In 2007, the Quality Management Group from the Spanish Society of Nephrology proposed a system for monitoring haemodialysis with the objective of establishing a standardised protocol for implementation,1 in accordance with the KDOQI guidelines from previous years.2-5 In this context, we registered the data for our unit, which treats approximately 300 000 inhabitants, subtracting the 50% that undergo dialysis from the Spanish Red Cross, approximately 150 000 patients.
We included the information for all patients on dialysis in our hospital during 2011 in our analysis. This produced a total of 77 patients; of them, 31 were included in the study over the course of the year, yielding a final prevalence of 47 patients. The mean age was 68.07 years, 69% were male, and the treatment administered was primarily conventional haemodialysis with biocompatible filters. The distribution of renal diseases was similar to rates in previous studies, with a higher frequency of nephroangiosclerosis, diabetic nephropathy, and of an unknown aetiology, with similar percentages. We analysed the standard demographic and biological indicators related to dialysis treatment, anaemia, iron parameters, renal osteodystrophy, etc. We would also like to highlight certain characteristics of the patients who passed away, given their homogeneity.
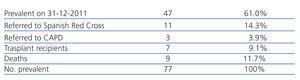
The prevalence during 2011 is summarised in Table 1.
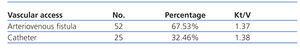
Some 30% of both prevalent and incident patients were diabetic, and 36% had a Charlson index >7. Only 3 patients underwent dialysis treatment more than 3 days per week, and none underwent less than 3 sessions per week. Gross mortality was 11.68%, with normal hospitalisation rates and duration of hospital stay. We observed positive results with permanent catheters: Kt/V (1.37)6 (Table 2) was similar to rates with fistulas. Furthermore, there was a very low rate of infections (1 bacteraemia in 22 permanent catheters in place for at least 3 months). Values for renal osteodystrophy were acceptable,7 with P<55 in 70%, CaxP<55 in 73%, and parathyroid hormone (PTH) <300 in 70%. There were no cases of PTH>800 + CaxP>55, thus no need for parathyroidectomy. All parameters for treated water and vaccinations were fulfilled without exception.8 We were satisfied that 80% of the patients starting dialysis treatment were referred from specialists and only 20% from emergency departments (pericarditis, uraemic coma, etc., and some patients that abandoned regular visits). However, we were unable to reach adequate Hb levels (11-13g/dl) in 90% of patients, as is suggested by standard guidelines. We only reached adequate Hb levels in 55% of cases. Furthermore, despite having a predialysis unit for patients with renal failure, a catheter was needed in the first session in approximately 50% of patients, not always due to the lack of an established vascular access, but rather inadequate performance by the already created vascular access in elderly patients. We also failed to comply with the recommended fistula:catheter ratio, resulting in a 3/1 value.
The most interesting results were those aspects that deviated from guideline objectives: the only patients that died were older than 80 years (mean: 85 years); except for one case, none responded to vaccination; and in more than half of all deaths, the patient left treatment several days or weeks before dying, rather than prolonging regressive situations without recourse. However, the mean duration on haemodialysis in these patients that died was 21 months, which should be taken into account when evaluating patient age upon inclusion in the programme.
No patients included in the treatment programme produced unexpected emergencies, although 2 cases occurred in patients in predialysis (pulmonary oedema) and 4 life-threatening situations were produced in previously unknown patients.
To conclude: in our experience, the positive results in permanent catheters are due to the total freedom in our unit for inserting, removing, replacing, and choosing catheters, for which we owe eternal thanks to Dr Forascepi; there is nothing like working closely with the patient to improve our results. Secondly, the few emergencies that were produced in prevalent dialysis patients were closely related to the referral of cardiologically unstable patients to peritoneal dialysis (essential collaboration from the Hospital Central de Asturias), and in some cases due to administering extra scheduled dialysis. Finally, avoiding unnecessarily prolonged treatment in certain patients with very low life expectancy and poor quality of life is an obvious goal, and we are focused on avoiding unnecessary suffering and ethical issues, etc., for heavily burdened families. In our opinion, senile patients with an acceptable quality of life should be included in this treatment programme. We need to improve many aspects of the treatment that we provide, but always with the patient’s needs in mind.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Prevalence during 2011
Table 2. Vascular access and Kt/V