Chronic kidney disease (CKD), cancer and hematological diseases share areas of reciprocal influence. Cancer can affect the kidney either as glomerular lesions or as a result of the toxic effects of medication or radiation with acute (thrombotic microangiopathy, acute kidney injury, interstitial nephropathies among others) or chronic processes (worsening of CKD after nephrectomy due to renal cancer, interstitial fibrosis, hydroelectrolytic disorders).
On the other hand, patients who require renal replacement therapy with dialysis and particularly with kidney transplantation are at high risk of onset of cancer due to the immunosuppression situation that they generate.
In addition to conventional chemotherapy, innovative treatments have been developed: target agents against growth factors and their receptor; anti-angiogenic drugs; immunoregulatory proteins; cell cycle regulators; and enzyme inhibitors. Other immunotherapeutic approaches have also been developed, such as vaccines, adoptive cell therapy (CAR T cells) or development of antibodies. All these therapeutic advances will improve the outcomes against cancer and hematological diseases, but they are not free from secondary renal problems.
Onco-Nephrology is already an important area for the Spanish Society of Nephrology with a large number of inter-consultations. Nephrologists need a better understanding of rapidly evolving areas of cancer biology and its treatment in order to become valued members of the cancer care team and to provide the best nephrology care possible.
La enfermedad renal crónica (ERC), el cáncer y las enfermedades hematológicas comparten áreas de influencia recíproca. El cáncer puede afectar al riñón bien como lesiones glomerulares o como consecuencia de los efectos tóxicos de la medicación o radiación, con procesos agudos (microangiopatía trombótica, insuficiencia renal aguda, nefropatías intersticiales, entre otros) o crónicos (empeoramiento de la ERC tras la nefrectomía por cáncer renal, fibrosis intersticial, trastornos hidroelectrolíticos).
En sentido opuesto, los pacientes que precisan tratamiento renal sustitutivo con diálisis y particularmente con trasplante renal son de alto riesgo para la aparición de cáncer debido a la situación de inmunosupresión que generan.
Además de la quimioterapia convencional, se han desarrollado tratamientos innovadores: agentes diana contra factores de crecimiento y su receptor, fármacos antiangiogénicos, proteínas inmunorreguladoras, reguladoras del ciclo celular o bloqueantes enzimáticos. También otros enfoques inmunoterapéuticos, como vacunas, terapia celular adoptiva (células CAR T) o desarrollo de anticuerpos. Todas estas novedades terapéuticas mejorarán los resultados frente al cáncer y enfermedades hematológicas pero no están exentas de problemas secundarios con afectación renal.
La Onco-Nefrología es ya un área importante para la Sociedad Española de Nefrología, con gran número de interconsultas. El especialista en Nefrología precisa una mejor comprensión de áreas de tan rápida evolución de la biología del cáncer y su tratamiento, para convertirse en miembro valioso del equipo de atención del cáncer y proporcionar la mejor atención nefrológica posible.
Cancer is the second cause of death and morbidity in Europe (3.7 million new cases per year). The median age of patients at the time of Cancer diagnosis is 65 years. From the 47% of cancer survivors, half of then are older than 70 years.1 In a aging population it is expected to have an increase in the number of patients whose cancer is complicated by acute or chronic kidney diseases (CKD).
The EPIRCE study2 done in Spain by the SEN, observed that 23% of patients older than 65 years had CKD stages 3–5. Therefore in the aging population coincide cancer and CKD that explains the large amount of consultations between Oncology and Nephrology. This justifies the generation of this working group.
The cancer-kidney connectionThe is an interrelationship between CKD and cancer. Cancer may affect the kidney through the so-called paraneoplastic nephropathies, mainly as glomerular lesions,3 or through the toxic effects of the medication or radiation,4,5 or even after reduction of renal mass post nephrectomy due to renal cancer.6 In addition, patients on dialysis7 and particularly transplanted8 are at a high risk for the onset of cancer due to the status of immunosuppression.
Clinical consultations from oncology to nephrologyIn oncology patients there are a large number of reasons that explains the increasing number to nephrology consultations.
- –
Acute Renal Failure of several causes: nephrotoxicity induced by chemotherapy (tubular necrosis, thrombotic microangiopathy, acute interstitial nephropathy), hemodynamic factors (sepsis), obstructive processes, etc.
- –
Nephrotic range proteinuria cased by certain cancers (Hodgkin's disease, leukemia, Multiple Myeloma, Colon cancer, lung, etc.) associated to minimal glomerular lesions, segmental and focal hyalinosis or membranous nephropathy. The glomerular disease associated with cancer could be summarize as follows9:
- 1.
Treatment of Cancer may result in the resolution glomerular process.
- 2.
Membranous nephropathy has been classically associated with solid tumors.
- 3.
Minimal change disease has been commonly described in hematological malignancies, especially Hodgkin lymphoma.
- 4.
Membranoproliferative glomerulonephritis is increasingly recognized as a pathology associated to chronic hematological malignancies such as Chronic lymphocytic leukemia.
- –
Injuries related to chemotherapy with different drugs: Interferon, Lenalidomide, Pamidronate, Anthracyclines, mTOR inhibitors or renal manifestations associated to with new therapies whose effect at the renal level is not well characterized yet such as antiEGFR, anti VEGF, anti PD1 and PDL1 or CAR T Cells, etc. that will be commented further in this manuscript.
- –
Water and electrolyte disorders such as: hyponatremia, hypercalcemia, hypokalemia, hypomagnesemia, hypophosphatemia, acid-base abnormalities, disorders of the calcium and mineral metabolism.
- –
Problems related to doses and timing of chemotherapy in patients with end stage renal disease on dialysis.
- –
Consensus on the protocols for inclusion in the transplant waiting list, and times latency in potentially resolved pathologies; both for the recipient and donor.
There should be special interest in cancer patients with contrast-induced renal damage.10 These patients are frequently exposed to examinations that require the use of iodized contrasts to control the disease progression. With repeated procedures the cumulative dose of iodinated contrast increases the risk of kidney injury reducing the survival.11 A work published by Hong demonstrated an association between the need to perform a CT scan with contrast and acute renal injury secondary to this procedure.12 In fact, the KDIGO guidelines recommend to delay new exposures to contrast in cancer patients with kidney injury.13
There is an area not yet sufficiently explored in relation with the Renal Functional Reserve (RFR) that may be altered after repeated kidney aggressions induced by contrast infusions without evidence of deterioration of renal function. Certainly, in the absence of elevation of the serum creatinine it cannot be ruled out subclinical acute structural kidney injury with kidney damage.14 Similarly to the measurement of cardiac troponin as a valid marker of in acute myocardial infarction without ST elevation, it is necessary to have precise markers of structural renal damage in cases of acute renal injury without elevation of serum creatinine. Among these biomarkers or “renal troponins” it should be noted the cell cycle markers, as the urinary tissue inhibitor of metalloproteinase 2 (TIMP-2) and protein 7 bound to insulin-like growth factor (IGFBP-7) that are commercialised together in Spain.
Therefore the nephrologist should evaluate both functional and structural kidney damage more precisely in a cancer patient subjected to toxicity of medications and repeated explorations with iodinated contrast. The idea is to prevent long term kidney deterioration.
Cancer and CKD as reciprocal risk factorsThe Societies of Nephrology, Oncology and Hematology must advance together in the study of associations between CKD and cancer as reciprocal risk factors. These questions could be answered by the analysis of existing databases in different countries.
The Belgian study BIRMA, showed an estimated glomerular filtration rate (eGFR) by MDRD less than 60ml/min/1.73m2 in 18% of cancer patients.15 In other series from different countries, the data is similar. In United States it was found chronic renal dysfunction in 22% of in cancer patients,16 25% in Japan17 and 15.5% in Austria.18 One of the few studies generated in Spain, revealed that in 594 patients hospitalized in Oncology a 18.2% presented an eGFR by MDRD<60ml/min/1.73m2.19 In any case, it is clear that epidemiological studies with a large number of patients are needed to know the true prevalence CKD in cancer patients. It is also necessary to know if CKD is a risk factor for cancer. In a meta-analysis of 32,057 participants there was no association between CKD and the risk of cancer, however there was evidence of increased incidence of certain types of cancer in dialysis patients, such as the urinary tract, endocrine and gastrointestinal.20 The prevalence of cancer in transplant patients is high21; data from the SEN Registry reveal that the mortality caused by cancer in the kidney transplant patient is 20% and a consensus document on its prevention has been developed.22 Currently, the age of patients undergoing kidney transplant is increasing progressively and cancer constitutes one of the most important complications, both in patients who are kidney transplant candidates as in patients who have already received it. In fact, the ANZDATA registry data (Australia and New Zealand) show, as in Spain, that cancer has become a cause of mortality as frequent as that of cardiovascular origin in the kidney transplant population.23
Incidence of CKD after nephrectomy due to kidney cancerDialysis facilities frequently receive patients who have undergone nephrectomy due to kidney cancer. Kim et al.24 showed that up to 22% of patients with renal tumors had eGFR<60mL/min per 1.73m2 before nephrectomy. The two surgical options radical nephrectomy or partial nephrectomy (“nephron-sparing surgery”) do not differ in terms of oncological evolution but it makes a difference in terms of postoperative incidence of CKD and cardiovascular complications.25 That is why the American and European Urology societies support partial nephrectomy as a new standard of treatment for tumors restricted to the organ≤4cm (T1a) and suggested that it be considered an option for patients with tumors>4 but ≤7cm (T1b).26,27
According to the SEN it is very important to analyze the epidemiology and evolution of nephrectomized patients (or simply starting dialysis with an active tumor) mainly in relation with the initiation of renal replacement therapy, anntineoplastic treatments, tolerance and survival.
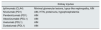
Therapeutic resources against cancer: target agents and immunotherapyTreatment of cancer evolves quickly. For the Nephrology specialist it is difficult to be updated on indications and side effects. Conventional chemotherapy (cisplatin, metrotexate, melphalan, cyclophosphamide, etc.) may produce renal injury mainly acute tubular necrosis and thrombotic microangiopathy, among others (Table 1).
Conventional chemotherapy.
| Kidney injuries | |
|---|---|
| Platinum (cis, carbo, oxali) | ATNg, TMA, chronic interstitial fibrosis, salt lossing nephropathy, Fanconi syndrome, hypomagnesemia |
| Ifosfamide | ATNag, nephrogenic diabetes insipidus |
| Methotrexate | Crystal induced Nephropathy |
| Pemetrexed | ATNg, TMA, AIN, tubular atrophy, interstitial fibrosis |
| Gemcitabine | TMA |
| Mitomycin | TMA |
| Melphalan | AKI, hyponatremia |
| Cyclophosphamide | Hemorrhagic cystitis, hyponatremia |
| Anthracyclines | Collapsing glomerulopathy, TMA, focal hyalinosis, minimal change GN |
TMA: thrombotic microangiopathy; AIN: acute interstitial nephritis; ATN
But there are other more recent therapeutic approaches directed to a specific target (Targeted Therapy). Such treatment is directed at the molecules that are essential for the survival of cancer cells. Molecular therapy has the advantage of the selectivity of the therapeutic target, which is different from chemotherapy and radiotherapy, because does not affect the surrounding healthy tissue, thus reducing significantly the side effects.
For the most part, all patients with the same type of cancer are not necessarily treated with the same medications or procedures. The therapy based on molecular targeting creates a personalized system of therapy in which patients are treated based on the unique molecular structure of its specific cancer. Using fundamental tissue stains, doctors can see which are the target molecules present in the patient's cancer and determine which drugs should be administered.
Target agentsTarget agents against EGFR (epidermal grow factor receptor inhibitors)Activation of the ErbB family (including EGFR or HER1, HER2, HER3 and HER4) increases tumor growth and progression, stimulates proliferation, angiogenesis, invasion, metastasis and inhibition of apoptosis. The most clinically advanced approach to EGFR inhibition includes the use of monoclonal antibodies (mAB) directed against the extracellular domain of EGFR (cetuximab, panitumumab) or HER2 (trastuzumab) and the use of targeted tyrosine kinase inhibitors [TKI]) against the intracellular domain of tyrosine kinase (gefitinib, erlotinib, lapatinib, canertinib).28 The binding of EGFR to its receptor activates the renal magnesium channel in the distal conboluted tubule, stimulating magnesium transport so that these anti-EGFR compounds are associated with hypomagnesemia and, as a consequence, secondary hydroelectrolytic disorders, such as hypocalcemia and hypokalemia (Table 2).
Target agents against VEGF-VEGFr antiangiogenic drugsAngiogenesis, the formation of new blood vessels from pre-existing ones, plays a central role in tumor growth and metastasis. Endothelial proliferation and the formation of new blood vessels increase the size of solid tumors. Blockade of angiogenesis should be an effective therapeutic approach against many types of tumors. The key signaling system that regulates the proliferation and migration of endothelial cells is VEGF and its receptors (VEGFr-1, 2 and 3).
Bevacizumab is an angiogenesis inhibitor, which targets vascular endothelial growth factor. Also there are several TKI, such as sunitinib, sorafenib, pazopanib and axitinib. The use of these targeted therapies may induce both glomerular damage (mild to severe proteinuria, thrombotic microangiopathy, etc.) and tubular injury (acute renal failure) because VEGF and others are also expressed in the normal nephron while maintaining the filtration barrier and glomerular endothelial integrity29 (Table 3).
VEGF-VEGFr inhibitors.
| Kidney injuries | |
|---|---|
| Bevacizumab | HTN, proteinuria, TMA |
| Aflibercept | HTN, proteinuria, TMA |
| Axitinib | HTN, proteinuria, TMA |
| Sunitinib | HTN, proteinuria, TMA |
| Sorafenib | HTN, proteinuria, TMA |
| Pazopanib | HTN, proteinuria, TMA T |
| Vandetanib | HTN, proteinuria, AKI, Renal lithiasis, water and electrolyte abnormalities |
Creatinine elevation is observed in sunitinib (46–70%), sorafenib (41%), pazopanib (32%) and axitinib (55%).
TMA: thrombotic microangiopathy; ARF: acute renal failure.
This is a protein that helps control several cellular functions, including the regulation of cell growth, proliferation and death. Since the activity of this protein is increased in some types of cancer, it is considered as a therapeutic target and several drugs have been designed to inactivate its function, including temsirolimus, which is used in the treatment of renal carcinoma. Everolimus and sirolimus are well known in Nephrology for their use to prevent rejection in renal transplantation for their ability to reduce the immune response30 (Table 4).
Agents against PD-1 and PD-L1 and CTLA-4 (checkpoint inhibitors)T lymphocyte receptors recognize surface antigens that identify a cell as cancerous; as a result they became activated with the purpose of eliminating such a cell. But activated T cell requires a stop signal to ensure that over activation will not occur. One mechanism by which T lymphocytes activation is regulated is by inhibition of receptors such as the programmed death receptor (PD-1) and the cytotoxic T-lymphocyte-associated antigen (CTLA-4), which are present on the surface of T cells. After activation, T lymphocytes increase the expression of the PD-1 and CTLA-4 receptor, allowing them to receive the deactivation signal. This signal will occur after the binding of this receptor to its PD-L1 or PD-L2 ligand, or B7-1/B72 that are normally expressed on the surface of dendritic cells and macrophages, causing a reduction of cytokine production and suppression of T cell proliferation.
This is the mechanism that have incorporated multitude of tumors to block its recognition. Cancer cells surface express the PD-L1 and PD-L2 or B7 ligand proteins, thus escaping the action of the immune system and continue to proliferate. The PD-1/PD-L1 and CTLA-4 pathway therefore represents an adaptive immune resistance mechanism developed by tumor cells in response to endogenous antitumor activity.31
Explained in a simple way, the T lymphocyte has the PD1 receptor and the tumor has the PDL1 ligand. So when the T lymphocyte is going to attack the tumor and the ligand binds the receptor, there is an inhibition of lymphocyte activity so the lymphocyte cannot destroy the tumor. Basically, this interaction between PD1 of the lymphocyte and PDL1 of the tumor causes the tumor to be protected and that the lymphocyte cannot attack the tumor cell. The “checkpoint” inhibitors block the lymphocyte receptor or block the tumor ligand, so that both cannot find each other, and if they are not found the lymphocyte will extinguish the tumor. That is why inhibition of this interaction is so important. Advances in technology have made possible to have now more than 7 antibodies from different pharmaceutical companies that inhibit the PD1 of the lymphocyte or inhibit the PDL1 of the tumor so lymphocytes can destroy the tumor with cancer regression.
The use of inhibition of the immune checkpoint pathways has led to the approval of several new drugs: ipilimumab (anti-CTLA-4), pembrolizumab (anti-PD-1) and nivolumab (anti-PD-1)31 (Table 5).
Agents against PD-1 and PD-L1 and CTLA-4 (checkpoint inhibitors).
| Kidney injuries | |
|---|---|
| Ipilimumab (CLA4) | Minimal glomerular lesions, lupus-like nephropathy, AIN |
| Nivolumab (PD1) | AIN, HTN, proteinuria, hypophosphatemia |
| Pembrolizumab (PD1) | AIN |
| Atezolizumabb (PDL1) | AIN |
| Avelumab (PDL1) | AIN |
| Durbalumab (PDL1) | AIN |
HTN: hypertension; AIN: acute interstitial nephritis.
BRAF is a protooncogene that belongs to the raf/mil family of serine/threonine protein kinase. It is the most common gene associated with mutations in malignant melanoma observed in 40–50% of patients. The resulting activation of mitogen-activated protein kinase leads to oncogenesis through stimulation of cell growth and inhibition of apoptosis. Clinical trials have demonstrated a median progression-free survival of approximately 12 months with the combination of a targeted BRAF inhibitor with a MEK inhibitor.
Currently, for the treatment of BRAF-mutated melanoma the FDA has approved32 BRAF inhibitors: vemurafenib, dabrafenib; and,
MEK inhibitors: trametinib, cobimetinib (Table 6).
Target treatments.
| Kidney injuries | ||
|---|---|---|
| HER2 inhibitor | Trastuzumab | HTN |
| BRAF inhibitor | Vemurafamib | ATN, proteinuria, FSH. |
| Fanconi S, hyponatremia, hypokalemia | ||
| Dabrafenib | AIN (granulomatous), ARF | |
| Hypophosphatemia | ||
| MEK inhibitor | Trametinib | ARF, HTN, hyponatremia |
| HGFR inhibitor | Crizotinib | ARF, hypophosphatemia; Rc |
| Proteasome inhibitor | Bortezomib | TMA |
| Carfilzomib | TMA, ATN, tumor lysis syndrome | |
| Titrosine kinase inhibitor | Imatinib | ARF, hypophosphatemia. |
| Anti-IL-6 | Siltuximab | Hyperkalemia, hyperuricemia |
HGFR: hepatocyte growth factor receptor; FSH: segmental and focal hyalinosis; HTN: arterial hypertension; ARF: acute renal failure; TMA: thrombotic microangiopathy; AIN: acute interstitial nephritis; ATN: acute tubular necrosis; RC: renal cysts.
This is a substance that blocks the enzyme PARP. PARP helps to repair DNA when damaged. DNA damage can be caused by many reasons, including exposure to ultraviolet light, radiation, certain anti-cancer medications or other substances in the environment. Blocking PARP may prevent cancer cells from repairing their damaged DNA, causing their death. PARP inhibitors, a type of targeted therapy, appear to improve progression-free survival in women with recurrent platinum-sensitive ovarian cancer, as evidenced primarily by the addition of olaparib to conventional treatment. Other drugs in this group are iniparib, rucaparib, veliparib, etc. In addition to its use in cancer therapy, PARP inhibitors are considered a potential treatment for life-threatening acute diseases, such as stroke and myocardial infarction, as well as for long-term neurodegenerative diseases.33
Cyclin inhibiting agentsCells that enter and progress throughout the cell cycle. The cell cycle is controlled by variations in the levels and degree of activity of the cyclines. Cyclines perform their functions forming complexes with structural proteins called cyclin dependent kinases (CDK).
Cyclin B/CDK1 controls the passage from phase G2 to phase M2. When the cell enters the G2 phase, cyclin B is synthesized and binds to CDK1, forming the cyclin B/CDKI complex, whose activity is indispensable for cells to move to phase M. This complex is activated by phosphorylation and the active kinase phosphorylates several proteins involved in mitosis and DNA replication.
Cyclin inhibitors are a new hormonal therapeutic route against breast cancer HR+/HER2−, metastatic or locally advanced, which reduces the progression of the disease by inhibiting the cell cycle, through inhibition of cyclin-dependent kinases, that is, the activation or control of cell proliferation. Ribociclib, abemaciclib and palbociclib are directed to cyclines 4 and 6 (CDK4/6).34
ImmunotherapyIt is one of the most important innovations in the history of medicine. Immunotherapy, also called biological therapy, is a type of cancer treatment that stimulates the body's natural defenses to fight cancer. It uses substances produced by the body or manufactured in a laboratory to improve or restore the function of the immune system. There are different types of immunotherapy:a. Improving the immune system and making it stronger.
a1 Vaccine: by identifying mutated proteins of the tumor, small neoantigens are created that are injected intravenously to activate T cells against specific tumor antigens.
a2 Adoptive cell therapy. CAR T cell: T cells samples from the patient are grown in the laboratory. This procedure increases the number of T cells capable of destroying cancer cells or fighting infections. These T cells are returned to the patient to help the immune system to fight the tumor. One form of adoptive cell therapy is T-cell therapy and CAR (CAR T cells). This therapy requires a separation of T cells from the patient's blood sample. Thereafter, using an unarmed virus, T cells are genetically modified to produce receptors on their surfaces called chimeric antigen receptors. These synthetic receptors allow T cells to recognize and bind to a specific protein, in this case, a tumor antigen. These designed T cells expand by hundreds of millions in a cell manufacturing facility. Finally, CAR T cells are infused into the patient (preceded by a lymphodepletion chemotherapy regime). These CAR T cells can selectively attack and kill cells that express the tumor antigen. This treatment is not exempt of serious side effects, such as syndrome of cytokine release or tumor lysis syndrome,35 A T-cell and CAR therapy was approved in August 2017 for the treatment of children with acute lymphoblastic leukemia. A second therapy will be approved soon for adults with advanced lymphomas.
a3 Stimulating factors: A third technique of “enhancement” of immune response is the use stimulating factors such as cytokines, which stimulate T cells to multiply and become stronger.
a4 Antibodies: Antibody-based therapy for cancer has been established for the past 15 years and is now one of the most successful and relevant strategies for treatment of patients with hematologic malignancies and solid tumors. The death of tumor cells using mAB may be the direct result of the antibody's action (through receptor blockage, for example), immune response mechanisms of cell death or specific effects of an antibody on the vasculature and tumor stroma.
Tumor antigens that have been used successfully include EGFR, ERBB2, vascular endothelial growth factor (VEGF), CTLA-4, CD20, CD30 and CD52. Serological, genomic, proteomic and bioinformatic databases have been used to identify antigens and receptors that are overexpressed in tumor cells or that are linked to genetic mutations identified as drivers of cancer cell proliferation.36
Administration of Conjugates of antibody and drug is an effective strategy of drug delivery that uses the directed action of the antibody together with cell death induced by a potent cytotoxic agent. Drug and antibody are bound together by a molecule. This modality of treatment helps to reduce the toxicity in non-target cells, guarantee a wide therapeutic window and overcome resistance to multiple drugs.37
b. Medications that inhibit the immunosuppressive effect of tumors.
Another strategy is to decrease the tumor cell defenses against the T lymphocyte. For example, neutralizing with antibodies the inhibitory factors and cytokines such as anti-interleukin-10 and transforming growth factor beta. Another possible strategy, already discussed, is to decrease the defenses of the tumor cell against T lymphocyte usingcheckpoint inhibitors, such as anti-PDL1 and anti-CTLA 4 antibodies which have been approved by the FDA (Table 7).
Immunotherapy.
| Kidney injuries | ||
|---|---|---|
| Interferon | Proteinuria, minimal glomerular lesions, FSH | |
| Anti-PD1 | Nivolumab | AIN, HTN, proteinuria, hypophosphatemia |
| Pembrolizumab | AIN | |
| Anti-PDL141 | Atezalizumab | AIN |
| Anti-CTLA-4 Ipilumumab | AIN, immune complexes GN | |
| CAR T cells | AIN, hyponatremia, hypokalemia, hypophosphatemia | |
| Tumor Lysis Symdrome |
GN: glomerulonephritis; FSH: focal segmental hyalinosis; HTN: hypertension; AIN: acute interstitial nephritis.
The nephrotoxic effect of conventional chemotherapy is well known by oncologists and nephrologists. In addition, the enormous growth of “target” treatments and modern immunotherapy, just commented, may lead to acute or chronic renal complications and alterations of water, electrolytes a acid-base regulation. Nephrologists and oncologists must be aware of these complications, not only to prevent and treat kidney damage but also for epidemiological pharmacological and therapeutic reasons.
Tables 1–6 show the most frequent renal alterations associated with the different treatments against cancer.38,39
Likewise, it should be kept in mind that excessive external or internal radiation may produce renal damage that is not observed after radiation received for diagnostic purposes. Clinically it is expressed as acute or chronic kidney disease, and may be associated with malignant hypertension. Histological lesions include endothelial damage with capillary thrombosis and fibrosis.5
Regarding hematological diseases, Onco-Nephrology should cover very relevant aspects of renal complications. Tumor lysis syndrome (observed in non-Hodgkin lymphoma, acute lymphocytic, lymphoblastic or myeloid leukemia, and less frequently in chronic leukemia, myeloma and solid tumors) causes hydroelectrolytic complications that are frequent reasons for consultation: hyperuricemia, hyperphosphatemia, hypocalcemia and hyperkalemia.
Onco-Nephrology, a working group of the Spanish Society of NephrologyThere are a large number of objectives to be covered by a SEN working group that deals with the cancer-kidney combination. The objectives are:
- –
Measurement of renal function in cancer patients.
- –
Cancer epidemiology in patients with CKD.
- –
Chemotherapy nephrotoxicity (ARI, crystal nephropathy, acute interstitial nephritis, thrombotic microangiopathy, segmental and focal hyalinosis, etc.).
- –
Hydroelectrolytic alterations secondary to the use of certain agents.
- –
Adjustment of doses and schedule of chemotherapy in patients with CKD.
- –
Treatments against cancer in dialysis patient.
- –
Kidney transplant and cancer in donor or recipient.
- –
Clinical efficacy and complications of new cancer treatments (anti/EGFR, anti/VEGF, anti/mTOR, anti/PD1 and PDL1, CAR T cell).
- –
Acute renal injury after administration of an iodinated contrast in patients with cancer and the influence of repeated examinations.
- –
Myeloma and dialysis management of light chains.
- –
Renal function after a nephrectomy.
- –
...
Future plans of the Spanish Society of Medical Oncology and the Society of Hematology include the development of training courses in epidemiology, patient monitoring, guidelines for the management of renal patients with cancer and the cancer patients with impaired renal function, and many other activities, including any relevant proposal by members of the SEN. Epidemiological data support the possibility of developing specific onconephrology clinic initially attended by a multidisciplinary team of oncologists, hematologists and nephrologists in first level hospitals covering the healthcare of at least half a million inhabitants. Including, if necessary, other medical specialists such as urologists, radiotherapists, pathologists, radiologists, palliative care, etc. It is about putting together the necessary health care specialist to provide optimal care to these patients with generation of protocols and educational activities.40
Conflicts of interestThe authors declare no conflict of interest.
Please cite this article as: de Francisco AL, Macía M, Alonso F, García P, Gutierrez E, Quintana LF, et al. Onco-Nefrología: cáncer, quimioterapia y riñón. Nefrología. 2019;39:473–481.
The Spanish Society of Nephrology (SEN) has initated a project with a new working group called Onco-Nephrology. A great activity is expected and the reasons that justify this program are being explained in this manuscript.