Dear Editor,
Requesting diagnostic tests that are easy to perform and interpret is extraordinary important for rapid diagnosis of serious diseases.
We present a 61 year old patient, ex smoker, with Arterial Hypertension (AHTN), diabetes mellitus type 2, dyslipidaemia, with a pacemaker for sinus node dysfunction, intermittent claudication and aortic valve disease, carotid stenosis and treated ischaemic heart disease. The patient is referred for external consultation to test for chronic renal failure with creatinine 1.56mg/dl (ClCr by MDRD 48ml/min.) No significant nephrourologic antecedents.
Physical examination showed right carotid murmur, weak popliteal pulse and lack of tibial and dorsalis pedis pulses as pathological findings. The blood count showed normocytic-normochromic anaemia (Hb 10.4mg/dl; MCV 91fl; MCH 30.6pg; and MCHC 31g/dl.) In the plasma biochemistry, potassium was 3.7mEq/l. Venous blood gas tests found plasma alkalaemia (pH 7.461) due to metabolic alkalosis (CO3H 29.5mEq/l), with adequate respiratory compensation (pCO2 measured 42.3mmHg, with PCO2 estimated at 43.85 ± 2mmHg.) Ultrasound showed kidneys of normal aspect and size.
The presence of generalised vascular disease, ATHN and metabolic alkalosis, which was inadequate for the patient’s level of renal function, led to the suspicion of the presence of renovascular AHTN. A renal arteriography was requested previous infusion of 2000cc of 0.9% saline serum in 24 hours (to prevent contrast-induced nephropathy), leading to hypokalaemia (2.9meq/l) with no electrocardiographic changes.
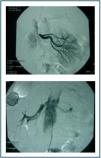
The arteriography detected stenosis in both renal arteries (figure 1), which was corrected with angioplasty and stent.
Renovascular arterial hypertension is one of the most common causes of secondary arterial hypertension and early diagnosis is important since it is a potentially reversible disorder. The incidence of this disorder is lower than 1% in patients with slight AHTN.1 However it is between 10-45% in serious or malignant AHTN.2
The presence of AHTN, metabolic alkalosis and hypokalaemia should lead to the suspicion of the existence of an excess of mineralocorticoids.3 In such cases, hypokalaemia only appears in 50% of cases,4 but it may be shown by the administration of sodium and water either with oral sodium chloride for three days (urinary sodium > 200mEq/24 hours to verify adequate overload)6 or 2 litres of isotonic solution for four hours,7 controlling arterial hypertension and hypokalaemia if present, and evaluating the risks of sodium overload. Increased distal flow and hyperaldosteronism increased the elimination of potassium.5
The elimination of alderosterone in urine > 14μg/24 hours6 and the concentration of plasma alderosterone > 10ng/dl7 will confirm the diagnosis.
The correct interpretation of simple diagnosis tests, such as venous blood gas in a proper clinical context and the provocation of hypokalaemia with the administration of sodium, very suggestive of hyperstimulation of the renin-angiotensin-aldosterone system are very useful in diagnosing patients with renovascular arterial hypertension.
Figure 1.