Intoxication is a common disorder in hospital Accident and Emergency departments, especially drug poisoning1,2 (50% of cases). Clinical consequences and severity will depend on the characteristics of the poisoning agent and its metabolites, volume of distribution, molecular weight and protein affinity.3 Furthermore, comorbidities such as kidney or liver failure can cause a greater toxicity.
The first step in treating intoxications consists of maintaining the clinical and haemodynamic stability of the patient and avoid intestinal absorption of the toxic compound through emesis.3 Additional measures are sometimes required, such as extracorporeal blood purification techniques (EBPT), including haemodialysis and haemoperfusion, which promote blood purification of toxins generated endogenously by organ failure or exogenous poisoning.4,5
We present two overlapping cases of levothyroxine poisoning treated with haemoperfusion (HP).
Two female patients aged 50 and 53 years were admitted for attempts at self harm, in the first case (case 1), having taken 100 levothyroxine 50 mcg tablets and in the second case (case 2), 75 levothyroxine 50 mcg tablets. The patients had no relevant previous medical history.
On physical examination, both had a Glasgow Coma Scale score of 13–15 and were haemodynamically stable, with no significant abnormalities in heart rate or pulse oximetry. ECG showed no changes. Blood tests: case 1 T4 > 7.70 ng/dl, TSH 0.76 microU/mL; case 2 T4 4.47 ng/dl, TSH 0.06 microU/mL.
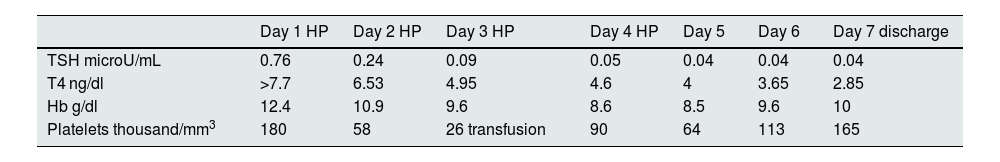
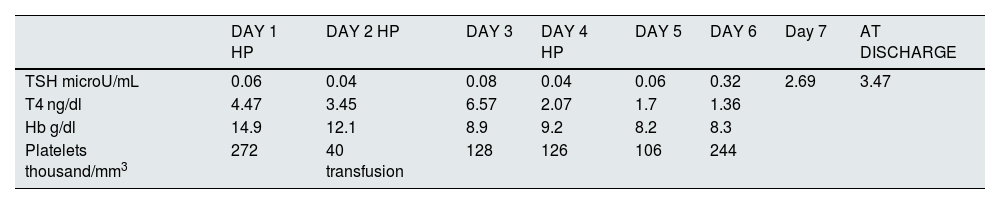
Both patients were admitted to the intensive care unit due to the risk of a thyrotoxic crisis; both had placement of femoral catheter within the first four hours to begin HP with activated charcoal. Four three-hour sessions were performed in case 1 and three sessions in case 2, basing the indication on the stability of the patients and their T4 levels. In case 1, after the last HP session she had a T4 level of 4 ng/dl, and at discharge 2.85 ng/dl; and in case 2 after the last HP session she had a T4 of 1.7 ng/dl, and at discharge 1.36 ng/dl (Tables 1 and 2). Both patients remained clinically and haemodynamically stable without emergency measures and without symptoms suggestive of thyrotoxic crisis.
Changes over time in laboratory parameters, patient 1.
| Day 1 HP | Day 2 HP | Day 3 HP | Day 4 HP | Day 5 | Day 6 | Day 7 discharge | |
|---|---|---|---|---|---|---|---|
| TSH microU/mL | 0.76 | 0.24 | 0.09 | 0.05 | 0.04 | 0.04 | 0.04 |
| T4 ng/dl | >7.7 | 6.53 | 4.95 | 4.6 | 4 | 3.65 | 2.85 |
| Hb g/dl | 12.4 | 10.9 | 9.6 | 8.6 | 8.5 | 9.6 | 10 |
| Platelets thousand/mm3 | 180 | 58 | 26 transfusion | 90 | 64 | 113 | 165 |
Hb: haemoglobin; HP: haemoperfusion.
Changes over time in laboratory parameters, patient 2.
| DAY 1 HP | DAY 2 HP | DAY 3 | DAY 4 HP | DAY 5 | DAY 6 | Day 7 | AT DISCHARGE | |
|---|---|---|---|---|---|---|---|---|
| TSH microU/mL | 0.06 | 0.04 | 0.08 | 0.04 | 0.06 | 0.32 | 2.69 | 3.47 |
| T4 ng/dl | 4.47 | 3.45 | 6.57 | 2.07 | 1.7 | 1.36 | ||
| Hb g/dl | 14.9 | 12.1 | 8.9 | 9.2 | 8.2 | 8.3 | ||
| Platelets thousand/mm3 | 272 | 40 transfusion | 128 | 126 | 106 | 244 |
Hb: haemoglobin; HP: haemoperfusion.
Levothyroxine poisoning is a rare but potentially life-threatening clinical condition. The severity of the poisoning or its toxicity is not necessarily related to the dose of levothyroxine or the initial T4 serum levels.6,7 Serum TSH levels do not show the severity of the condition, as it is not suppressed until 48−72 hours later. However, the concentrations of free T4 and free T3 are increases rise from the begining. It is therefore recommended to test both in the first few hours, as symptoms become evident when T4 is transformed into T3, which explains why patients can remain asymptomatic for the first few hours.6,7 Due to the half-life of levothyroxine (seven days), symptoms may appear up to day +11 after ingestion.
The symptoms of levothyroxine poisoning range from being asymptomatic to a wide range of clinical manifestations, including malignant hyperthermia, arrhythmias, acute myocardial infarction, cardiogenic shock, acute psychosis, convulsive states and coma,8,9 which is why admission to intensive care units is recommended.
There is no treatment protocol for levothyroxine intoxication; rapid action involving symptomatic treatment and gastrointestinal decontamination techniques (gastric lavage and administration of activated charcoal), and drugs that inhibit the metabolism of T4 to T3 are essential. In addition, therapies such as plasmapheresis and HP are capable of decreasing the half-life of T4 more quickly.10
The use of extrarenal blood purification techniques (EBPT) in the treatment of intoxications has been increasing in recent years.11 These techniques are reserved for the following scenarios: exposure to the toxic with potentially lethal high plasma concentrations; toxicity of the substance that cannot be counteracted by an antidote or treatments that prevent absorption and/or elimination; or a high probability of permanent disability or developing toxicity despite supportive measures.11
The principles that govern the elimination of the poison by EBPT are: diffusion; convection; adsorption; and centrifugation. The elimination of the poison depends on its characteristics: volume of distribution; percentage of protein binding; molecular weight; and the velocity of passage from the tissue to the vessel.4
Adsorption is a process by which particles located in the blood compartment bind reversibly or irreversibly to the surface of a sorbent column; in the case of HP, this is activated carbon (high adsorption capacity and contact surface area of 300−1,000 m2/g). HP enables the purification of high molecular weight toxins of up to 5,000 Daltons. Its extractive capacity is identical for water-soluble and fat-soluble poisons4,11 and is not limited by the degree of binding of the poison to plasma proteins.
HP requires greater systemic anticoagulation than other EBPT and non-selectively adsorbs platelets, white blood cells, calcium and glucose. It has to be replaced every two hours due to cartridge saturation.
Possible complications are common to other EBPT (hypothermia, haemorrhage, arterial hypotension and infection of vascular access routes), with the addition of thrombocytopenia, hypocalcaemia and hypoglycaemia.4
In summary, levothyroxine poisoning is potentially life-threatening and requires intensive care. The use of HP could ensure the relatively safe and effective management of potential adverse events deriving from the poisoning.