To the Editor,
BK virus (BKV) has a high prevalence in the world population (> 80%). Although it does not cause disease in immunocompetent patients, it remains latent in the kidneys and urinary tract1.
Its reactivation in renal transplant recipients can lead to BKV-associated nephropathy (BKVAN). There is no specific treatment and the therapeutic strategy consists on the change of immunosuppressive drugs or dose adjustment. The correct detection and monitoring of this virus is crucial, since early intervention could prevent said disease2.
Active viral infection may be confused or coexist with cellular rejection, but they are two opposing entities, so it is essential to differentiate them.
Renal biopsy is the gold standard for BKVAN diagnosis2,3. However, real time PCR (polymerase chain reaction) makes it possible to quantify viral load and detect patients at risk for nephropathy before tissue damage occurs4,5.
Objective: To analyse the incidence of active BKV infection and the development of BKVAN in patients during their first two years after renal transplantation.
MATERIAL AND METHOD
We studied 70 kidney recipients in the Renal Transplant Unit of Dr. Julio C. Perrando Hospital; 62 of them received kidneys from cadaveric donors. Urine samples were included for BKV screening in patients who were in their first two years post-transplantation (viruria was monitored every three months during the first two years; if levels of viruria >107 copies/mL, plasma detection was performed).
Patients received induction with daclizumab/baxilzumab-methylprednisolone-mycophenolate-mofetil (MMF) and maintenance with tacrolimus-MMF-steroids.
DNAs were extracted using commercial columns (Quick-gDNA MiniPrep, Zymo Research, U.S.A.).
Qualitative real-time PCR was performed, using primers according to Randhawa et al5. Positive samples were quantified by commercial Q-PCR Alert (Nanogen Advanced Diagnostics SRL®).
RESULTS
Viruria was detected >107 copies/mL in 12 of the 70 patients (17%), but only 5 had persistent viruria, the others were transient.
Active infection was between 3 and 24 months after transplantation, with positive viraemia after 12 months.
Half the patients with viruria also suffered from renal function deterioration (creatinine > 1.4mg/dL).
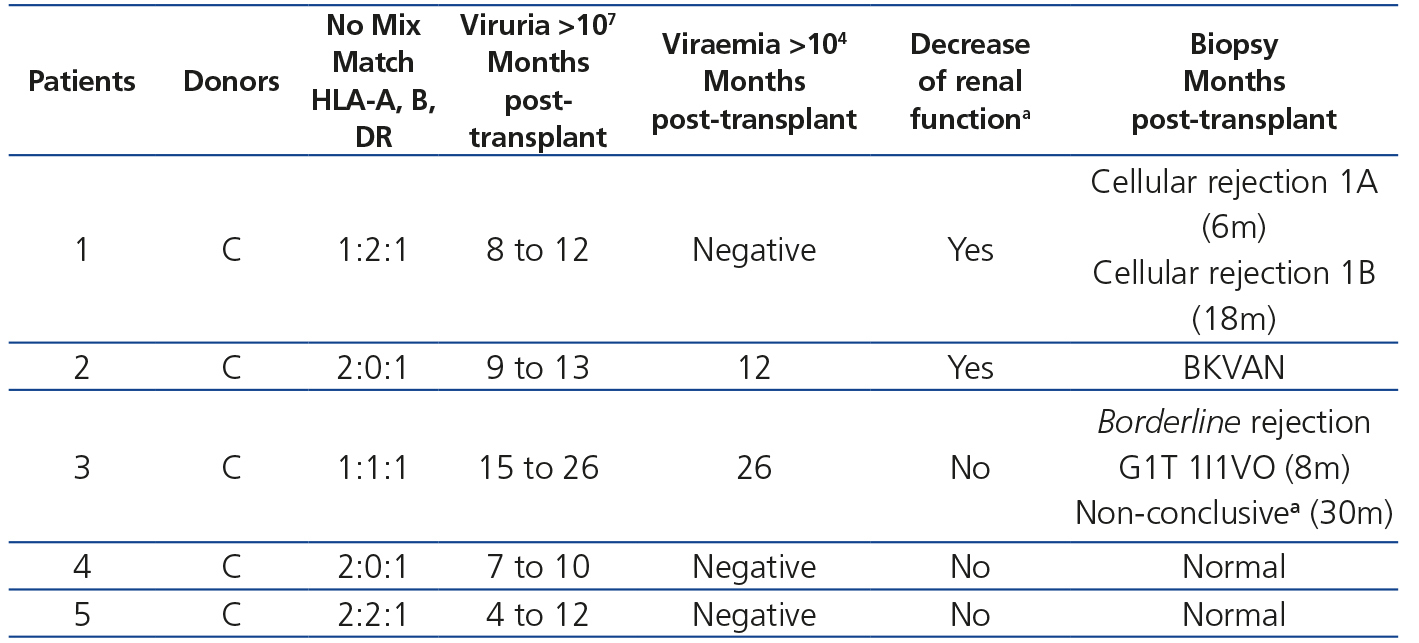
Table 1 shows the number of cases of mismatch, renal function, biopsy, viruria and viraemia in patients with persistent levels of viruria.
BKVAN was confirmed by biopsy in 1 patient, and therefore had an incidence of 1.4% in our centre.
Case report
55 year-old patient who received a cadaveric transplant. Induction: daclizumab-tacrolimus-MMF-steroids. Maintenance: tacrolimus-MMF-steroids. Creatinine 1mg/dL and 1.2mg/dL; creatinine clearance: 96mL, no proteinuria. Nine months after transplantation, the patient presented viruria (107 copies/mL) for BKV without renal dysfunction and with negative viraemia. High levels of viruria persisted with negative viraemia, which became positive at month 12 (> 104 copies/mL); biopsy findings: interstitial nephritis, tubular nuclear alterations related to BKV. The patient was switched to sirolimus 2mg/day and ciprofloxacin 500mg/day (10 days) is added. The patient maintained stable renal function values, clearance 86mL, without proteinuria and decreased viral load in blood and urine. Currently, the patient has still his kidney and does not require dialysis.
DISCUSSION
The prevalence of BKV in the urine of renal transplant patients ranges from 18%-40%: Shenagari et al.6 report 40%, Costa et al. 18,3%7 and Viscount et al. 24%4. Reactivation usually occurs within the first two months post-transplant8. In our study, we determined viral load in plasma in the 5 patients with persistent viruria, 2 had viral loads> 104 copies/mL, similar to other reports, in one patient BKVAN was found by biopsy, and the other patient had a non-conclusive biopsy. BKVAN lesions are multifocal with random distribution, and can give false negatives3.
Hirsch et al.9 monitored BKV replication during the first year after transplant, and found the highest values of viruria and viraemia (25.4% and 13.7%, respectively) 6 months after transplantation.
Babel et al.10 showed that 21.4% of patients with persistent viruria developed BKVAN between 5 and 11 weeks after reactivation in urine and blood. In our patient with BKVAN, viruria appeared 12 weeks before viraemia and this became positive almost simultaneously with biopsy findings, without clinical signs of renal dysfunction (no protocol biopsies performed in the centre).
In addition to immunosuppression, other factors such as inflammation and host immunity should be considered in the pathogenesis of BKVAN.
CONCLUSIONS
The positivity of PCR in urine may be the first finding indicative of BKV reactivation. In our patient, screening determined a significant and persistent viral load in urine 12 weeks before viraemia, which could be an advantage for early detection of reactivation and allow adjustment of immunosuppression, although viraemia is more strongly associated with the development nephropathy. The data reported are useful, since so far no literature has been published on the incidence of BKV reactivation in renal transplantation in Argentina.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Number of cases of miss match, viruria, viraemia, renal function and biopsy in patients with active infection due to BK virus