Dear Editor:
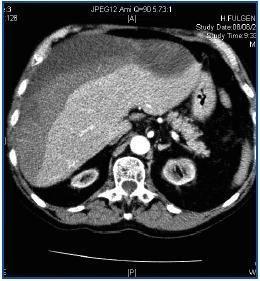
Patients on periodic HD have an elevated risk of spontaneous haemorrhages or haemorrhages caused by minimal trauma to the retroperitoneal, renal, pericardial, mediastinic and subdural areas. Multiple factors affect predisposition to bleeding, including platelet dysfunction, antiplatelet agents and anticoagulants.1,2 The development of a subcapsular hepatic haematoma is an exceptional complication that can occur spontaneously or with minimal closed trauma.3,4 We present a patient aged 77 years who in 2003 was diagnosed with chronic kidney disease second to myeloma kidney (IgG Kappa). Treatment with melfalan/prednisone decreased the circulating paraprotein and improved the medullar affectation. In February 2004, the patient began HD. During the last two years, the patient received two cycles of melfalan/prednisone, and later, bortezomib (Velcade®). He remained stable, with the disease under control and without anaemia with EPO. From April to July 2006, he received conjugated oestrogen (Equin®) (20mg/day) for uraemic thrombopathy. Lately, the patient has been taking aspirin as an anti-platelet agent. On 7 August 2006, eight hours after finishing the HD session, he experienced dizziness and fell, striking his right hypochondrium, and lost consciousness for several minutes. When he was admitted to the hospital he was conscious and aware of his surroundings; he complained of pain in his right scapula. Blood pressure was 55/35, cardiac frequency 72l/min and he showed sinus rhythm. Analytical tests showed: haematocrit 19%, haemoglobin 6.9g/dl, 300,000 platelets/mm3, 10,000 leukocytes/mm3 with the normal formula, PT 82%, INR 1.2 and fibrinogen 520mg/dl. Other data: Na 139mmol/l, K 6.7mmol/l, HCO3 22mmol/l, urea 84mg/dl, Cr 7.5mg/dl, GGT 727UI/l, GOT 127UI/l, GPT 167UI/l, LDH 372UI/l and total bilirubin 0.4mg/dl. A thoracic-abdominal CT with contrast revealed a subcapsular hepatic haematoma measuring 10 x 7 x 20cm in the right lobe; the organ was displaced, but without underlying hepatic lesions (figure 1). The kidneys were atrophic and there was a moderate amount of free liquid (blood) in the pouch of Douglas. To reverse the hypovolaemia, we administered isotonic saline and blood transfusions (four packs of red blood cells) and gum for the hyperpotasaemia. Six hours after being admitted, his haemodynamics were stable and he underwent an HD session without heparin. In the following 48 hours he remained at rest and under observation with frequent haematological checks.Haemoglobin levels remained stable. Local discomfort required mild analgesics.Over the following days, HD was performed under close monitoring and without heparin. Eight days after admission, during a CTexam, the haematoma had not increased in size and remained within the subcapsular area.The patient was referred to his original unit and follow-up by a series of CTs showed the slow, progressive reabsorption of the haematoma over eight weeks, with no need for surgery.
The likely causes that would favour bleeding, in addition to the uraemia, could include the myeloma itself, the administration of oestrogens, use of heparin during HD, the anti-platelet agent, and lastly, the closed local trauma. Although the CT showed no sign of underlying hepatic lesions (adenoma, haemangioma or peliosis) the patient could suffer from lesions arising from hepatic peliosis that were undetected by the CT.4,5 Hepatic peliosis , which is characterised by cystic blood-filled spaces in the sinusoids, is associated with the administration of androgenic-anabolic and other steroids, oral contraceptives and synthetic oestrogens. Its complications can include ruptured liver and spontaneous hepatic haematoma.6-12 In this case, both the myeloma and the oestrogens could have favoured the development of hepatic peliosis,8,10 making the liver more susceptible to spontaneous rupture or rupture from closed trauma.3 Many hepatic haematomas that are haemodynamically stable are given conservative treatment without surgical intervention and have a success rate of more than 80%.13,14 The only determining factor for it to be treated without surgical intervention is haemodynamic stability. In our patient, once his haemodynamics were stable, conservative treatment consisting of rest, transfusions, close monitoring and HD without heparin permitted favourable evolution and the resolution of the haematoma in two months.
To sum up, the development of a subcapsular hepatic haematoma in HD is a rare complication which, by producing a severe haemorrhage and shock, places the patient’s life at risk and is a challenging situation. Conservative treatment with no surgical intervention is an option that permits recovery without problems. As far as we know, this is the first case of a patient undergoing periodic HD who has presented this complication.
Figure 1.