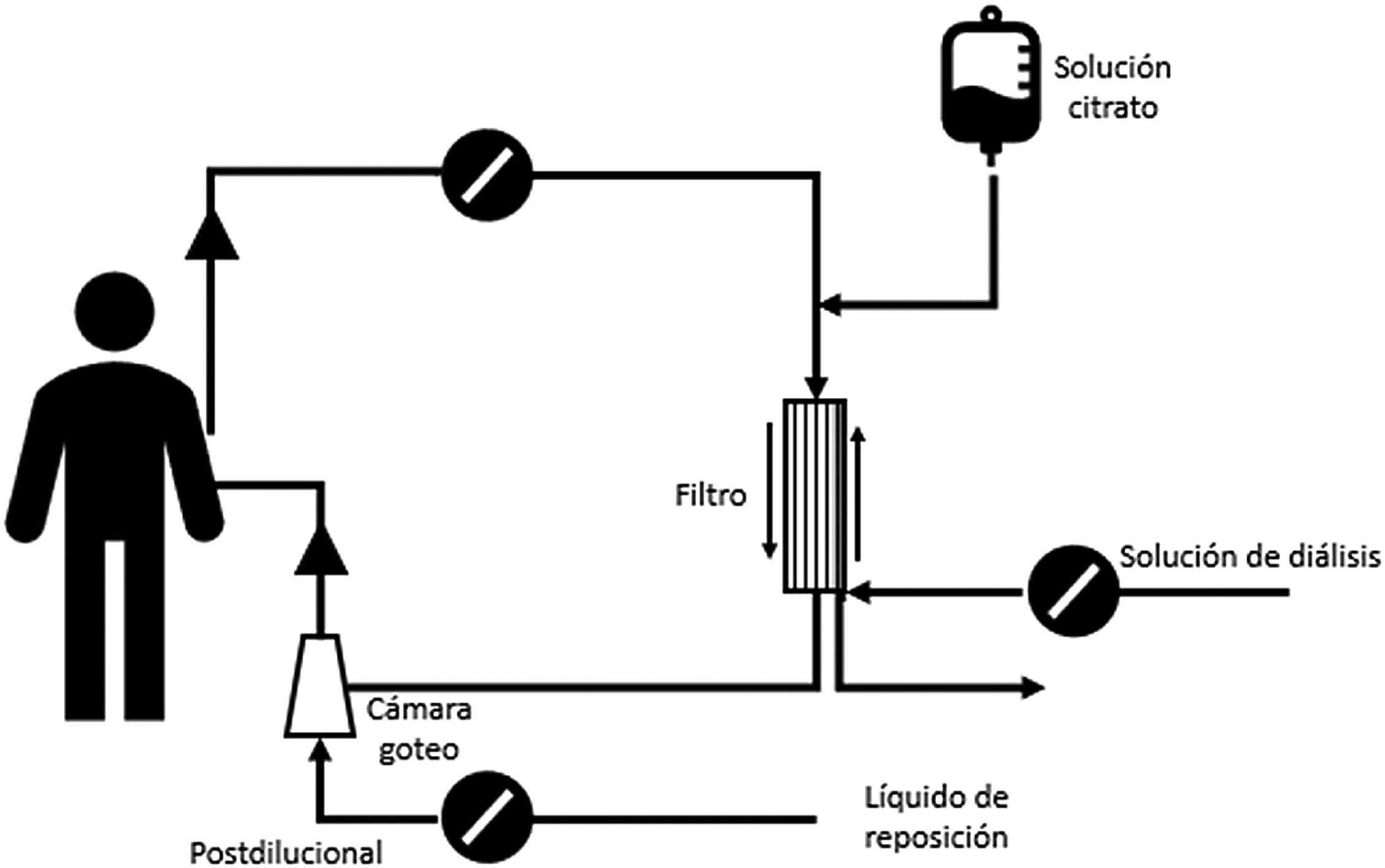
The two patients performed post-dilutional online HDF, during 255 min, with Fresenius 5008 equipment, with Qb 350−400 mL/min Qd 500 mL/min, bath with calcium 3.5 mEq/L, sodium 138 mEq/L, potassium 2 mEq/L, bicarbonate 32 mEq/L, chlorine 109.5 mEq/L with high efficiency helixone FX 600–800 filters. The target replacement rate was between 20 and 24 L at each session. No calcium replacement was used in the venous branch, only calcium levels were monitored during the sessions. The citrate solution used was Soluflex® 679S ACD (citric acid 0.8% sodium citrate 2.2%) at a citrate infusion rate varying between 200−300 mL/h connected to the circuit in the pre-filter arterial branch (Fig. 2). The technique included calcium measurement prior to dialysis, at 2 h and at the end of the dialysis session to avoid hypocalcemia during the first sessions. Patients and dialysis nurses were instructed in the detection of symptoms compatible with hypocalcemia.
Post-dilution replacement with a calcium-rich bath made it possible to maintain renal replacement therapy without producing thrombocytopenia or thrombotic episodes in patients diagnosed with HIT, avoiding coagulation of the extracorporeal system and episodes of hypocalcemia, without the need for calcium replacement as usually required by continuous renal replacement therapies.
We believe HIT is underdiagnosed in many dialysis clinics, although type II is a serious entity that implies a change in the prescription of anticoagulation during dialysis sessions.
Our experience demonstrates that the use of online HDF and a calcium-rich bath with post-dilutional replacement using citrate anticoagulation without calcium replacement is a simple and safe alternative in patients with contraindications to the use of heparin resulting in no coagulation of the extracorporeal system.