To the Editor
Syphilis is a systemic infectious disease caused by the organism Treponema pallidum. It is acquired by sexual contact, congenitally through the placenta, by contaminated human blood transfusion and by accidental direct innoculation.1 It begins when Treponema pallidum invades the cerebrospinal fluid (CSF).2,3
Its forms of presentation are classified as follows: early syphilis, late syphilis, neurosyphilis and congenital syphilis.4,5
Central nervous system involvement occurs in 5%-10% of those infected and in up to a third of cases progressing to advanced stages developing neurosyphilis.6
Currently, atypical presentation forms are prevalent with regard to the classical forms of progressive general paralysis and tabes dorsalis.7 The treatment is based on the administration of penicillin G sodium and, as a second option, cephalosporins.
We report the case of a patient who had renal transplant for 13 years and who came to the emergency Department with fever in the context of skin lesions and neurological symptoms.
CASE STUDY
A 39-year-old male with a third renal transplant, several episodes of pneumonia and hepatitis C virus carrier. He went on an exotic trip for two months, having at-risk sexual relations, without protection. He came in with low back pain and fever. His medical history showed fever, itching, whitish penile discharge, maculopapular rash, paraesthesia in legs and double vision.
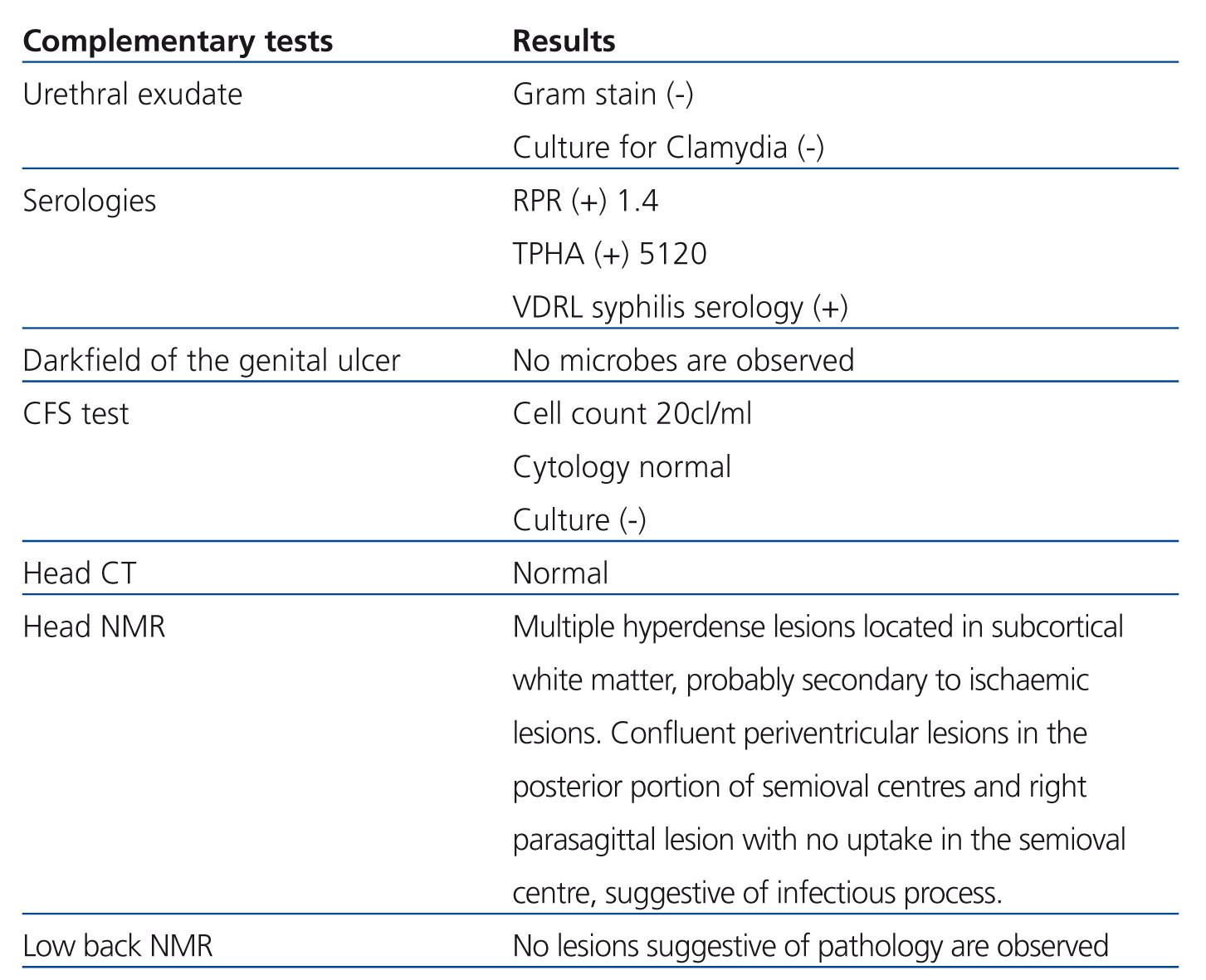
On examination: blood pressure: 177/106mmHg, temperature: 36.8°C, heart rate 120bpm. Maculopapular rash with palmoplantar keratoderma (Figure 1), with central predominance. Left sixth cranial nerve palsy (Figure 2), absence of deep tendon reflexes, decreased strength in both legs and dysesthaesia. Haemogram and leukocyte count normal, creatinine 1.8mg%, ionogram and blood gas normal. Other tests in Table 1.
With the early symptomatic diagnosis of neurosyphilis with meningitis and radiculitis, he was started on treatment with penicillin G sodium 24,000,000 IU intravenously for 3 weeks, with substantial improvement, recovering deep tendon reflexes after 8 days of treatment, with disappearance of low back pain and paraesthesia in the legs and with the cranial nerve palsy being partially resolved.
The patient was discharged after completing treatment, with tests every three months in an outpatient clinic. Progressive improvement of all neurological symptoms is observed along with decreased TPHA (Treponema pallidum Haemagglutination Assay) titres, RPR (rapid plasma reagin) and VDRL (Venereal Disease Research Laboratory) after one year of follow-up. Currently, after 5 years of infection, the patient is totally asymptomatic.
DISCUSSION
Symptomatic meningitis may occur years later, with headache and neck pain, confusion, nausea, vomiting, stiffness, seizures, decreased visual acuity, cranial neuropathies, cerebral arteritis, syphilitic leptomeningitis or gums causing back pain, sensory loss, incontinence, leg weakness or muscular atrophy.8
Although literature tells us that the symptomatic presentation may occur years after infection, in our case the evolution of the disease was accelerated and there was skin, genital and severe neurological manifestations.
The short period to the invasion of the central nervous system was striking since it is normal for neurosyphilis to present after two years in the latent phase.
The maculopapular rash (secondary syphilis) with palmoplantar keratoderma first led us to suspect the diagnosis of syphilis as the first possibility. In addition to the personal history of migration of the patient, the immunosuppression acquired was taken into account since he was a renal transplant patient.
Although no similar case has been found in literature, there are reports of high incidences of this disease in patients who are immunocompromised due to human immunodeficiency virus.9,10
CSF abnormalities associated with meningovascular neurosyphilis are generally less severe than in cases of acute meningitis.
Serological tests for syphilis include VDRL, RPR, FTA-ABS (fluorescent treponemal antibody absorption), particles for Treponema pallidum, TPPA (agglutination assay) and EIA (enzyme immunoassay).
These tests are still reactive for life in virtually all individuals regardless of previous treatment.
The treatment recommended by the Centres for Disease Control and Prevention (CDC), including ocular syphilis are:10 aqueous crystalline penicillin G (3 to 4 million units intravenously every four hours, or 24 million units per day as a continuous infusion) for 10 to 14 days, or procaine penicillin G plus probenecid. Doxycycline or ceftriaxone at high doses could be used as an alternative to penicilin.11
Follow-up should be carried out three and six months after treatment and then every six months until the CSF is normal and VDRL is unresponsive. Treatment must be repeated if any CSF follow-up sample increases four times in the VDRL titre or if there is an increase in leukocytes.8
CONCLUSION
Syphilis is an infectious disease which is not very prevalent in our setting and as such, is not often suspected.
Neurosyphilis has been considered a late manifestation of syphilis. In the case of our patient, the presence of a clinical profile, in which the symptoms of secondary syphilis (skin involvement) and neurological symptoms occur almost simultaneously is striking. We suspect that this is a consequence of the fact that it involves a patient on immunosuppression due to renal transplant anti-rejection medication.
We believe that, in addition to the lack of prevention by the patient, it is very important to consider immunodeficiency acquired by the renal transplant itself and we believe that it is an excellent opportunity to highlight the susceptibility of these patients to exposure to these type of microbiological agents; in cases of immune competitiveness, the presentation of this type of disease is probably not very aggressive.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Complementary tests
Figure 1. maculopapular rash
Figure 2. Left sixth cranial nerve palsy