Lupus anticoagulant-hypoprothrombinaemia syndrome (LAHS) is a disorder characterised by the acquired deficit of coagulation factor II (prothrombin) together with the presence of lupus anticoagulant. It is an extremely rare syndrome (less than 100 cases described in the literature),1 in which there is a predisposition to bleeding, unlike antiphospholipid syndrome (APS), which is characterised by an increased risk of thrombosis.
The first case was described by Rapaport et al.2 in 1960, but it was not until more than 20 years later that the study be Bajaj et al.3 demonstrated the presence of anti-prothrombin antibodies. Although these antibodies do not impede prothrombin activity, they lead to secondary hypoprothrombinaemia due to rapid clearance of the antigen–antibody complexes from the circulation.
The most common treatment of LAHS consists of steroid therapy together with other immunosuppressors (cyclophosphamide, azathioprine, or rituximab). The aim of treatment if to reduce the risk of bleeding and eliminate prothrombin inhibitor.4
We present the clinical case of a 37-year-old Bulgarian man, with a history of lupus nephropathy diagnosed in his country in 2004. Despite receiving treatment, he had a poor clinical course, requiring renal replacement therapy 7 years after diagnosis. Two years later, he attended our hospital to continue haemodialysis. He was assessed by the rheumatology team and the haematology team for chronic thrombocytopenia, for which he received immunosuppressive treatment with steroids, immunoglobulins, and rituximab, as well as thrombopoietin-receptor agonists (eltrombopag), with a poor response. He also had APS and was positive for anti-cardiolipin antibodies and anti-β2-microglobulin antibodies. This presented with several thrombotic events (thrombosis of several vascular access devices) and a cerebrovascular event in 2014, for which he had been started on anticoagulant treatment.
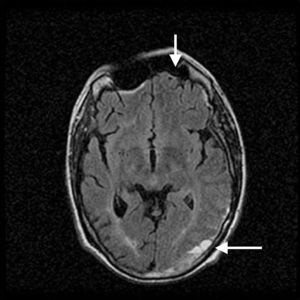
The patient was admitted to our department for an episode of general malaise and low-grade fever in the context of a possible central venous catheter bacteraemia. He started broad-spectrum antibiotic treatment with a clear clinical improvement, and it was decided to stop anticoagulation temporarily to allow a change of venous catheter. During this period of withheld anticoagulation, he experienced a transient ischaemic attack which presented as right-sided paraesthesia and reduced power, with expressive aphasia. It was therefore decided to re-start anticoagulation with heparin sodium. Surprisingly, brain magnetic resonance angiography showed, along with old ischaemic lesions, a significant subdural haematoma at the left cerebral convexity with mass effect in the parieto-occipital region (Fig. 1). Between the neurosurgery and neurology teams, it was decided to stop anticoagulation and wait and see how he progressed clinically and radiologically. Given the presence of thrombotic and haemorrhagic events, a new coagulation study was requested. This showed lupus anticoagulant, elevated levels of anti-cardiolipin antibodies and anti-β2-microglobulin antibodies, and low coagulation factor II (prothrombin) activity, which corrected with mixing, confirming the presence of lupus anticoagulant-hypoprothrombinaemia syndrome (Table 1).
Clotting factor activity with and without correction for lupus anticoagulant.
| Factor | Factor activity (%) | Corrected factor activity (SynthAFax®) (%) | Mixed factor activity (%) |
|---|---|---|---|
| Factor II | 25 | – | 70 |
| Factor V | 102 | – | – |
| Factor VII | 136 | – | – |
| Factor X | 114 | – | – |
| Factor VIII | 16 | 83 | – |
| Factor IX | 6 | 96 | – |
| Factor XI | 8 | 94 | – |
| Factor XII | 7 | 98 | – |
Combined treatment was started with anticoagulation and immunosuppression with low dose steroids, mycophenolic acid, and rituximab 6-monthly.
The association of lupus anticoagulant with hypoprothrombinaemia is a rare syndrome, infrequently described. It is a syndrome that is more common in children and young adults, and is commonly associated with viral infections and auto-immune diseases (above all systemic lupus erythematosus), although cases have also been described in association with drugs or tumours.1 LAHS is usually self-limiting when associated with viral infection, whereas in those associated with auto-immune diseases, relapse is common despite treatment.
It is clinically characterised by haemorrhagic diathesis, with epistaxes and ecchymoses being the most common types of bleed, although cases have been described of haematuria, gastrointestinal bleeding, and intracranial haemorrhage, amongst others5 Several cases have been described of LAHS with associated thrombosis, in some cases multiple thromboses. However, those cases were mainly in the context of starting treatment against prothrombin inhibitor.
Treatment of LAHS is based on immunosuppression to avoid haemorrhagic events and to try to eliminate factor II-inhibitor.4 An increase in thrombotic events has been described in patients with LAHS, as immunosuppression reduces inhibitor levels, but not lupus anticoagulant levels.5 There are no guidelines indicating what the best treatment is for LAHS, most treatment being based on corticoids with another immunosuppressor.
In conclusion, in patients with lupus nephropathy with both thrombotic and haemorrhagic processes, lupus anticoagulant-hypoprothrombinaemia syndrome must be suspected. Diagnosis and treatment-based on immunosuppression to control the clinical manifestations of the disease are essential.
Conflicts of interestThe authors declare that they have no potential conflicts of interest related to the contents of this article.
Please cite this article as: Carreño-Tarragona G, Morales E, Jiménez-Herrero MC, Cortés-Fornieles E, Gutierrez E, Praga M. Síndrome de anticoagulante lúpico-hipoprotrombinemia: una extraña asociación en el lupus eritematoso sistémico. Nefrologia. 2016;36:186–188.