Chronic kidney disease (CKD) is associated with high morbidity, burden, and resource utilization, and represents a major challenge for healthcare systems. The purpose of this study was to analyse the care patterns for these patients and to reach a consensus on the key factors that should be implemented for an optimal care model in CKD, through a multidisciplinary and integrative vision.
Materials and methodsA multidisciplinary panel of professionals with experience in the field of CKD was formed, composed of an advisory committee of 15 experts and an additional panel of 44 experts. Challenges and areas for improvement across the continuum of care were identified through review of scientific evidence and individual interviews with the advisory committee. Key factors for an optimal model of care in CKD were agreed and assessed using the Rand/UCLA consensus methodology (adapted Delphi), evaluating their appropriateness and necessity.
Results38 key factors were identified for an optimal CKD patient care model, organised into four challenges: (1) Development of CKD management models and increased visibility of the disease, (2) Prevention, optimisation of screening, early diagnosis and registration of CKD at all levels of care, (3) Comprehensive, multidisciplinary and coordinated monitoring, ensuring therapeutic optimisation and continuity of care, and (4) Reinforcement of CKD training for health care professionals and patients. 35 key factors were assessed by the panel as adequate and clearly necessary, and of these, 14 were considered highly imperative.
ConclusionsThere is consensus on the need to prioritise CKD care at both institutional and societal levels, moving towards optimal models of CKD care based on prevention and early detection of the disease, as well as comprehensive and coordinated patient monitoring and training and awareness-raising at all levels. The key factors identified constitute a roadmap that can be implemented in the different Autonomous Communities and contribute to a significant improvement in the patient’s care.
La enfermedad renal crónica (ERC) se asocia a una elevada morbilidad, carga y consumo de recursos, y constituye un importante desafío para los sistemas sanitarios. El objetivo de este trabajo fue analizar los modelos asistenciales de atención a estos pacientes y consensuar los factores clave que deben implementarse para un modelo óptimo de atención en la ERC, a través de una visión multidisciplinar e integradora.
Materiales y métodosSe conformó un panel multidisciplinar de profesionales con experiencia en el ámbito de la ERC, integrado por un comité asesor de 15 expertos y un panel adicional de 44 expertos. Se identificaron los retos y las áreas de mejora a lo largo de todo el proceso asistencial, a través de la revisión de la evidencia científica y entrevistas individuales al comité asesor. Se consensuaron los factores clave para un modelo óptimo de atención en la ERC, que fueron valorados utilizando la metodología de consenso Rand/UCLA (Delphi adaptado), valorando su adecuación y necesidad.
ResultadosSe identificaron 38 factores clave para un modelo óptimo de atención al paciente con ERC, estructurados en cuatro retos: (1) Desarrollo de modelos de gestión de la ERC y aumento de la visibilidad de la enfermedad, (2) Prevención, optimización del cribado, diagnóstico precoz y registro de la ERC en todos los niveles asistenciales, (3) Seguimiento integral, multidisciplinar y coordinado, asegurando la optimización terapéutica y la continuidad asistencial, y (4) Refuerzo de la formación en ERC a los profesionales sanitarios y pacientes. 35 factores clave fueron valorados por el panel como adecuados y claramente necesarios, y de estos, 14 fueron considerados altamente prioritarios.
ConclusionesExiste consenso sobre la necesidad de priorizar la atención de la ERC tanto a nivel institucional como social, avanzando hacia modelos óptimos de atención en ERC basados en la prevención y detección precoz de la enfermedad, así como en el seguimiento integral y coordinado de los pacientes y la formación y concienciación a todos los niveles. Los factores clave identificados constituyen una hoja de ruta implantable en las distintas Comunidades Autónomas que puede contribuir a una mejora significativa en la atención a estos pacientes.
Chronic kidney disease (CKD) is a major health problem worldwide due to its high prevalence, incidence, social and health burden, and growing economic costs.1 In Spain, the prevalence of CKD in any of its stages, has been estimated to be 14.4%2 to 15.1% for the general population,3 which could increase to more than 18% by the year 2040.4
CKD is associated with an increase in morbidity and mortality from the early stages of the disease, as well as with high frailty, increased hospitalizations, and reduced quality of life.3,5,6 It is also a risk multiplier for other chronic diseases (such as cardiovascular disease),1,7 and has been associated with high resource use and a considerable economic burden, which increases with disease progression8–10 and the presence of comorbidities.10 In the advanced stages of CKD, renal replacement therapy (RRT) accounts for between 2.5% and 3% of the National Health System (NHS) budget, even though it affects less than 1% of the population.11 Nevertheless, it continues to be an underdiagnosed disease12,13 that is largely unknown by society, probably due to the lack of symptoms that do not develop until the more advanced stages.14
CKD is generally included within the framework of chronic care models. In Spain, a specific framework document on CKD was developed in 2015 within the Strategy for Addressing Chronicity in the NHS,11 and Advanced Chronic Kidney Disease (ACKD)15 and Cardiorenal Units16 have been created and developed based on well defined standards as multidisciplinary and specialised functional models. In addition, in 2022, the Spanish information and consensus document for the detection and approach to CKD, signed by 10 scientific societies (SSs), was updated based on current recommendations and knowledge.5 It should be noted that the implementation of models, processes, programmes and units in CKD presents a high degree of heterogeneity among the different autonomous regions in Spain, possibly associated with differences in the organization of health care and the availability of resources.
In this context, the main objective of the intERCede project was to determine the care models for CKD patients at all stages of the disease and to reach consensus among a multidisciplinary panel of experts, on the key factors for an optimal model of care, defining a roadmap for the decision-makers and stakeholders involved in the management of this disease.
The consensus presented in this article has been endorsed by the following SSs: the Spanish Society of Nephrology (SEN), Spanish Society of Primary Care Physicians (SEMERGEN), Spanish Society of General and Family Physicians (SEMG), Spanish Society of Family and Community Medicine (semFYC), Spanish Society of Primary Care Managers (SEDAP), Spanish Society of Internal Medicine (SEMI), Spanish Society of Endocrinology and Nutrition (SEEN), Foundation Network of Diabetes Study Groups in Primary Health Care (redGDPS) and the Spanish Society of Health Managers (SEDISA).
MethodsThis study utilises RAND Corporation and University of California, Los Angeles methodology with adapted Delphi (Delphi-RAND/UCLA) through two rounds of individual assessment carried out by a multidisciplinary panel of experts during which the appropriateness (first round) and necessity (second round) of the key factors identified for an optimal care model in CKD were assessed.
The methodology was developed in four working phases (Fig. 1).
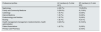
A multidisciplinary advisory committee (AC) was first established that included 15 professionals (Table 1) with extensive experience and knowledge in the field of CKD. An external methodological advisor also collaborated in coordinating and facilitating the project.
Profiles of professionals who were part of the advisory committee of this project.
| Professional profiles | AC members [n (% total AC)] | EP members [n (% total EP)] |
|---|---|---|
| Nephrology | 4 (26.7%) | 13 (29.5%) |
| Family and Community Medicine | 3 (20.0%) | 6 (13.6%) |
| Cardiology | 1 (6.7%) | 3 (6.8%) |
| Internal Medicine | 1 (6.7%) | 3 (6.8%) |
| Endocrinology and Nutrition | 1 (6.7%) | 3 (6.8%) |
| Nursing | 1 (6.7%) | 4 (9.1%) |
| Health management (management, medical direction, health administration | 3 (20.0%) | 8 (18.2%) |
| Patient Associations | 1 (6.7%) | 3 (6.8%) |
| Primary Care Pharmacy | 2 (4.5%) |
AC: advisory committee; EP: expert panel.
During the first two phases, CKD care in Spain was discussed and the care pathway of the CKD patient was analysed. This included a narrative review of the literature, as well as individual semi-structured interviews with the AC and a workshop. The result was, a preliminary proposal of the challenges and key factors for an optimal model of care in CKD, which was presented in the form of a structured questionnaire for evaluation in phase 3.
For assessment of these identified challenges and key factors, an additional multidisciplinary panel of 44 experts was formed (Table 1). Overall, the Delphi panel (AC and expert panel) was made up of 59 specialists representing different care models and geographical areas, all of them with experience and knowledge of CKD from their professional profile and field.
For the consensus and prioritisation of the key factors proposals, two rounds of assessment were carried out by means of a structured questionnaire via an online platform, using the RAND/UCLA consensus methodology17 (adapted Delphi) (Fig. 1, right side). These rounds were conducted in January and March 2023, respectively.
A 9-point Likert scale was used during the individual rating rounds to determine the appropriateness and necessity of the key factors. The response categories were described by linguistic qualifiers in three regions (1−3: inappropriate or unnecessary; 4−6: opinion neither for nor against, indeterminate; 7−9: appropriate or necessary). Experts were allowed to provide comments and observations in both rounds but were not permitted to exchange information; key factors not scored were analysed as missing cases for statistical purposes. The data obtained in the two rounds were analysed statistically (via Microsoft Excel) to measure the degree of appropriateness, necessity and concordance, using the following metrics: frequency, median, interquartile range, mean and standard deviation.
During the first round, the Delphi panel assessed the appropriateness of the preliminary proposal of challenges and determining factors. The application of the key element was considered appropriate when the health benefit expected from its use outweighed by a large margin the potential negative consequences or risks by a large margin. Each factor was analysed and classified according to the degree of appropriateness and concordance of the responses (Table 2). This was followed by a workshop with the AC to discuss specific key elements with indeterminate consensus, and elements with proposals for wording adjustments or with greater disparity.
Methodology adapted from RAND/UCLA used for assessment of the key factors: level of appropriateness, necessity and agreement.
| Assessment round | Aspect assessed | Assessment | Criterion |
|---|---|---|---|
| First Delphi rating round | Degree of appropriateness | Appropriate | Median in the upper third of the appropriateness scale (7,8,9) |
| Inappropriate | Median in the lower third (1,2,3). | ||
| Indeterminate | Median in the middle (4,5,6). | ||
| Degree of agreement | Agree | At least seven-ninths (77.77%) of the panellists score in the range (1–3; 4–6; 7–9) contained in the median | |
| Disagree | At least one third (33.33%) of the panellists rate the recommendation in the region 1–3, and at least one third (33.33%) of the panellists rate it in the region 7–9. | ||
| Indeterminate | Cases that do not meet the above. | ||
| Second round of Delphi assessment | Degree of necessity | Necessary | Median in the upper third of the need scale (7,8,9). |
| Unnecessary | Median in the lower third (1,2,3). | ||
| Indeterminate | Median in the middle (4,5,6). | ||
| Agree | At least seven ninths (77.77%) of the panellists score in the range (1–3; 4–6; 7–9) contained in the median. | ||
| Disagree | At least one third (33.33%) of the panellists rate the recommendation in the region 1–3, and at least one third (33.33%) of the panellists rate it in the region 7–9. | ||
| Indeterminate | Cases that do not meet the above. |
In the second round, the panellists evaluated the need for the proposal of key factors adjusted after the consensus and assessment of the results obtained after the workshop. A key element was considered as necessary when it met the following four criteria: appropriate; it would be inappropriate or malpractice not to implement it; there is a reasonable possibility that it would benefit the patient; and the magnitude of the expected benefit is not small. Each was analysed and classified according to the degree of necessity and the concordance of the responses (Table 2). After this round, another workshop was held with the AC, in which the determining factors with indeterminate necessity were discussed, as well as those in which considerations had been presented.
Finally, the definitive list of challenges and key factors was obtained for an optimal model of care for patients with CKD. Those that obtained an average score of 8 or higher in terms of both appropriateness and necessity were considered as priorities. The results were included in a final report.
No patient data were collected in this project, so no review or approval by the ethics committees of the participating hospitals was required.
ResultsBased on the analysis of current patterns of care and the identification of the main patient pathways, the AC established a series of minimum characteristics for optimal models of CKD care: (1) prevention of the disease and periodic screening of patients with risk factors; (2) early diagnosis and appropriate recording thereof at all levels of care; (3) comprehensive and individualised follow-up; (4) proactive care, integration and coordination between areas, specialties and levels of care; (5) reinforcement of the training and awareness of patients and healthcare professionals throughout the entire care pathway; (6) evaluation of health outcomes and of the quality of life, experience and perspective of the person; (7) and development of information systems that facilitate the different stages of the care process.
Considering these characteristics, in addition to the analysis of the main areas for improvement and good care practices, the main challenges and key factors for progress in the development of optimal models of care in CKD were established.
In the first Delphi round, a total of seven challenges and 68 key factors were initially identified. Of these 68, 59 were rated as appropriate and with agreement, while nine received an indeterminate consensus. Following the deliberations of the AC during the workshop, and based on the clarifying considerations and observations for improvement made by the panellists, synergies between different key factors were identified, integrating them into those that were more precise and avoiding the dispersion of information (Appendix A Supplementary Fig. S1). None were eliminated. In addition, editorial changes were made to the initial proposal to ensure an accurate assessment aligned with a clear understanding. As a result, a final list of 38 key elements was obtained, structured into four challenges (Table 3), which were then subjected to a second round of assessment.
Challenges to achieving an optimal model of care for patients with CKD.
| Challenges of an optimal CKD care model | Number of key factors included |
|---|---|
| 1) Development of CKD management models and increased visibility of the disease | 12 |
| 2) Prevention, optimisation of screening, early diagnosis and registration of CKD at all levels of health care. | 5 |
| 3) Comprehensive, multidisciplinary and coordinated follow-up, ensuring treatment optimisation and continuity of care. | 15 |
| 4) Reinforcement of CKD training for healthcare professionals and patients | 6 |
Challenge 1 arose from considering the poor visibility and prioritisation of CKD at all levels and in models and specific macro-, meso- and micro management tools. Challenges 2 and 3 arose from the description of the care pathway and the current room for improvement in terms of prevention, screening and early detection of CKD, as well as the need to ensure a comprehensive and individualised approach to the patient and coordination between the different professionals involved. Finally, challenge 4 arose from the need for training of healthcare professionals and also patients themselves and family members/caregivers, as key aspects necessary to optimise the health care model.
After the second round of assessment, of the 38 key factors, 35 were considered appropriate and clearly necessary, while three were considered appropriate but not clearly necessary. The final score and rating obtained for each of the key elements is detailed in Appendix Supplementary Table S1. In cases where the factor was the result of the integration of two or more factors, the appropriateness was calculated as the mean of the appropriateness score of the consolidated key aspects. The mean score of the challenges in terms of necessity was 8, with the exception of the second challenge, which scored the highest with a mean necessity score of 9.
As a final result, a total of 14 key factors were identified as high priority (Table 4). A matrix of prioritisation of all key elements based on on the mean appropriateness and necessity is shown in Appendix A Supplementary Figure S2. None of the factors in challenge 4 were considered as priority.
Priority key factors by challenge.
| n | Key factor |
|---|---|
| Challenge1. Develop CKD management models and increase the visibility of the disease. | |
| 1 | Update the national strategic plan for CKD, with a special focus on prevention and early treatment, from a multidisciplinary and comprehensive viewpoint, with the participation of the main Patient Associations (PAs) and Scientific Societies (SSs). |
| 2 | Promote the approach to CKD as a priority in health plans and chronic disease strategies at regional and/or local level. |
| 3 | Promote the implementation of those protocols and procedures on the approach to CKD that have already been developed and agreed upon. |
| 6 | Develop clinical decision support tools and clinical dashboards integrated into the Electronic Health Record or laboratory reports. |
| 7 | Promote the definition and homogenisation of specific laboratory test profiles for patients at risk of CKD. |
| Challenge 2. Prevention, optimisation of screening, early diagnosis and registration of CKD at all levels. | |
| 13 | Design and establish protocols for the prevention, monitoring and control of CKD risk factors, implementing CKD screening in the patient profiles defined in the guidelines/consensus documents. |
| 15 | Promote actions to increase awareness of the importance of assessing albuminuria in at-risk populations, and develop tools that enable its automatic request when values compatible with possible impaired renal function are detected. |
| 17 | Provide adequate, clear and accurate information to patients from diagnosis about CKD, its stage and prognosis. |
| Challenge 3 Comprehensive, multidisciplinary and coordinated follow-up, ensuring treatment optimisation and continuity of care. | |
| 20 | Strengthen communication channels and two-way telematic cross-consultation systems between primary care, nephrology and other hospital specialties, as well as the creation of protocols and working groups and the implementation of integrated information systems. |
| 22 | Implement alert systems to identify those patients who require treatment adjustment, patients who meet the criteria for referral to nephrology and patients at greater risk of CKD progression based on their laboratory parameters. |
| 24 | Promote the participation of primary care and nephrology nurses from the early stages of the disease in the monitoring and assessment of CKD patients, as necessary, and implement communication tools between, primary care and nephrology |
| 28 | Promote treatment optimisation for CKD patients in pre-dialysis stages. |
| 29 | Implement screening for cardiovascular disease and type 2 diabetes mellitus as part of the follow-up of the CKD patient. |
This study allowed us to identify various aspects to move towards optimal models of care in CKD with a high level of agreement and unanimity (Appendix Supplementary Table S1). We confirmed the existing consensus on the need to prioritise CKD both at social and health authority level, as well as the need to promote a paradigm shift towards prevention and an early approach. This will ensure comprehensive, multidisciplinary and coordinated follow-up throughout the disease process, together with training and raising awareness among professionals, patients and family members/caregivers. To date, and following a review of the scientific literature, this is the first study that identifies the challenges and key factors to advance in the development and implementation of optimal models of care in CKD at the national level.
The 38 recommendations or key factors proposed are intended to serve as a basis for advancing the development of optimal CKD models adapted throughout Spain, taking into account local models and available resources, thereby improving the quality of care.
The discussion is structured by challenges and focuses especially on these key priority factors, since these are the ones that mark the most immediate start of the roadmap. Once the essential elements have been implemented, the other basic elements identified should be incorporated progressively.
Challenge 1. Developing CKD management models and increasing the visibility of the diseaseThere was a clear consensus on the need to develop specific planning lines or management models for CKD at all key levels, and to be able to implement strategies to achieve better patient outcomes and mitigate the burden and morbidity and mortality associated with the disease.5,9,18 An updated and specific national strategic plan for CKD was considered to be of great importance for efficient and coordinated management of resources. Despite the fact that national CKD policies have been recognised as essential elements in healthcare systems,7,19 only one third of countries worldwide have adopted them.
Today, there are nephroprotective drugs20 that have been shown to delay the progression of kidney disease and its associated morbidity and mortality, so this consensus identifies the prevention and early management of CKD as central elements of health policies.
The results of the study highlight the need to implement the agreed-upon protocols as a strategy to improve the quality of care.21 Nevertheless, the rates of compliance with the recommendations established for the follow-up of risk factors in CKD are lower than desired.22 Unanimity was also reached regarding the evaluation of outcomes through the implementation of indicators and objectives, especially in the early stages of the disease. There have been several attempts in Spain to implement quality indicators in nephrology as a management method to improve patient outcomes.23 However, the lack of institutional support together with the scarce symptoms until advanced stages of the disease process have hindered the implementation of this type of initiative.
Priority should continue to be given to the development of clinical decision support systems and the standardised definition of specific laboratory profiles for patients at risk of CKD. These types of tools are still underdeveloped and not homogeneously implemented at national level.24
In order to achieve a comprehensive vision, patient associations (PAs) and family members should be involved in the formulation and evaluation of plans, strategies and protocols, in line with the trends observed at European level,21 although in Spain the role of the patient in this area is still at very early stages.
Challenge 2. Prevention, optimisation of screening, early diagnosis and registry of CKD at all healthcare levelsPrevention of CKD, screening of patients with risk factors and early detection of the disease were recognised as the most urgent priorities to be addressed, given the lack of systematic implementation of CKD screening and the current underdiagnosis and diagnostic delay.2,12–14
The accessibility of screening tests in the NHS and the availability of effective therapeutic interventions to delay the progression of CKD and reduce cardiovascular risk,25 together with the arguments already described, are key conclusions to definitively promote the early detection of CKD in Spain and the paradigm shift towards primary and secondary prevention. Recent studies have shown that the detection of CKD is cost-effective in at-risk patients,26 even in the general population, through screening for of albuminuria.27
At present, however, the detection of CKD by measuring the estimated glomerular filtration rate (eGFR) and urine albumin/creatinine ratio (ACR) is approximately 50% in the most favourable situations.28,29 This underscores the need to encourage the active search for the disease through greater awareness and the development of tools that allow urinary albumin tests to be automatically requested. All of this, is to facilitate the early detection of CKD, since it has been observed that delaying the diagnosis of stage III CKD by one year increases the risk of progression by 40%.30
In addition, recent studies in Spain show that, although the use of antidiabetic drugs with proven cardiorenal benefits has increased over the years, their use remains low.31
This situation has a negative effect on patient prognosis and quality of life, as well as on the associated burden and costs, which are exacerbated as CKD progresses.8–10,32,33
The systematic implementation of screening should be complemented with the recording or coding of the diagnosis of CKD at all levels of care, as already stated in the 2015 CKD Framework Document.11 Recording the CKD diagnosis is considered a fundamental aspect to reduce the risk of progression and minimise adverse clinical outcomes.30 New real-world evidence has shown that the prevalence of non-diagnosed/non-recorded CKD stage III is 62%–96%, remaining high even in patients with comorbidities at high risk of disease progression.13
In other words, despite the availability of effective resources for the prevention, detection and early treatment of CKD, no full comprehensive measures have been adopted in this area.
Likewise, during the study, the importance of providing the patient with correct, clear and precise information from the time of diagnosis was highlighted, taking into account his or her emotional state. According to the manifesto of individuals with kidney disease presented in 2015, patients with CKD should receive information and counselling that truly helps them to make shared decisions at this key moment in their lives.34 Counselling at-risk subjects on the symptoms and progression of CKD could help to detect CKD at earlier stages and improve its prognosis, as suggested by the results of a European survey conducted in 2023.35
Finally, it is notable that, although 21% of the prioritised key factors fall within challenge 2, an analysis of the complete set of priority factors revealed that 64% of them are directly related to, or include to some extent, the importance of early diagnosis and management of CKD. This reinforces the urgent need to prioritise interventions associated with the prevention, optimisation of screening and early diagnosis of CKD.
Challenge 3. Comprehensive, multidisciplinary and coordinated follow-up, ensuring treatment optimisation and continuity of careSeveral studies have demonstrated the benefits of multidisciplinary models of care of patients with CKD, including greater cost-effectiveness and coordination of care.36,37 A consensus was reached on the importance of incorporating a holistic vision in these models, including services such as individualised nutritional, psychological, social-health and community support, which positions the reduction of symptoms and the impact of the disease on daily life as a key part of the approach to the individual patient. In fact these are the aspects most prioritised by patients according to different studies.38,39
It was considered a priority to guarantee smooth two-way communication between primary care and nephrology.. The need to optimize the referral process to nephrology has been evidenced in different studies.40–42 In this regard, the panellists agreed that the development of telematic consultation systems and efficient communication channels would help to optimise coordination and appropriate referral between the different healthcare levels, specialties and resources.
Early management and pharmacological treatment of patients was considered an aspect of special importance to improve the approach to this disease, delay progression from early stages, reduce costs and improve patient health outcomes.43 Given the high prevalence of comorbidities in patients with CKD10, as well as their impact on increased hospitalisations and mortality,14 the optimisation and standardisation of treatment and the definition of therapeutic objectives were considered essential. These aspects are especially relevant in early stages of CKD (I-III), since variability in the therapeutic approach and follow-up of patients has substantial implications for their prognosis.44
To this end, the development of alert systems in the medical record to facilitate the prevention of nephrotoxicity, patient referral, or identification of patients at risk of progression has been valued as a favourable tool to optimise the monitoring of these patients throughout the care process; the importance of ensuring that the systems are robust and balanced was also highlighted.45
Challenge 4. Reinforcement of training in chronic kidney disease for healthcare professionals and patientsThe importance of ongoing training for healthcare professionals and also patients, family members or caregivers as an integral part of addressing CKD was unanimously recognised. The fact that no key factor was a priority in this challenge could be due to the fact that, in the present situation, it is considered necessary to focus efforts on other elements that would most require advancement and development as a priority. Furthermore, the results are consistent with the composition of the Delphi panel, suggesting existence of a possible bias in this regard.
Ongoing, complete and individualised education of people with CKD at the most appropriate emotional moment is a key aspect to achieve greater control of their health, as well as to be able to participate in shared decision-making.34,46 Barriers to effective education of patients with CKD include insufficient awareness and a shortage of staff and time to reinforce training.47 In addition, limited evidence has been identified on training in shared decision-making among healthcare professionals who treat patients with CKD.48
Various initiatives have been developed in Spain to support the empowerment and training of patients with CKD, promoted by the PAs, the healthcare setting and the SSs. Similarly, the Autonomous Regions are developing different actions to improve the training of healthcare professionals in CKD. The growing capacity and access to technology provide new opportunities to improve the education and awareness of CKD for all interested participants.49
As the main limitations of the study, the participation of a broader panel of experts would have been desirable to achieve greater representation of the different specialties, as well as the inclusion of other professionals with different expertises such as social work and psychology and a greater number and diversity of patients, of different complexity and circumstances, as well as their caregivers.
ConclusionsThe results of this project show that there is consensus on the need to prioritise the care of CKD at both institutional and social levels, as well as to encourage a paradigm shift towards its prevention and early management, while guaranteeing comprehensive, multidisciplinary and coordinated monitoring throughout the disease process in addition to training and raising awareness among professionals, patients and family members/caregivers.
For the first time, this work provides a roadmap to move towards the definition of optimal models of care in CKD from a multidisciplinary perspective, through initiatives and actions that can potentially be implemented in the short term in the different health areas of Spain.
FundingThis Delphi intERCede project has been coordinated by Ascendo Sanidad&Farma, with the support and funding of Boehringer Ingelheim (BI) Spain. BI did not exert any type of influence on the opinions of the participating experts or the final consensus.
Conflict of interestJosé Luis Górriz has received honoraria for lectures from AstraZeneca, Menarini, Boehringer-Ingelheim, Lillly, Bayer and Novo Nordisk. He has participated in advisory boards of Menarini, Boehringer-Ingelheim, AstraZeneca and Bayer.
Roberto Alcázar Arroyo has received f honoraria for continuing education activities from AstraZeneca, Boehringer-Ingelheim, Lilly, Bayer, Vifor-cls and Novo Nordisk. He has participated in advisory boards of Boehringer-Ingelheim, AstraZeneca and Bayer.
Patricia Arribas has received honoraria from Boehringer-Ingelheim.
Sara Artola has received honoraria for lectures from AstraZeneca, Menarini, MSD, Sanofi, Boehringer-Ingelheim, Lillly, Bayer, Almirall and Novo Nordisk. He has participated in advisory boards of Menarini, MSD, AstraZeneca and Alter.
Sergio Cinza-Sanjurjo has received honoraria for lectures from AstraZeneca, Boehringer-Ingelheim, Lillly and Bayer. He has participated in advisory boards of Boehringer-Ingelheim and Bayer. He has received research funding from AstraZeneca, Boehringer-Ingelheim, and Bayer.
Rafael de la Espriella has received honoraria for lectures from AstraZeneca, Boehringer-Ingelheim, Lillly, Bayer, Novartis, Pfizer, Daiichi Sankyo, and Novo Nordisk. He has served on advisory boards for Boehringer-Ingelheim, AstraZeneca, Pfizer, and Bayer.
Javier Escalada has received honoraria for lectures from AstraZeneca, Boehringer-Ingelheim, Esteve, Lillly, and Novo Nordisk. He has served on advisory boards for AstraZeneca, Boehringer-Ingelheim, Lilly, and Novo Nordisk.
Lisardo García-Matarín has received speaker fees from AstraZeneca, Boehringer-Ingelheim, Lilly, Chiesi, GlaxoSmithKline, Bial, Menarini, Teva, Novartis, Pfizer, Sanofi Aventis, FAES, Novo Nordisk, and Vifor Pharma. He has served on advisory boards from Boehringer-Ingelheim, AstraZeneca, Daiichi Sankyo, and GlaxoSmithKline.
Juan Carlos Julián declares that his entity, the National Federation of ALCER Associations, receives or has received in the last three years revenue in compensation for its participation in advisory boards for the companies Astellas Pharma Europe LTD, Astrazeneca, Bristol-Myers Squibb, Bayer Hispania, Boehringer-Ingelheim, Ipsen Pharma, GlaxoSmithKline, Hansa Biopharma AB, Novartis Inc., Novartis Farmacéutica, Pfizer Ltd., and Travere Therapeutics. The National Federation of ALCER Associations receives or has received in the last three years financial contributions for business collaborations within the framework of the Spanish Patronage Law, from the companies Astellas, Astrazeneca, Baxter, Bayer, Bristol-Myers Squibb, Bayer Hispania, Boehringer-Ingelheim, Chiesi, CSL Vifor, Deiters, Diaverum, Fresenius Medical Care, GlaxoSmithKline, Hansa Biopharma, Ipsen, Novartis, Pfizer and Sanofi.
José Pablo Miramontes González has received honoraria for lectures from Boehringer-Ingelheim, Lillly and Novo Nordisk. He has participated in advisory boards of Novo Nordisk.
Félix Rubial has received honoraria for lectures from Astellas, AstraZeneca, Boehringer-Ingelheim, Pfizer and Sandoz.
Mercedes Salgueira has received honoraria for speaking engagements and advisory board membership from AstraZeneca, Vifor, GlaxoSmithKline, Amgen and Boehringer-Ingelheim.
María José Soler has received honoraria for speaking engagements from AstraZeneca, Boehringer-Ingelheim, Lilly, Bayer, Vifor, ICU Medical, Fresenius, Travere Therapeutics y Novo Nordisk. She has participated in advisory boards of Novo Nordisk, Menarini, Boehringer-Ingelheim, AstraZeneca, Mundipharma, Vifor, ICU Medical, GE Healthcare, Travere Therapeutics y Bayer.
Jose Luis Trillo Mata has received honoraria for speaking engagements from AstraZeneca, Boehringer-Ingelheim, Lilly and Novo Nordisk. He has participated in advisory boards of Boehringer-Ingelheim, AstraZeneca and Bayer.
The authors would like to thank all the individuals who have collaborated in the development of the intERCede project and in the preparation of this article. The authors meet the criteria of authorship recommended by the International Committee of Medical Journal Editors (ICMJE) and did not receive any payments in relation with the development of this manuscript.
Ascendo Sanidad&Farma provided editorial assistance in the writing of the manuscript, which was contracted and funded by Boehringer Ingelheim (BI) Spain. BI had the opportunity to review the manuscript to verify its medical and scientific accuracy, as well as possible intellectual property considerations.