Intradialytic hypertension (IDH) is a poorly understood phenomenon with no consensus on its definition, etiology, or related factors, and there is limited evidence on its consequences.
ObjectiveTo determine the prevalence of IDH according to different definitions in hemodialysis (HD) units, with different clinical practices and assessment of possible events after 18 months have passed.
Materials and methodsA cross-sectional observational study was conducted in 2 HD units, including all prevalent patients from March 2021 to September 2022. We established 3 definitions of IDH:
- •
Def 1: Mean arterial pressure (MAP) difference pre- and pos-HD >15 mmHg
- •
Def 2: Systolic blood pressure (SBP) difference pre- and pos-HD >10 mmHg
- •
Def 3: SBP difference >0 and ultrafiltration rate (UFR) >5 ml/kg/h
IDH was considered present if the criterion was met in more than 50% of the 6 consecutive sessions (2 weeks) of follow-up. Personal history, medications, dialysis characteristics, and pre- and post-HD biochemical data were collected. Residual renal function (RRF) was considered as urine output >250 ml/24 h. At 18 months, the possible events of the group were analyzed.
ResultsWe included 169 patients (68% men) with a mean age of 67.9 (14.2) years and a median HD duration of 34.5 (IQR 17.5–67.5) months. Of these, 94 come from one unit and 75 from the other. The prevalence of IDH was 8.3% according to Def 1, 27.2% according to Def 2, and 29.6% according to Def 3. Def 2 showed an association with a history of previous hypertension, use of renin-angiotensin system inhibitors (RASIs), and furosemide, as well as with patients with RRF. Def 3 showed an association only with coronary artery disease. There was an association with different prescriptions of dialysis fluids. Catecholaminergic hormones and aldosterone did not increase in patients with hypertension during the HD session. They did not present a higher incidence of cardiovascular events or mortality at 18 months.
ConclusionsIDH has different prevalence rates depending on the definition used and the studied center. The future poses an important challenge: to determine which definition correlates with higher morbidity and mortality and the role of differences found in different HD units.
La hipertensión arterial intradiálisis (HTAID) es un fenómeno poco conocido del que no existe consenso en su definición, ni datos sobre su etiología o factores relacionados, y hay poca evidencia sobre sus repercusiones.
ObjetivoDefinir la prevalencia según diferentes definiciones en dos unidades de hemodiálisis (HD), de dos hospitales diferentes, con distinta práctica clínica y valoración de posibles eventos después de haber pasado 18 meses.
Material y métodosEstudio observacional transversal realizado en 2 unidades de HD donde se incluyeron todos los pacientes prevalentes desde marzo 2021 hasta septiembre 2022. Establecimos 3 definiciones de HTAID:
- •
Def 1: Diferencia de presión arterial media (PAM) pre- y pos-HD > 15 mmHg
- •
Def 2: Diferencia de presión arterial sistólica (PAS) pre- y pos-HD > 10 mmHg
- •
Def 3: Diferencia de PAS > 0 y UFR > 5 ml/kg/h
Consideramos había HTAID si se cumplía el criterio en más del 50% de las 6 sesiones consecutivas (2 semanas) de seguimiento. Se recogieron antecedentes personales, medicamentos, características de diálisis y datos bioquímicos pre y post HD. Se consideró función renal residual (FRR) una diuresis >250 ml/24 h. Se analizó a los 18 meses los posibles eventos del grupo.
ResultadosIncluimos 169 pacientes (68% hombres), con una edad media de 67,9 (14,2) años y una mediana de tiempo en HD de 34,5 (AIC 17,5–67,5) meses. De ellos 94 provienen de una unidad y 75 de la otra. La prevalencia de HTAID fue según Def1 (8,3%), Def 2 (27,2%) y Def3 (29,6%). Se evidencia una asociación en la Def2 con antecedente de HTA previa, uso de inhibidores del sistema renina angiotensina (ISRA) y furosemida y en los pacientes con FRR, en la Def3 solo asociación a coronariopatía. Existe asociación con las diferentes prescripciones de los líquidos de diálisis. No aumentaron las hormonas catecolaminérgicas y aldosterona en los pacientes con HTAID durante la sesión de HD. No presentaron mayor incidencia de eventos cardiovasculares o mortalidad a los 18 meses.
ConclusionesLa HTAID tiene una prevalencia distinta tanto según la definición utilizada como la unidad estudiada. El futuro plantea un importante reto: conocer cuál de las definiciones determina una mayor implicación clínica y el papel que tienen las diferencias encontradas en las distintas unidades de HD.
Intradialytic arterial hypertension (IDHTN) is the increase in blood pressure (BP) during hemodialysis (HD), a phenomenon that many describe as paradoxical, due to the fact that it is the opposite effect to that which would be expected, especially in patients undergoing volume removal. It is a phenomenon that has been poorly studied in most respects and with little conclusive data.1–3
To start, it should be known there is no widely accepted definition of IDHTN. These are some of the criteria proposed in different studies:
- -
Increase in mean arterial pressure (MAP) ≥15 mmHg during the HD session2 in 2/3 of the last 12 sessions.4
- -
Increase in systolic blood pressure (SBP) ≥10 mmHg during HD session in 4/6 sessions.5,6
- -
Increase in BP despite ultrafiltration in more than 50% of the last 6 sessions7 or during 4 consecutive sessions.3
The epidemiology is also unknown, since the prevalence of IDHTN has not been studied systematically. According to different publications, the prevalence is between 5 and 15%.5,8 There is little data about its consequences; it has been described a higher risk of hospitalization or death in the short term (6 months),9 a 2-year decrease in survival in those patients with pre-dialysis BP <120 mmHg.5 Furthermore, this situation often requires early interruption of the HD session, to administer antihypertensive drugs, and to prolong the patient's stay in the dialysis unit or in the hospital, with immediate negative consequences such as under-dialysis, poorer quality of life, and an increase in health care costs.
There are several theories to explain the pathogenesis, but with contradictory results. The hypotheses proposed to explain this phenomenon are the following: (1) Excess of volume,7 which is also described in patients with pre-dialysis arterial hypertension (HTN)10; (2) Activation of the sympathetic nervous system (SNS)11,12; (3) Activation of the renin angiotensin aldosterone system (RAAS)13; (4) Endothelial dysfunction leading to vasoconstriction3; (5) Net sodium gain during the HD session14–16; (6) Elimination of antihypertensives drugs during the dialysis session9; (7) Use of erythropoietin-stimulating agents17,18; and (8) Increased vascular stiffness.19
There are no clear strategies for the management of IDHTN. Some approaches applied are: strict control of intravascular volume,20 pharmacological blockade of the SNS or SRAA, modifications of the sodium (Na) concentration of the dialysis fluid (DF), avoid high hemoglobin levels and hypotensive drugs that are eliminated during HD21
In summary, at the present time the concept of IDHTN is not clearly defined, its pathophysiology is unknown, its epidemiological characteristics have not been established, and there is no specific therapeutic management. Furthermore, despite knowing that HTN is a clear cardiovascular risk factor, there are no studies that analyze the relationship between IDHTN and cardiovascular morbidity and mortality.
Taking into consideration these premises, we wanted to study the prevalence of IDHTN according to the different definitions and the factors that may be associated, whether they are epidemiological, clinical or related to HD techniques, and to determine its consequences.
MethodsThis is a prospective observational multicenter study conducted on prevalent patients in March 2021, with follow-up until September 2022, in 2 HD units: Hospital Clínica Benidorm (HCB) and Hospital Universitario Infanta Leonor (HUIL). The study was approved by the Clinical Research Ethics Committee of the HUIL (Internal Code 003/21).
Patients included in the study were all prevalent patients (≥3 months on HD) of legal age, who had started renal replacement therapy in the hospital HD facilities before March 1, 2021, with a minimum of 2 weekly sessions and after having signed the informed consent.
Definition of ID HTNBlood pressure (BP) was measured using the sphygmomanometers of the HD monitors. The first BP measurement was that taken after connection and the last BP measurement was that taken before disconnection. We consider that these are 2 conditions in which the patient is in the same state of activity-rest at the beginning and theend of the HD session.
Its prevalence has been defined according to the different definitions used in previous studies, establishing the diagnosis if the criterion is met in more than 50% of 6 consecutive follow-up sessions:
- -
Definition 1: Difference between the last and first measurement of MAP ≥ 15 mmHg,2,4
- -
Definition 2: Difference between the last and first measurement of SBP ≥ 10 mmHg,5,6
- -
Definition 3: Any increase in SBP between the last and first measurement.with a rate of ultrafiltration greater than 5 ml/kg/h (minimum rate of UF considered as significant).3,7
The data collected through the computer program of the participating centers (Nefrolink®) were:
- -
Demographic data: age, sex, kidney disease etiology, previous HTN, other cardiovascular risk factors (smoking, diabetes mellitus [DM], dyslipidemia [DLP], obesity, physical activity), history of cardiovascular disease (coronary heart disease, cerebrovascular disease, peripheral vascular disease) and time on HD.
- -
Antihypertensive treatment: calcium channel antagonists, loop diuretics, renin angiotensin system inhibitors (RAASI), alpha-adrenergic antagonists, beta -blockers.
- -
Monthly Biochemical data: sodium, potassium, calcium, bicarbonate, parathyroid hormone (PTH), hematocrit and evaluation of residual renal function (RRF) in any patient with a diuresis volume >250 ml/24 h, calculating glomerular filtration by mean creatinine and urea clearance (mClUN-cr).
- -
Usual HD parameters: HD modality (conventional or online hemodiafiltration) and dialysis fluid composition (bicarbonate, sodium, calcium, potassium).
- -
Blood sample from the arterial line at the time of connection and at the end of the session, in patients diagnosed with IDHTN (without differentiating between Def 2 and Def 3): glucose, sodium, potassium, chloride, bicarbonate, calcium and hormones (epinephrine, norepinephrine, dopamine and aldosterone) using the HPLC system with electrochemical detector in plasma (Chromosystem®). The values were not adjusted to taking into account the ultrafiltration performed.
- -
At 18 months patients were categorized into 4 possible outcomes: death, cardiovascular event, leaving HD for any other cause or continuing in HD).
Statistical analysis was performed with the STATA® 17 program (StataCorp LLC®).
For quantitative variables, the mean (x̄) was used as a measure of central tendency and the standard deviation (SD) as a measure of dispersion. Median (Md) and interquartile range (IQR) are presented for strongly skewed data. Tables of frequency are presented for qualitative variables. The normal distribution of the variables was ascertained by box plot and cumulative distribution function.
The simple association study was performed using Student's t test and Chi-square test. Fisher's exact test and the Wilcoxon rank test were used as nonparametric tests. The simple association between qualitative variables was performed by calculating odds ratios.
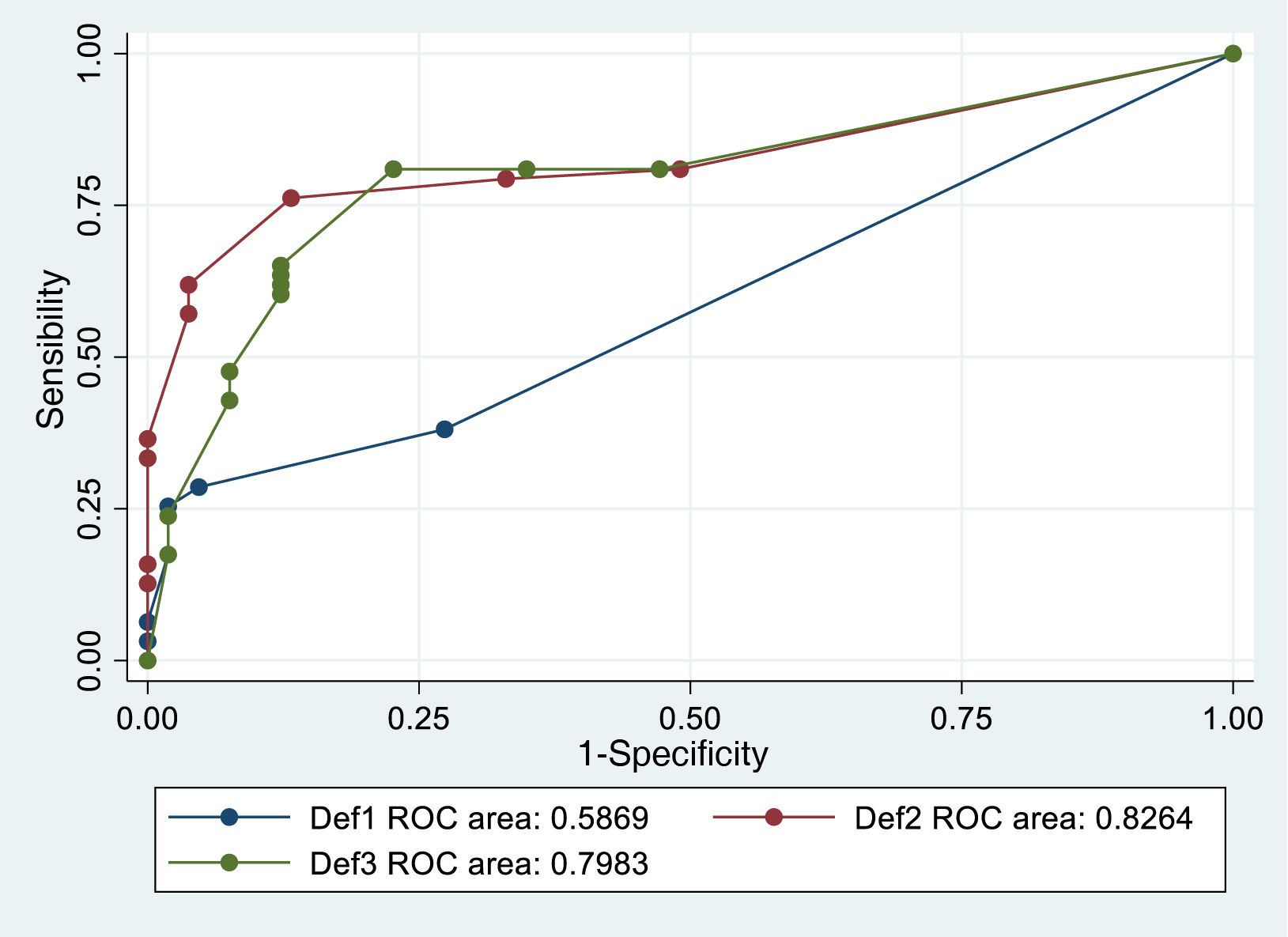
The comparison of the accuracy of the diagnostic definitions was assessed using sensitivity and specificity study and an ROC curve with composite reference standard. For this standard, “hypertensive” was defined as a patient who met at least one of the 3 definitions of hypertension, considering the percentage of successes for each definition over 6 consecutive dialysis sessions.
ResultsThere were included 169 patients on HD (115 males and 54 females), with a mean age of 67.9 (14.2) years, with a median time on HD of 34.5 (IQR: 17.5–67.5) months. 94 patients belonged to HCB and 75 to HUIL, with no differences in age or time on HD. The monitors used with the incorporated sphygmomanometer were Fresenius 5008 and 5008S in HCB, and in HUIL 66% were Gambro AK200 and a33% were Fresenius 5008. There were significant differences in the proportion of patients with non-filial and congenital nephropathy in favor of HUIL and vascular nephropathy in favor of HCB (Appendix A Annex Table A1). Regarding history and antihypertensive treatment, there was a higher proportion of DM, coronary artery disease, treatment with RAASI and calcium antagonists in HUIL (Appendix AA Annex Table A2). There were no differences in the proportion of patients with RRF, although the mean clearance was higher in HUIL patients (Appendix A Annex Table A3). There were significant differences in the prescription of dialysis fluid, with higher calcium and potassium concentrations in HUIL and lower bicarbonate and sodium concentrations in HUIL (Appendix A Annex Table A4).
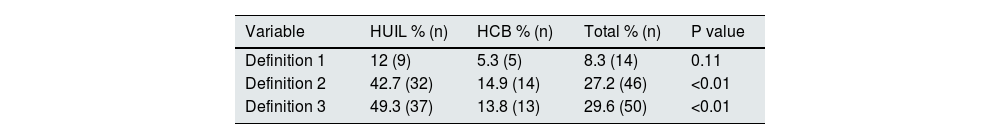
The patients identified as having IDHTN according to definition 1 (Def 1) were 14 (8.3%), according to definition 2 (Def 2) were 46 (27.2%) and according to definition 3 (Def 3) were 50 (29.6%). Table 1 shows the results separated by center, with a significant difference in definition 2 and 3, with a higher frequency in HUIL.
Comparison of patients per center according to the different definitions of IDHTN.
| Variable | HUIL % (n) | HCB % (n) | Total % (n) | P value |
|---|---|---|---|---|
| Definition 1 | 12 (9) | 5.3 (5) | 8.3 (14) | 0.11 |
| Definition 2 | 42.7 (32) | 14.9 (14) | 27.2 (46) | <0.01 |
| Definition 3 | 49.3 (37) | 13.8 (13) | 29.6 (50) | <0.01 |
HCB: Hospital Clínica Benidorm; HUIL: Hospital Universitario Infanta Leonor. IDHTN: intradialysis arterial hypertension.
Definitions 1 and 2 are based on a single similar criterion for establishing a diagnosis of IDHTN, elevated MAP and SBP respectively, and we observed that all patients diagnosed with IDHTN according to definition 1 were also included in definition 2, so that, for the subsequent analysis, we will use only the definition 2 will be used, as it is the criterion that provides the greatest sensitivity.
Assessment and comparison of the accuracy of the definitionsThe result of the sensitivity and specificity study evidences that there is a difference between the definitions (Def 1 AUC: 0.59; IC: 0.51−0.66; Def 2 AUC: 0.83; IC: 0.75−0.90; Def 3 AUC: 0.80: IC 0.72−0.87). Being definition 2 the best classifier of intradialytic hypertension, although with a non-significant difference with respect to definition 3 (p = 0.61), and definition 1 is the worst (p < 0.01) (Fig. 1).
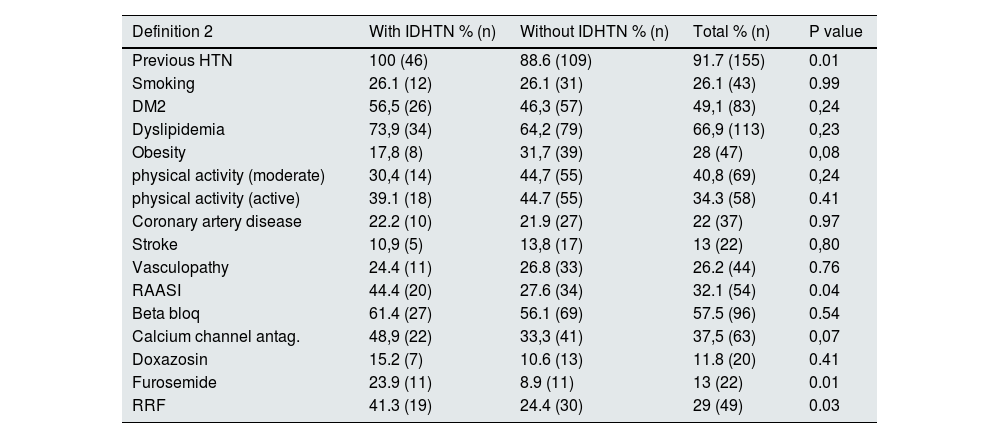
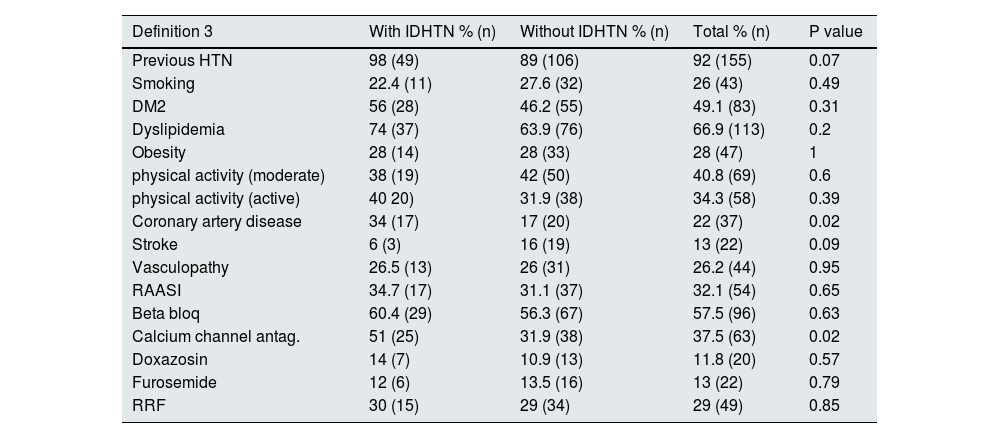
Comparison between patients with or without IDHTN according to definition 2 and 3Patients with a history of previous HTN were more likely to have IDHTN according to Def 2 (p = 0.01) and patients with a history of coronary artery disease were more likely to have IDHTN according to Def 3 (p = 0.015). No differences were found in any of the other findings of past medical history collected.
Regarding antihypertensive drugs, patients with prescription of RAASI and furosemide were more likely to suffer IDHTN according to Def 2 (OR: 2.09; 95% CI: 1.03–4.25; p = 0.039) for those on RAASI and (OR: 3.2; 95% CI: 1.28–8.01; p = 0.01) in patients on furosemide. Patients on calcium antagonists had IDHTN according to Def 3 (OR: 2.22; 95% CI: 1.13–4.38; p = 0.02). There were no differences were observed with with other drugs.
Patients with RRF presented more frequently IDHTN according to Def 2 (OR: 2.18; 95% CI: 1.07–4.47; p = 0.03). All data are presented in Tables 2 and 3.
Comparison between patients with and without IDHTN, by definition 2 (n = 46 [27.2%] and n = 123 [72.8%]) according to history, antihypertensive medication and RRF.
| Definition 2 | With IDHTN % (n) | Without IDHTN % (n) | Total % (n) | P value |
|---|---|---|---|---|
| Previous HTN | 100 (46) | 88.6 (109) | 91.7 (155) | 0.01 |
| Smoking | 26.1 (12) | 26.1 (31) | 26.1 (43) | 0.99 |
| DM2 | 56,5 (26) | 46,3 (57) | 49,1 (83) | 0,24 |
| Dyslipidemia | 73,9 (34) | 64,2 (79) | 66,9 (113) | 0,23 |
| Obesity | 17,8 (8) | 31,7 (39) | 28 (47) | 0,08 |
| physical activity (moderate) | 30,4 (14) | 44,7 (55) | 40,8 (69) | 0,24 |
| physical activity (active) | 39.1 (18) | 44.7 (55) | 34.3 (58) | 0.41 |
| Coronary artery disease | 22.2 (10) | 21.9 (27) | 22 (37) | 0.97 |
| Stroke | 10,9 (5) | 13,8 (17) | 13 (22) | 0,80 |
| Vasculopathy | 24.4 (11) | 26.8 (33) | 26.2 (44) | 0.76 |
| RAASI | 44.4 (20) | 27.6 (34) | 32.1 (54) | 0.04 |
| Beta bloq | 61.4 (27) | 56.1 (69) | 57.5 (96) | 0.54 |
| Calcium channel antag. | 48,9 (22) | 33,3 (41) | 37,5 (63) | 0,07 |
| Doxazosin | 15.2 (7) | 10.6 (13) | 11.8 (20) | 0.41 |
| Furosemide | 23.9 (11) | 8.9 (11) | 13 (22) | 0.01 |
| RRF | 41.3 (19) | 24.4 (30) | 29 (49) | 0.03 |
Act: activity; Stroke: cerebrovascular accident; beta bloq: beta-blockers; Calcium antag.: calcium channel antagonists; DM2: diabetes mellitus 2; RRF: residual renal function; HTN: arterial hypertension; IDHTN: intradialytic arterial hypertension; RAASI: renin angiotensin aldosterone system inhibitors.
Comparison between patients with and without IDTHN using definition 3 (n= [29.6%] and n = 119 [70.4%]) respectively according to history, antihypertensive medication and RRF.
| Definition 3 | With IDHTN % (n) | Without IDHTN % (n) | Total % (n) | P value |
|---|---|---|---|---|
| Previous HTN | 98 (49) | 89 (106) | 92 (155) | 0.07 |
| Smoking | 22.4 (11) | 27.6 (32) | 26 (43) | 0.49 |
| DM2 | 56 (28) | 46.2 (55) | 49.1 (83) | 0.31 |
| Dyslipidemia | 74 (37) | 63.9 (76) | 66.9 (113) | 0.2 |
| Obesity | 28 (14) | 28 (33) | 28 (47) | 1 |
| physical activity (moderate) | 38 (19) | 42 (50) | 40.8 (69) | 0.6 |
| physical activity (active) | 40 20) | 31.9 (38) | 34.3 (58) | 0.39 |
| Coronary artery disease | 34 (17) | 17 (20) | 22 (37) | 0.02 |
| Stroke | 6 (3) | 16 (19) | 13 (22) | 0.09 |
| Vasculopathy | 26.5 (13) | 26 (31) | 26.2 (44) | 0.95 |
| RAASI | 34.7 (17) | 31.1 (37) | 32.1 (54) | 0.65 |
| Beta bloq | 60.4 (29) | 56.3 (67) | 57.5 (96) | 0.63 |
| Calcium channel antag. | 51 (25) | 31.9 (38) | 37.5 (63) | 0.02 |
| Doxazosin | 14 (7) | 10.9 (13) | 11.8 (20) | 0.57 |
| Furosemide | 12 (6) | 13.5 (16) | 13 (22) | 0.79 |
| RRF | 30 (15) | 29 (34) | 29 (49) | 0.85 |
Act: activity; Stroke: cerebrovascular accident; beta bloq: beta-blockers; Calcium antag.: calcium channel antagonists; DM2: diabetes mellitus 2; RRF: residual renal function; HTN: arterial hypertension; IDHTN: intradialytic arterial hypertension; RAASI: renin angiotensin aldosterone system inhibitors.
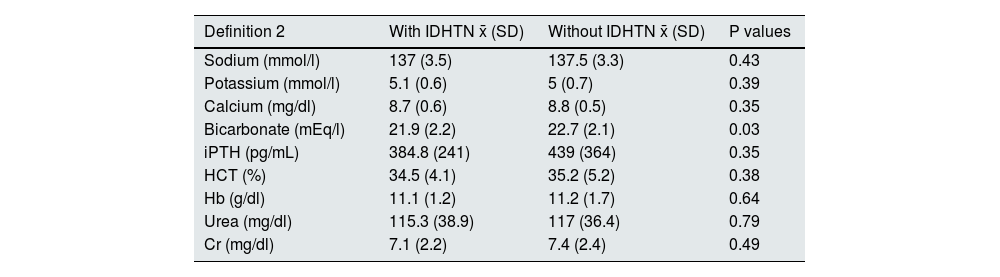
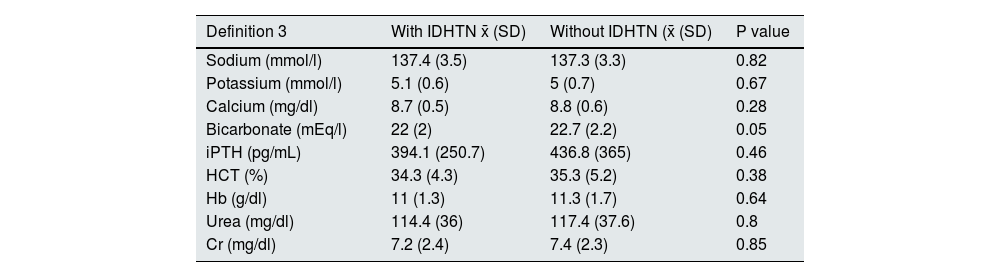
It was performed a comparison of the means of the monthly biochemical data from patients with or without IDHTN according to Def 2 and Def 3. The results shows an association of lower bicarbonate concentrations with IDHTN according to Def 2 (Tables 4 and 5).
Comparison of monthly biochemical data in patients with and without IDHTN according to definition 2: (n = 46 [27.2%] and n = 123 [72.8%]).
| Definition 2 | With IDHTN x̄ (SD) | Without IDHTN x̄ (SD) | P values |
|---|---|---|---|
| Sodium (mmol/l) | 137 (3.5) | 137.5 (3.3) | 0.43 |
| Potassium (mmol/l) | 5.1 (0.6) | 5 (0.7) | 0.39 |
| Calcium (mg/dl) | 8.7 (0.6) | 8.8 (0.5) | 0.35 |
| Bicarbonate (mEq/l) | 21.9 (2.2) | 22.7 (2.1) | 0.03 |
| iPTH (pg/mL) | 384.8 (241) | 439 (364) | 0.35 |
| HCT (%) | 34.5 (4.1) | 35.2 (5.2) | 0.38 |
| Hb (g/dl) | 11.1 (1.2) | 11.2 (1.7) | 0.64 |
| Urea (mg/dl) | 115.3 (38.9) | 117 (36.4) | 0.79 |
| Cr (mg/dl) | 7.1 (2.2) | 7.4 (2.4) | 0.49 |
Cr: creatinine; Hb: hemoglobin; HCT: hematocrit; IDHTN: intradialytic arterial hypertension; iPTH: parathyroid hormone; SD: standard deviation; x̄: mean.
Comparison of monthly biochemical data in patients with and without IDHTN according to definition 3 (n = 50 [29.6%] and n = 119 [70.4%]).
| Definition 3 | With IDHTN x̄ (SD) | Without IDHTN (x̄ (SD) | P value |
|---|---|---|---|
| Sodium (mmol/l) | 137.4 (3.5) | 137.3 (3.3) | 0.82 |
| Potassium (mmol/l) | 5.1 (0.6) | 5 (0.7) | 0.67 |
| Calcium (mg/dl) | 8.7 (0.5) | 8.8 (0.6) | 0.28 |
| Bicarbonate (mEq/l) | 22 (2) | 22.7 (2.2) | 0.05 |
| iPTH (pg/mL) | 394.1 (250.7) | 436.8 (365) | 0.46 |
| HCT (%) | 34.3 (4.3) | 35.3 (5.2) | 0.38 |
| Hb (g/dl) | 11 (1.3) | 11.3 (1.7) | 0.64 |
| Urea (mg/dl) | 114.4 (36) | 117.4 (37.6) | 0.8 |
| Cr (mg/dl) | 7.2 (2.4) | 7.4 (2.3) | 0.85 |
Cr: creatinine; Hb: hemoglobin; HCT: hematocrit; IDHTN: intradialytic arterial hypertension; iPTH: parathyroid hormone; x̄: mean; SD: standard deviation.
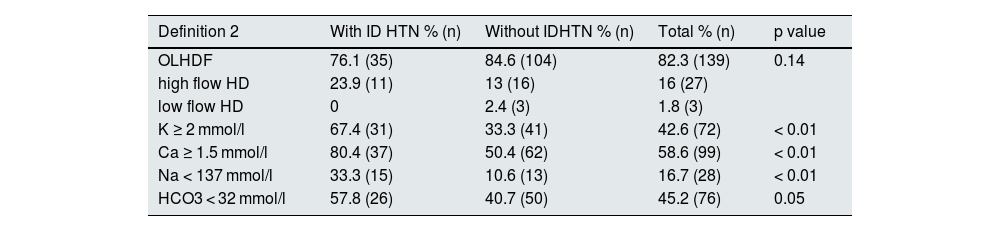
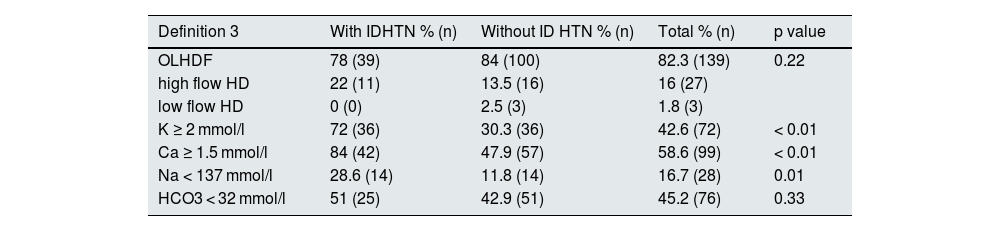
A comparison of HD parameters in IDHTN according to Def 2 shows that they are dialyzed, more frequently, with a dialysis fluid containing a sodium concentration ≤137 mmol/l, potassium ≥2 mmol/l, calcium ≥1.5 mmol/l and bicarbonate ≤32 mmol/l (Table 6). The results were similar to de observed with Def 3, except that, no differences were found in the prescription of bicarbonate in DF (Table 7).
Comparison of hemodialysis parameters in patients with and without IDHTN using definition 2 (n = 46 [27.2%] and n = 123 [72.8%]).
| Definition 2 | With ID HTN % (n) | Without IDHTN % (n) | Total % (n) | p value |
|---|---|---|---|---|
| OLHDF | 76.1 (35) | 84.6 (104) | 82.3 (139) | 0.14 |
| high flow HD | 23.9 (11) | 13 (16) | 16 (27) | |
| low flow HD | 0 | 2.4 (3) | 1.8 (3) | |
| K ≥ 2 mmol/l | 67.4 (31) | 33.3 (41) | 42.6 (72) | < 0.01 |
| Ca ≥ 1.5 mmol/l | 80.4 (37) | 50.4 (62) | 58.6 (99) | < 0.01 |
| Na < 137 mmol/l | 33.3 (15) | 10.6 (13) | 16.7 (28) | < 0.01 |
| HCO3 < 32 mmol/l | 57.8 (26) | 40.7 (50) | 45.2 (76) | 0.05 |
Ca: calcium; HCO3: bicarbonate; HD: hemodialysis; OLHDF: online hemodiafiltration; IDHTN: intradialisis arterial hypertension; Na: sodium.
Comparison of hemodialysis parameters in patients with and without IDHTN using definition 3. (n = 50 [29.6%] and n = 119 [70.4%]).
| Definition 3 | With IDHTN % (n) | Without ID HTN % (n) | Total % (n) | p value |
|---|---|---|---|---|
| OLHDF | 78 (39) | 84 (100) | 82.3 (139) | 0.22 |
| high flow HD | 22 (11) | 13.5 (16) | 16 (27) | |
| low flow HD | 0 (0) | 2.5 (3) | 1.8 (3) | |
| K ≥ 2 mmol/l | 72 (36) | 30.3 (36) | 42.6 (72) | < 0.01 |
| Ca ≥ 1.5 mmol/l | 84 (42) | 47.9 (57) | 58.6 (99) | < 0.01 |
| Na < 137 mmol/l | 28.6 (14) | 11.8 (14) | 16.7 (28) | 0.01 |
| HCO3 < 32 mmol/l | 51 (25) | 42.9 (51) | 45.2 (76) | 0.33 |
Ca: calcium; HCO3: bicarbonate; HD: hemodialysis; OLHDF: online hemodiafiltration; IDHTN: intradialysis arterial hypertension; Na: sodium.
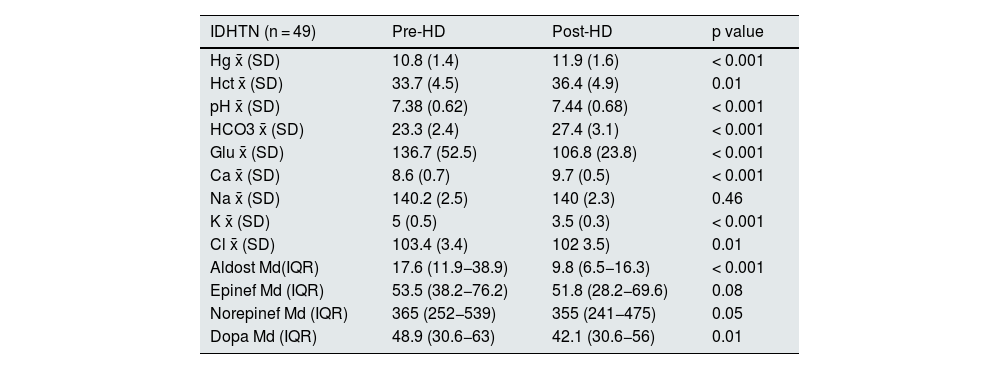
In all patients diagnosed with IDHTN it was found the biochemical changes expected in all patients undergoing HD: post-HD decrease in potassium, glucose and increase in bicarbonate, pH, calcium and hematocrit, with no changes in sodium.
It was also assessed whether there was any increase in the hormones that had a relation with potential changes in BP (dopamine, epinephrine, norepinephrine and aldosterone. It was observed a reduction in all of them, with aldosterone and dopamine changes being statistically significant (Table 8).
Biochemical and hormonal comparison before and after dialysis in patients with IDHTN.
| IDHTN (n = 49) | Pre-HD | Post-HD | p value |
|---|---|---|---|
| Hg x̄ (SD) | 10.8 (1.4) | 11.9 (1.6) | < 0.001 |
| Hct x̄ (SD) | 33.7 (4.5) | 36.4 (4.9) | 0.01 |
| pH x̄ (SD) | 7.38 (0.62) | 7.44 (0.68) | < 0.001 |
| HCO3 x̄ (SD) | 23.3 (2.4) | 27.4 (3.1) | < 0.001 |
| Glu x̄ (SD) | 136.7 (52.5) | 106.8 (23.8) | < 0.001 |
| Ca x̄ (SD) | 8.6 (0.7) | 9.7 (0.5) | < 0.001 |
| Na x̄ (SD) | 140.2 (2.5) | 140 (2.3) | 0.46 |
| K x̄ (SD) | 5 (0.5) | 3.5 (0.3) | < 0.001 |
| Cl x̄ (SD) | 103.4 (3.4) | 102 3.5) | 0.01 |
| Aldost Md(IQR) | 17.6 (11.9−38.9) | 9.8 (6.5−16.3) | < 0.001 |
| Epinef Md (IQR) | 53.5 (38.2−76.2) | 51.8 (28.2−69.6) | 0.08 |
| Norepinef Md (IQR) | 365 (252−539) | 355 (241−475) | 0.05 |
| Dopa Md (IQR) | 48.9 (30.6−63) | 42.1 (30.6−56) | 0.01 |
IQR: interquartile range; Aldost: aldosterone (ng/dl); Ca: calcium (mg/dl); Cl: chloride (mmol/l); Dopa: dopamine (pg/mL); Epinef: epinephrine (pg/mL); Glu: glucose (mg/dl); Hb: hemoglobin (g/dl); HCO3: bicarbonate (mmol/l); Hct: hematocrit (%); IDHTN: intradialysis arterial hypertension; K: potassium (mmol/l); Md: median; Na: sodium (mmol/l); Norepinef: norepinephrine (pg/mL); SD: standard deviation; x̄: mean.
After 18 months, 20 patients had a cardiovascular event (11.8%), 24 died (14.2%), 13 left HD for other causes (7.7%) and 112 remained on HD (66.3%). No significant differences were observed in any of the events studied between patients with and without IDHTN (according to Def 2 or Def 3), (Appendix Tables A5 and A6).
DiscussionThe aim of the study was to learn about a controversial and poorly-studied phenomenon, namely the increase in BP during the HD session in our units. We found a great difference in prevalence according to the center and the different definitions. We were not able to detect a profile of patient clearly susceptible to have IDHTN; their medical history, medication, biochemical tests or changes in hormones did not justify BP elevation. Furthermore in our population with IDHTN after 18-months there was no increase in mortality or a higher incidence of cardiovascular events.
One of the difficulties encountered, as described by Chazot and Jean,20 is the lack of an uniform definition. There are several definitions, taking into account an increase in MAP greater than or equal to 15 mmHg,2,4 increase in SBP greater than 10 mm HG.5,6 or any increase in BP with ultrafiltration.3,7 We have applied the 3 definitions to find out if there is any difference between them, in relation to the variables studied, at a prognostic level and if we consider one of them as a more valid test. In definition 3 we stablished a minimum ultrafiltration rate, arbitrarily, at 5 ml/kg/h to consider significant ultrafiltration.
The prevalence according to Def 1 is 8.3%, similar to other publications that use the same criteria,2,4 however, if Def 2 is used the prevalence increases greatly (27.2%), higher than other publications that place it between 5 and 15%.5,6,8 The difference found between the 2 centers is striking: 42.7% in HUIL and 14.9% in HCB. Def 3 performs in the same way, with a total prevalence of 29.59% and a significant difference between centers (HUIL 49.3% and HCB 13.8%). One explanation could be that most of the BP measurement devices connected to the available HD monitors have not been clinically validated and show variations among them,27 the existence of different monitors in the 2 units and the use of different intradialytic intervention protocols, such as the infusion of ultrapure HD fluid, the use of physiological saline, the modification of the ultrafiltration ratio or the modification of patient position, could influence the difference in prevalence.26 The absence of information about what happened between pre-HD and post-HD BP measurement could constitute a relevant confounding factor in the results. Because the initial hypothesis of the study was not to analyze differences between centers it cannot be established a reason why these differences occur, but this result underlines two aspects: the huge differences in frequency, which is already seen in the literature and the need to find a single definition that clarifies what is IDHTN.
Singh et al. performed an observational study, with a very large sample of HD patients (n = 3,198), to investigate the association between different definitions of intradialytic hypertension and long-term mortality. They used 3 definitions of intradialytic hypertension: any increase in SBP from before to after HD (Hyper0), any increase of >10 mmHg (Hyper10), and any increase of >20 mmHg (Hyper20) in ≥30% of HD sessions during a 90-day follow-up period. During the baseline period, the percentages of patients fulfilling all three definitions were 47, 21.2, and 6.8%, respectively. They confirm that the Hyper0 definition was significantly associated with an increased risk of death (HR: 1.32; 95% CI: 1.05–1.66).25 Their results suggest that IDHTN should be defined as any increase in blood pressure at the end of a dialysis session, provided that the phenomenon is not sporadic and occurs in more than 30% of hemodialysis sessions. This is a simple definition that can be easily integrated into clinical practice1; however, we consider that it may be a definition with very low specificity due to the fact that the measurement of blood pressure in HD units is not precise, mainly because the sphygmomanometers available in the monitors are not validated and patients often change their position and modify the cuff settings during the session.27
Since there is no gold standard definition for intradialytic hypertension, we have tried to find out which definition achieves the best balance between the ability to detect true positives and avoid false positives. Therefore, it was performed a sensitivity and specificity analysis with ROC curves. The result shows that there are difference between the definitions, with definition 2 being the one that best classifies intradialytic hypertension, although with a non-significant difference with respect to definition 3.
The fact that patients with IDHTN are more frequently hypertensive may suggest that there is a predisposing factor, although when Def 3 is used the difference is not statistically significant, but there is a clear tendency. These results coincide with those presented by van Buren et al.,6 therefore, it is assumed that patients with IDHTN are patients with interdialytic hypertension. The association found between a history of coronary artery disease and Def 3 would require a more specific study of this group with echocardiography in order to identify them more specifically.
The clinical appreciation that those with RRF present more frequently IDHTN has been confirmed by our results. Whether the mechanism is because they are more hypervolemic due to a reduction in ultrafiltration rate or have more intact nephro-vascular pathophysiological mechanisms that may be lost with deteriorating renal function are speculative explanations. Gunal et al. explain that the mechanism of IDHTN is the increase in cardiac output by reducing part of the vascular congestion, but without achieving the ideal dry weight, i.e., maintaining a lower congestive state increases cardiac output,3 and perhaps, in our HD units we are excessively cautious when performing ultrafiltration in patients with RRF, aiming to prevent possible renal damage due to hypoperfusion and this would explain this association. As for the patients receiving RAASI or calcium channel antagonists and furosemide, it is possibly associated with their history of HTN and preservation of RRF rather than the drugs could be the cause.
It was not expected to find any difference in the pre-dialysis analytical values between patients with IDHTN and the rest of the of HD patients, and interestingly, a significant difference on bicarbonate levels was detected in Def 2 and a trend in Def 3, but the difference found appears to have no clinical relevance. As expected the rest of the values (sodium, potassium, calcium, PTH, hematocrit) did not present differences.
In regard with the study of the DF composition, it should be taken into account that we are performing a descriptive analysis and that, in many of these patients, measures could have been taken to avoid IDHTN, for this reason, the lower sodium concentrations in DF could be a therapeutic measure without being able to determine whether or not it is an effective measure for this purpose, since this was not the objective of our study. The HD fluid pattern with calcium concentrations higher than 1.25 mEq/l has also been associated with IDHTN in both definitions. Here there could be a cause/effect association since the increase in blood calcium concentration favors cardiac contractility, thus improving cardiac output and also increases vasoconstriction22,23 which could increase the BP.
Despite the existence of several studies that relate hypertension with increased activity of SNS,24 we did not detect an increase in the neurotransmitters studied (epinephrine, norepinephrine, dopamine, and aldosterone) or in aldosterone in any of the definitions, in agreement with the study by Chou et al.4 Although we did not adjust for ultrafiltration. These results are not in favor of the traditional theory of increased BP due to stimulation of the RAS or SNS, although our sample is small.13
With regard to the events assessed at 18 months, it was not detected any association, in any of the definitions, both in cardiovascular events and mortality. There are several studies that relate hypertension with mortality; one of them, is very interesting as it comments on an increase in mortality in patients with IDHTN if pre-dialysis BP is <120 mmHg, they define IDHTN as an increase in SBP>10 mmHg5; they restricts the group of patients with IDHTNT to those that we have to pay more attention, we have not categorized patients by initial BP figures, but we understand that their results are like ours if they consider all patients with IDHTN. A second study, that has been discussed already, investigate the association between different SBP increases (Hyper0 any increase, Hyper10 an increase of 10 mmHg and Hyper20 an increase of 20 mmHg) and long-term mortality.25 Surprisingly, there was an inverse association with the risk of death (in the Hyper20 group, the risk death was lower than in the Hyper0 group). Another study does show an increase in mortality as the BP differences increases,28 but it does not evaluate each hemodialysis session, but the averages all pre-HD and post-HD blood pressures, so the difference in definition is so great that we cannot establish a comparison with our work. Further studies or continued follow-up of these patients would be required to clarify whether these patients have a worse prognosis.
Regarding the limitations of our study, firstly, it should be remembered that it is a descriptive study in which we have studied associations that do not identify causality. Secondly, we should consider that the BP recorded between the 2 HD units was performed with different sphygmomanometers and we do not have a record of what happened during the session if interventions were made that could modify the final result. Third, we did not include serum phosphorus in the study, despite it being a prognostic factor in HD patients, and we have not been able to compare the hormonal and biochemical changes that occur pre- and post-HD between patients with IDHTN versus patients without IDHTN. Finally, patients are not followed up, therefore, a survival study that would provide more information on the prognosis of these patients cannot be performed. It would be necessary to include more HD centers in order to increase the sample size and better understand differences in the population.
ConclusionOur study highlights the high prevalence of IDHTN in hemodialysis units, indicating its difficult control. However, its impact and clinical relevance have not yet been fully clarified. We believe that it is crucial to establish a single definition of IDHTN, based on the possible risks that it presents to the patient. This will allow us a better definition of the affected populations, a better understanding of its pathophysiology and the identification of the most effective treatment measures. Among the definitions considered, the most specific and sensitive is definition 2, although further studies are still required to definitively rsolve these questions.
FundingThe present research has not received specific support from public sector agencies, the commercial sector or non-profit organizations.
To Marta for her generosity in teaching and supporting me at all times, and to Maite and Fabio because without them I could not have carried out the work.