Introduction: Chronic kidney disease (CKD) affects the daily life of the child especially during the stage where their personal development takes place. Adult renal patients have a demonstrated worse health related quality of life (HRQL) mainly under hemodialysis (HD), however there are few published data about HRQL in children with CKD, most of them obtained after patient´s childhood or with generic tests that do not discriminate changes in a specific disease. Objetive: To assess how our patients perceive their health by measuring the HRQL and its most affected domains. To determine how the different therapies affect the child with CKD and the agreement on the opinion between children and their parents. Material and methods: We included 71 CKD children and their parents in a cross-sectional study ( 33 transplanted, 11 peritoneal dialysis [PD], 5 HD, 22 conservative treatment). We used a specific quality of life test for CKD children that we had previously developed (TECAVNER). If the child was younger than 9 years, only their parents completed the survey. Results: Children on HD refer a worse HRQL followed those who underwent PD and those transplanted. The best HRQL was obtained in children with conservative treatment. Both parents and children agree
that the domains more frequently affected are physical activity and school attendance especially those on HD. The way the adolescents 15 years and older perceived their health was similar to that of their parents. This was not the case in the younger group, 9 through 15 years.
Introducción: La enfermedad renal crónica (ERC) modifica la vida del paciente y afecta de manera especial a los niños en su etapa de desarrollo personal. En adultos se ha demostrado peor calidad de vida relacionada con la salud (CVRS), sobre todo en hemodiálisis (HD); sin embargo, hay muy pocos datos objetivos sobre CVRS en niños con ERC, la mayoría obtenidos una vez superada la infancia de estos enfermos o con cuestionarios genéricos que no permiten discriminar cambios en una enfermedad específica. Objetivos: Conocer cómo perciben nuestros pacientes su estado de salud midiendo la CVRS y sus áreas más afectadas. Determinar la influencia de los distintos tratamientos y la concordancia entre la opinión de los niños y de sus padres. Material y métodos: Estudio transversal en 71 niños (33 sometidos a trasplante, 11 en diálisis peritoneal, cinco en HD y 22 en tratamiento conservador) y en sus padres. Utilizamos un cuestionario específico desarrollado por nosotros para la medida de CVRS en niños con ERC. En los menores de 9 años sólo contestaron los padres. Resultados: Los niños en HD refieren una peor CVRS, seguidos de los pacientes en diálisis peritoneal (DP) y de los sometidos a trasplante (TX), y la mejor CVRS se obtiene en los pacientes sometidos a tratamiento conservador. Los aspectos que más se ven alterados son la actividad física y la asistencia escolar, sobre todo en HD, hecho en el que coinciden padres e hijos. La concordancia entre padres e hijos fue buena en los mayores de 15 años, existiendo discordancia en los niños de 9 a 15 años.
INTRODUCTION
Chronic kidney disease (CKD) diagnosed in childhood will persist through and change the patient’s entire life.1 Children must become dependent on family for their care and the hospital for the periodic revisions that are usually very frequent. They are subjected to blood draws, must follow a diet which restricts certain foodstuffs and sometimes liquids and take a variety of drugs several times a day. Furthermore, they exhibit symptoms such as loss of appetite and delayed sexual maturity. They must change and adapt their everyday life and learn to live with the disease in an already complicated stage of life in which development into adulthood takes place.1 The aspects which most concern children are growth and physical appearance, with the additional burden of dedicating time to medical controls and hospital admissions with the consequent disruption to normal life, physical, school and social activity. While quality of life (QL) in adults with CKD is well studied,2,3 the QL in children with kidney disease is rarely objectively measured; the majority of studies are limited to adolescents and use measuring instruments specific to adults with kidney disease or generic health related QL (HRQL) scales not specific to kidney disease.4,5 In a previous study, we studied the QL of our patients with the MOS-SF-206 generic questionnaire. We found that patients on haemodialysis (HD), in general, have a worse QL than those on peritoneal dialysis (PD), in conservative treatment or who are transplant (TX) recipients. Since generic scales are not appropriate for measuring changes within a specific disease, nor differences between the different treatments applied (HD, PD, TX), we examined the need to develop a specific questionnaire for children with CKD and to be able to study HRQL in our population; up to now there has been no such instrument for this population in Spanish. This questionnaire is described in detail in an attached study. Goldstein’s group is currently working on a specific questionnaire in English DP.5 Nowadays, numerous scientific and therapeutic advances are available, but resources used in the psychological support of patients and their families are still few. The aim of our study was to measure the HRQL of children with CKD, understanding this as a multidimensional concept which refers to how patients perceive and react to their state of health and includes physical, psychological and social well-being.8,9 We also wanted to define the most affected areas and how they are influenced by the distinct treatments employed, to allow us to intervene and, therefore, improve their QL, helping them to live with their disease and reducing their limitations, ultimately accompanied by the recuperation of their desire to live and dream.10,11
MATERIAL AND METHODS
Transversal study whose accessible population was children seen in the Children’s Nephrology Section of the Gregorio Marañón University Hospital (Madrid) included 71 CKD patients (more than 3 months of evolution), 22 in conservative treatment, 33 carrying a kidney graft and 16 in replacement treatment: 11 on PD and 5 on HD. All patients participated voluntarily in the study, giving consent for inclusion after previous verbal explanation. We used the QL questionnaire specific to children with kidney disease (TECAVNER) developed by us and described in detail in an attached study.7 It consists of 14 domains. It has a reliability of 0.92 using Cronbach’s coefficient alpha. Its main limitations stem from not having undergone the testretest nor construct validity. It is answered by children older than 9 years of age and their parents independently, and by only the parents of children under 9. Data collected were: a) sociodemographic variables: age, civil status, education and working situation of parents, social level, type of housing, number of siblings, job situation in working-age patients, education and school delay and, b) clinical data: age of patients, age at disease onset and its evolution time, baseline diagnosis of the disease and current treatment type. In the statistical analysis, the description of quantitative variables is expressed as mean and standard deviation (SD) and qualitative variables as a percentage or frequency. A simple or bivariant analysis was done to demonstrate associations, using the χ2 test for qualitative variables and, where that was not possible, the Fisher exact test. To compare the means of independent groups, the non-parametric version of ANOVA (Kruskal-Wallis) was used when the sample was less than 30 or the variances were not homogeneous. We determined the reliability of the questionnaire using Cronbach’s coefficient alpha. Concordance between the answers of children over 9 with their parents’ answers has been analysed using the intraclass correlation coefficient with its ICC at 95%. This coefficient is used to determine agreement between two distinct groups which use the same scale. Values over 0.9 indicate excellent agreement and values of 0 indicate total disagreement.
RESULTS
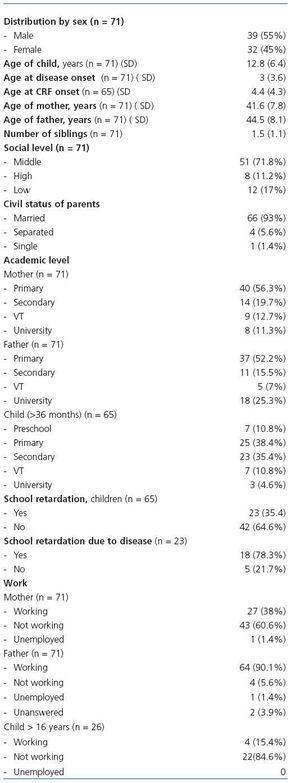
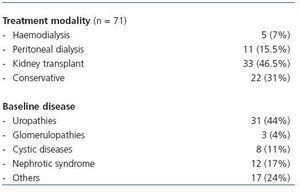
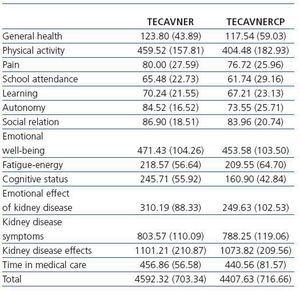
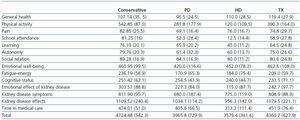
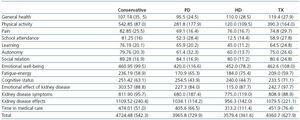
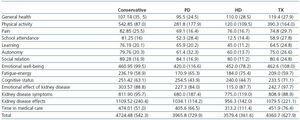
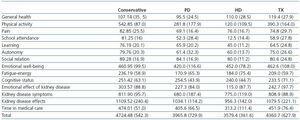
Tables 1 and 2 show the sociodemographic data, baseline disease and treatment, education, school delay and academic level, number of admissions and days of admission in the previous 6 months. Of the 71 children in the study, 42 were older than 9 years and, of them, 11 were receiving conservative treatment, 4 were on PD, 2 on HD and 25 were renal transplant carriers. Tables 3 and 5 detail the overall results and according to treatment type of the TECAVNER questionnaire, answered by the children over 9 years, and the TECAVNERCP, answered by parents of all children regardless of age. The questionnaire has good internal consistency, with a Cronbach coefficient alpha of 0.925 when answered by children and 0.915 when answered by parents. To determine concordance or agreement between parents and children, we divided them into 3 age groups. There was no concordance in any domain of the test in children between 9 and 12 years and only in social relationship in children from 12 to 15, with an ICC of 0.71. Concordance was obtained, however, between parents and children in the older group (over 15 years) in physical activity, pain, school attendance, learning, emotional well-being, fatigue-energy and effects of kidney disease with an ICC higher than 0.7 and, therefore, good. In Table 3 a slightly lower score across all domains stands out in the questionnaires answered by parents in relation to those answered by their children, the main differences being in the domains of physical activity (404-459), cognitive status (160-245) and emotional effect of the kidney disease (249-310). The distinct domains are affected to a greater or lesser degree according to the treatment modality. The children reflect significant differences between HD and TX or conservative treatment (Tables 4 and 6) in physical activity, school attendance, social relation, symptoms of kidney disease and total QL. Physical activity (HD 150.0 against conservative treatment 490.9; p 0.013) (HD 150.0 against TX 492.0; p 0.01); school attendance (HD 12.5 against conservative treatment 75; p < 0.01) (HD 12.5 against TX 67; p < 0.01); social relation (HD 50.0 against conservative treatment 90.9; p 0.01) (HD 50.0 against TX 89.0; p 0.017); total quality of life (HD 3353.2 against TX 4663.34; p 0.044) (HD 3353.2 against conservative treatment 4776.3; p < 0.034). Kidney disease symptoms are more conspicuous in HD and PD than in conservative treatment or TX (HD 562.5 against conservative treatment 813.6; p < 0.01) (HD 562.5 against TX 835.0; p < 0.01) (PD 700.0 against TX 835.0; p 0.041). Although there are no significant differences in learning, fatigue-energy, cognitive status, emotional effect of the kidney disease and time dedicated to medical care, those on haemodialysis are in a worse situation. Only in general health and autonomy do patients on PD have worse scores than patients on HD. As far as pain, patients on HD mention less intensity while being very similar across the three remaining groups, although somewhat higher in those subjected to transplant. Overall QL mentioned by the children (Table 4) is worse in HD, followed by PD and then TX and conservative treatment with very similar scores. Parents’ answers regarding the QL of their children are shown in the scores of Table 5. There are significant differences according to the established treatment in the domains covering physical activity, school attendance, learning, emotional effect of kidney disease, symptoms of kidney disease, time dedicated to medical care and total quality of life, with a better HRQL seen in conservative treatment. Physical activity (conservative 542.85 against TX 390.32; p < 0.01) (conservative 542.85 against PD 281.81; p < 0.023) (conservative 542.85 against HD 120.00; p < 0.01). School attendance (conservative 81.25 against TX 58.87; p 0.011) (conservative 81.25 against PD 52.27; p < 0.01) (conservative 81.25 against HD 12.50; p < 0.01). Learning (conservative 76.19 against HD 45; p 0.03). Emotional effect of kidney disease (HD 115.00 against conservative 303.57; p < 0.01) (HD 115.00 against TX 242.74; p 0.028). Symptoms of the disease (PD 680.00 against conservative 811.90; p 0.017) (PD 680.00 against TX 808.87; p 0.013). Time dedicated to medical care (HD 313.20 against conservative 474.01; p < 0.01) (HD 313.20 against TX 808.87; p < 0.01). Total quality of life (conservative 4724.48 against PD 3965.83; p 0.023) (conservative 4724.48 against HD 3579.43; p 0.019). The domains of autonomy and effects of kidney disease are better for patients in conservative treatment, followed by TX and PD, and worse for those on HD. Patients subjected to TX have better general health and those on PD, worse. Those subjected to PD also suffer more intense pain, followed by those subjected to TX, HD and conservative treatment (Table 7). In general health, children who have received TX obtain a better score, while those on HD and, especially, those treated with PD, express a worse state of health.
DISCUSSION
An individual’s QL is the perception that person has of his or her own life and circumstances and is influenced by both objective and subjective factors; among these, the individual’s expectations and social and family surroundings play a fundamental role. The HRQL measures the impact of the disease on the individual and its consequences from a physical, social or psychological point of view. Children have generally been thought incapable of answering questions on their own QL and, therefore, the majority of studies have been based exclusively on the opinion of the parents. However, the perception of children and their parents is not necessarily the same and how children feel about their own disease and treatments should be taken into account. We believe, therefore, that any current QL evaluation in children should include their opinion. Although paediatric nephrologists have always been sensitive to the child’s adaptation to CKD, the absence of specific methods to measure QL at this age has made its study difficult. In a recent study, McKenna et al.4 compare the QL of 59 children with CKD (27 subjected to TX, 12 on dialysis and 20 in conservative treatment). They set out from the hypothesis that QL is worse on dialysis but find that education and emotional state are better on dialysis than in children subjected to TX, although without significant differences. As they themselves point out, the use of the PedsQL questionnaire may not discriminate between different treatments since it is a generic questionnaire not specific to kidney disease. The generic questionnaire has allowed them to compare healthy children to children with CKD and they have found the expected differences, with worse QL in the sick children. Another very recent Spanish study, conducted by Riaño-Galán et al.,12 also with a generic questionnaire (CHIP-AE), studied the QL of 81 adolescents with kidney disease (68 subjected to TX and 13 on dialysis), comparing them to the healthy population. Those subjected to dialysis, PD and HD, mention less satisfaction with their health than healthy people and those subjected to TX; the
differences between PD and HD are not studied, and no differences are found between transplant recipients and the healthy population.12 In our group’s previous study on the same patient population, with the generic MOS-SF-206 questionnaire, we also found that perceived QL is better in healthy children than in sick, above all in terms of physical function, perception of health and overall QL. In contrast to the Riaño-Galán group, we did find a tendency for a worse QL in those who underwent TX than in the healthy population; this difference may be due to the application of different questionnaires. According to treatment modality, we found differences between HD and the other treatments, improving in PD, conservative treatment and TX, these last two groups expressing better QL. With our TECAVNER questionnaire for children with kidney disease, we find better scores and, therefore, better QL, during conservative treatment or TX than in children on dialysis. This finding is also evident in adults, where there is also a difference between PD and HD.13 The involvement of the different areas of QL over the 14 TECAVNER domains is very similar in TX and conservative treatment, and clearly worse in almost all the domains in children on HD. These children mention greater change in physical activity, school attendance, learning, social relation and emotional well-being. This is probably related to the hours spent in dialysis sessions, which prevents them from having adequate schooling and results in low academic achievement, poor learning, less physical activity and fewer possibilities for entering into social relationships or establishing friendships in school, which may explain their worse emotional state. Similar results were obtained by Gerson et al.14 when they analysed the state of health of 113 adolescents with CKD. They found that dialysed patients showed worse state of health, without differentiating between PD and HD, with greater limitations to physical activity, while those subjected to TX were more satisfied with their state of health, as occurred in our patients. It was striking to us that children on HD mentioned less pain than on other treatments in spite of the fistula puncture three times a week. We may be able to explain this by the routine application in our service of a topical anaesthetic prior to the puncture or by adaptation to repeated punctures. The parents’ assessment of their children’s QL coincides with theirs in that the greatest effect is on physical activity, school attendance and learning with worse QL in HD, followed by PD and then TX, with better QL in conservative treatment. We see that the parents’ perception of overall HRQL is worse than their children’s across all treatment modalities except HD. Parents, therefore, underestimate the QL of their children, as McKenna et al.4 also found. Concordance of opinion between parents and children depends on the children’s age. We found no agreement in any domain in children under 12 years. Between 12 and 15 there is concordance only in the social relation domain (0.71 ICC), while in those over 15 years there is concordance in more domains: physical activity, pain, school attendance, learning, emotional well-being, fatigue-energy and effects of kidney disease (> 0.70 ICC). The difference in perception we observed between parents and children has been documented previously, in relation to behaviour as well as emotional problems.15,16 A slight correlation has been demonstrated (0.28 ICC) between different caregivers such as parents, teachers, observers and companions and between the children and their parents (0.22 ICC).17,18 The discrepancy, rather than a problem, is an option. The opinions of parents and children can be evaluated in different ways: a moderate correlation is mutually validating, a weak correlation makes us doubt the validity of one of the measurements and if it is high, the parents’ score could be used to substitute the opinion of the children who are incapable of providing good information due to age or state of health. Furthermore, discrepancies may indicate a change in communication between parents and children and signal the need for psycho-social intervention. However, it is not always low concordance that is a sign of problems: a broad coincidence between the perception of parents and children may be a sign of failure to reach the level of autonomy and free-thought that the child should be developing.19 There appear to be two common facts: a) even when concordance between children and parents is high, it is far from being perfect, and b) parents generally believe their children have more problems and worse QL than perceived by the children themselves.20-22 In our study, we see there is no concordance between parents and children under 12 years, but improves as children get older. This finding increases the validity of our questionnaire which can detect the discrepancies that exist between parents and children and which reflects the bibliography.15-22 If the correlations between parents and children are very low, how do we establish the values that are not valid? One approach would be to simultaneously administer other questionnaires or another independent measure. If the correlations with other measures are moderate and the children have worse responses than the parents, it could be an indication that there are problems in the validity of the parents’ scale. Another means of evaluation would be through guided, qualitative interviews that help to determine the reason for the discrepancies.20 The fact that both children and their parents consider HD and PD worse QL options, in spite of great progress in dialytic techniques, convinces us that the treatment of choice for children with terminal kidney disease is TX which allows the child to develop adequately and improves his or her QL.5 TX has many advantages: it avoids vascular access, improves the state of nutrition, lifts the restriction of liquids and diet and improves psychosocial development. TX enables the child to lead a normal life with regular school attendance which improves his or her education and the possibility of securing work in adult life.23 Our patients, with normal intellectual capacity, are held back at school by the disease because of the absences caused by consultations and frequent admissions. The school system is unable to offer support in spite of having teachers in the hospital to help them with their studies. This is demonstrated by the poor results, school attendance and learning of children on HD and this issue should be a priority for dialysis and TX teams. Another important factor is that TX allows children to have far more independence from their parents than children on PD. The majority of TX recipients mention being satisfied with their life and think their health is excellent or good. Some studies in adults show no more stress than in the healthy population, finding only greater difficulties in the area of personal or partner relationships.24 The choice of adequate replacement treatment has a fundamental role in the rehabilitation of the child in adult life. Finishing school, finding a secure job and becoming independent from parents and establishing stable adult relationships can all be favourably influenced if the child receives a functioning TX and avoids prolonged dialyses. We should consult the child and his or her family before deciding the best treatment to improve QL given their environment.25 Many young adults who develop CRF in childhood experience a number of problems in achieving full rehabilitation. Some are medical problems like cataracts, osteoporosis or aseptic necrosis; others are social and derive from the need for chronic medical treatment, fear of rejecting the graft and the possibility of going back on dialysis. With this study we contribute new data not previously evaluated with generic questionnaires, including the two previous studies carried out in Spain.6,12 We have been able to demonstrate how HRQL is affected according to the treatment modality employed, and we differentiate HD from PD (not done by Riaño-Galán’s group), QL in the HD group being clearly worse in the opinion of both parents and children, improving with kidney TX or conservative treatment. Furthermore, we have determined some of the areas most affected specifically by kidney disease and its treatment, such as physical activity, education and learning, that are not evaluated in the previous studies6,12 which use a generic questionnaire. It should be taken into account that these areas are crucial in child development: less learning and a worse education will encumber integration into adult life. Moreover, the reduction of physical activity implies a sedentary lifestyle with greater morbidity and mortality and emotional effects because of the difficulty of integrating into society. With the development of this questionnaire, new lines of investigation are opened which will allow us, preliminarily, to determine differences in QL caused by analytic and clinical parameters such as anaemia, albumin, short stature and arterial hypertension, which is what we are currently working on. Our study, as it is carried out in only one centre in Spain, is limited by having only a small number of patients, above all on HD and PD, to which we must add the range of ages. We believe it is vital, therefore, for this study to be disseminated so that a national, multicentre study can be conducted which reveals the HRQL of Spanish children with CKD. In future multicentre studies, a construct validation and the testretest of the TECAVNER questionnaire will be done, which would confirm its validity. This being the only questionnaire in Spanish specifically for children with CKD it could have practical use in other Spanish speaking populations.
SUPPORTING SUMMARY
1. What is known of the issue?
The quality of life of adults with chronic kidney disease is affected, to a large extent, by the kind of treatment followed, and is worse with haemodialysis. The few studies that have been conducted on the quality of life of children with chronic kidney disease have been done with generic questionnaires which allow them to be compared to healthy children but do not discriminate variables in a specific disease. No studies have been published which use questionnaires specifically for children with kidney disease and which evaluate the influence of treatment type in chronic kidney disease.
2. What contribution does the study make?
The study provides data on health related quality of life in children with chronic kidney disease in the different treatment modalities. Comparisons are made between modalities and the most affected quality of life areas are reflected. A comparison is also made of the data collected from children with data collected from parents to evaluate concordance of perceived quality of life between parents and children in different treatments.
Table 1. Sociodemographic data
Table 2. Clinical data
Table 3. Results of TECAVNER (children) and TECAVNERCP (answered by parents)
Table 4. TECAVNER according to treatment modality (children over 9 years)
Table 5. TECAVNERCP according to treatment modality. Parents opinion
Table 6. TECAVNER in children. Statistical significance by treatment
Table 7. TECAVNERCP. Statistical significance by treatment