Dear Editor:
The incidence of renal affectation in Systemic Sclerosis (SSc) is difficult to establish, because in the early stages and in its milder forms, the manifestations may be subclinical, and they may coincide with other pathologies, given the disease’s long evolution. We distinguish between three types of nephropathy: acute, chronic and overlap syndrome (associating scleroderma and other rheumatic illnesses).1-2
Clinical case
Male patient, aged 36 years with a history of SSc since 2000, bipolar disorder, terminal ileitis, consumer of alcohol and marijuana.
Underwent treatment with D-penicilamine for the SSc for several years, which was discontinued a year ago due to gastric distress. Usual treatment: nifedipine, deflazacort, lithium and olanzapine.
In January 2008, the patient was referred for renal failure (RF) study, due to recent presentation of plasma creatinine at about 2mg/dl, proteinuria 300mg/dl and hypoalbuminaemia 2.36g/dl.
Physical examination showed limited flexion of the fingers; the rest was normal. BP: 123/76mmHg.
Analytical tests showed: haemoglobin, 11.5g/dl; urea, 138; creatinine, 4.2; cholesterol 157mg/dl. Total proteins, 5.4; albumin 2.6g/dl. PTH, 119pg/mml. Widespectrum immunology screen negative except for ANCA-anti-MPO+. Proteinuria, 4.2g/día; sediment, 1,042 red blood cells per high-power field. Creatinine clearance 25ml/min. In studies prior to 2000, anti-scl 70 and ANA+ were prominent. The ultrasound showed kidneys measuring 11.5cm with an increase in cortical echogenicity.
Given the presence of RF and proteinuria in the nephrotic range, we started treatment with ramipril and recommended discontinuing the lithium.
15 days later, the patient came to the Emergency Room with nausea, vomiting, and abdominal pain that had been evolving over several days.He presented a lithaemia of 4.4 mEq/l,; crp 5.8; urea 178mg/dl. Hydration treatment was started, despite the fact that it increased lithaemia; for this reason, the patient underwent emergency haemodialysis. In subsequent checks, the lithaemia was below 1.5meq/l, so it was not necessary for him to undergo additional haemodialysis sessions.
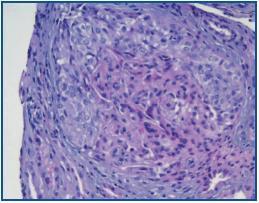
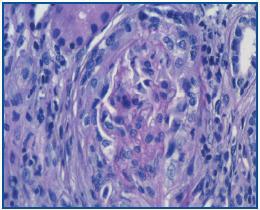
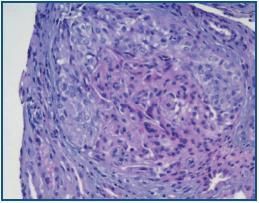
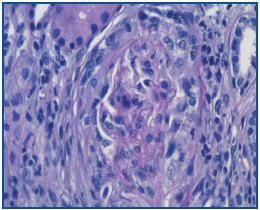
As glomerular disease was suspected, we performed a kidney biopsy. The anatomical pathology showed 10 glomerules, of which two were sclerotic and six had focal and circumferential epithelial crescents and diffuse mesangial proliferation and capillary lumens obliteration with a mixed interstitial inflammatory infiltrate. Negative immunofluorescence test (figures 1 and 2).
We started immunosuppression with three methylprednisolone tablets, followed by 1mg prednisone/kg/day and 900mg of cyclophosphamide in a monthly bolus, and followed up on the patient.
We arrived at the clinical opinion that it was probably overlap syndrome scleroderma/vasculitis with ANCA-anti-MPO+ with stage IV CKD secondary to proliferative mesangial glomerulonephritis with extracapillary proliferation.
Discussion
Hybrid forms of scleroderma/ANCAvasculitis, sometimes associated with glomerulonephritis, are described in up to 10% of all cases. This overlap syndrome may occur after a period of treatment with D-penicilamine which varies from five months to five years. For some authors, this association represents a new entity that is related with this drug.Although our patient had gone at least a year without taking it, we can establish the hypothesis that the D-penicilamine could have acted latently as an antigenic factor, and then triggered the extracapillary form of vasculitis.3-7
Figure 1.
Figure 2.