Antecedentes: El trasplante de órganos de donantes añosos en receptores de edad avanzada se ha incrementado en los últimos años. Esta situación plantea problemas específicos tanto en el órgano como en el receptor, y la pauta de inmunosupresión debe ser adaptada a ellos. Un estudio previo mostró buenos resultados iniciales en el trasplante renal de donante y receptor añosos (medias de edad: 64,4 y 61,3 años) con una inmunosupresión inicial de daclizumab, mofetil-micofenolato e introducción retrasada de tacrolimus a dosis bajas. En el presente estudio revisamos los resultados a largo plazo en ese mismo grupo de pacientes. Métodos: Estudio observacional, retrospectivo y multicéntrico a nivel nacional de la supervivencia y función renal de 126 pacientes incluidos en el estudio inicial (sobre 127 que alcanzaron el primer año con riñón funcionante, 123 tratados según protocolo). Obtuvimos datos del segundo al sexto año de: 120, 118, 113, 102 y 62 pacientes. Secundariamente se analizó la evolución de la función renal, aspectos clínicos relevantes y el perfil de seguridad. Resultados: A los 5 años, la mayoría de los casos continuaban con el esquema inmunosupresor inicial: 92% tacrolimus y 80% mofetil-micofenolato; 48% habían abandonado los esteroides y se introdujo un inhibidor de la señal de proliferación en 3%. La supervivencia del paciente y el órgano (censurada para muerte) a los 5 años resultó de 93,1 y 93,8%, respectivamente. La principal causa de muerte fue la neoplasia (en 7 de los 10 casos) y, de pérdida de injerto, la muerte con riñón funcionante. Las otras causas de muerte fueron 2 infartos agudos de miocardio y una hemorragia digestiva. La función renal se redujo significativa pero moderadamente a lo largo del tiempo (p < 0,001): la creatinina media en el conjunto de pacientes pasó de 1,60 ± 0,50 mg/dl al primer año a 1,63 ± 0,70 al cierre del estudio (p < 0,05); MDRD de 46,28 ± 15,64 ml/min al primer año a 45,69 ± 15,44 al cierre del estudio (p < 0,01). Sólo se registraron 2 rechazos agudos después del primer año. Se registraron 19 eventos cardiovasculares en 12 pacientes. Conclusiones: La pauta utilizada en nuestro estudio resulta útil y adecuada para parejas donante-receptor de mayor edad, como demuestran los buenos resultados en supervivencia a largo plazo, y el mantenimiento de una óptima función renal y un perfil de seguridad aceptables.
Background: Organ transplants in elderly recipients have increased over the past few years. This situation poses specific problems both in terms of organs and recipients; therefore, immunosuppressant regimens must be adapted accordingly. A previous study demonstrated good initial results in kidney transplant cases in which older donors and recipients (average ages of 64.4 years and 61.3 years) had received initial immunosuppressant therapy with daclizumab and mycophenolate mofetil as well as delayed introduction of reduced-dose tacrolimus. In this study we reviewed the long-term results in the same group of patients. Methods: An observational, retrospective multi-centre study carried out at a national level to determine survival rates and renal function in 126 patients included in the initial study (127 patients who survived the first year with a functioning graft, 123 treated according to protocol). We gathered data from the 2nd to the 6th year for 120, 118, 113, 102 and 62 patients, respectively. The evolution of renal function, relevant clinical data, and safety profiles were also analysed. Results: After five years, most patients continued with the initial immunosuppressant regimen: 92% tacrolimus and 80% mycophenolate mofetil; 48% had abandoned steroids and proliferation signal inhibitors had been introduced in 3%. Patient and graft survival (adjusted for patient death) after five years was 93.1% and 93.8%, respectively. The main cause of death was neoplasia (in 7 out of 10 cases) whilst graft loss was mainly due to death with a functioning graft. The other causes of death were 2 acute myocardial infarctions and a gastrointestinal haemorrhage. Renal function was moderately but significantly reduced with the passing of time (P<.001): average creatinine levels in the overall group of patients rose from 1.60±0.50mg/dl after the 1st year to 1.63±0.70mg/dl at the end of study. MDRD dropped from 46.28±15.64ml/min after the 1st year to 45.69±15.44ml/min at the end of study (P<.01). Only two acute rejections were observed after the 1st year. There were 19 cardiovascular events registered in 12 patients. Conclusions: The regimen used in our study was useful and appropriate for elderly donor-recipient pairs as demonstrated by the good long-term survival results, continued optimum renal function, and acceptable safety profile.
INTRODUCTION
The global increase in life expectancy and the expanded use of renal replacement programmes for chronic kidney disease have led to an increase in the mean age of patients treated.1 Kidney transplants (KT) are currently the treatment of choice for appropriate patients with established chronic kidney disease, since they improve patient survival and quality of life as compared to those who remain on dialysis, not only in young individuals, but also in the elderly population.2 Several studies have yielded excellent results performing transplants in elderly recipients, with patient and graft survival rates of 70% and 60%, respectively, after 5 years.3 These results have led to the growing acceptance of placing elderly patients on organ waiting lists.4
The expansion of inclusion criteria for KT combined with a limited availability of donated organs has led to the use of cadaveric donors at higher ages, even although these kidneys are inferior.3,5 The structural and functional changes associated with advanced age (glomerulosclerosis, arteriolar hyalinosis, reduced functional kidney mass, and reduced glomerular filtration rate) can make these organs especially vulnerable to the aggressions produced in the ischaemia-reperfusion process, since tissue repair mechanisms are diminished in these cases. These factors increase the risk of delayed graft function and acute rejection5,6 and decrease the rate of graft survival. On the other hand, the primary cause of graft loss in elderly recipients is the death of patients with a functioning graft (approximately 50%, versus 15% in young recipients), which might imply that organs with a shorter expected functional life span would cover the needs of elderly recipients in terms of life expectancy.4,6 This is why kidneys donated by elderly donors are usually transplanted into elderly recipients.7
The physiological alterations that occur with advanced age include changes in absorption, distribution, and metabolism, which affect the pharmacokinetics and pharmacodynamics of immunosuppressant drugs, increasing the frequency and severity of toxicity.8-10 Calcineurin inhibitors (CNI) can negatively affect the incidence and duration of delayed renal function, increasing the risk of acute nephrotoxicity by inducing oxidative stress.11,12 The prolonged use of CNI at normal doses contributes to decreased renal function and chronic allograft nephropathy, which is the primary cause of late graft loss. In addition, the use of these drugs can exacerbate many of the more important cardiovascular risk factors in these patients (hypertension, diabetes mellitus, and dyslipidaemia), and increases the risk of developing tumours.13,14
The majority of studies researching the most appropriate immunosuppression therapy in elderly transplant recipients have thus been based on low or non-existent CNI regimens,14-16 and usually involve antibody-based induction, mycophenolate mofetil (MMF), and/or proliferation signal inhibitors (PSI).17
In a previous study carried out by our group involving 133 KT with elderly donors and recipients, we observed good patient and graft survival rates (after 12 months, patient survival was 97.7%, graft survival was 96.1%, and graft survival adjusted for patient death was 98.5%), with good renal function and a low rate of secondary side effects. The treatment protocol involved daclizumab, MMF, and delayed introduction of low doses of tacrolimus (TC).18 In this study, 42.86% of patients suffered initial delayed graft function and 13.5% suffered acute rejection. In the present study, we have reviewed the long-term results from this same group of patients.
PATIENTS AND METHOD
The primary objective of our study was to analyse long-term patient survival. We also examined the evolution of renal function, the number of patients whose CNI and/or anti-metabolite regimens were modified, the safety profile associated with blood pressure and glucose and lipid metabolism, and the rate of neoplasia.
We designed a nationwide observational, retrospective, multi-centre study of the evolution of patients who reached 1 year of follow-up from the group of 133 patients that started the initial study.18 The selection criteria for the original study were: age ≥50 years, panel reactive antibodies <25% in the previous 6 months, and recipients of a single kidney, coming from organ donors ≥55 years of age, with a cold ischaemia time <30 hours. In terms of sex distribution, 64% of donors and 60% of recipients were male. The mean age of the recipients was 61.3±6.2 years and the mean donor age was 64.4±5.3 years.
Initial immunosuppressant treatment consisted of daclizumab in combination with MMF, TC, and steroids. Patients received two doses of daclizumab at 1.0mg/kg (maximum: 100mg): the first dose 6 hours before starting the transplant surgery (day 0 of the study), and the second dose on day 14. MMF was administered orally at 2g/day (1g/12 hours) until day 45 of the study, and was then adjusted based on the criteria of each centre. The initial dose of TC was 0.1mg/kg/day, and was started between the 5th and 7th day after transplantation, once renal function had stabilised (creatinine [Cr] less than 3.0mg/dl, or Cr clearance >30ml/min) and never after 7 days following the procedure. Dosage was adjusted in order to reach trough levels of 4-8ng/ml. As regards steroid treatment, methylprednisolone was administered at 500mg at the moment of surgery, and was then reduced in the following manner: day 1: 125mg intravenously every 24 hours; days 2-14: 20mg/24 hours; days 15-30: 15mg/24 hours; days 31-90: 5-10mg; and days 91-360: according to each hospital’s protocol. Prophylactic treatment was recommended against cytomegalovirus and Pneumocystis jiroveci, following the established protocol at each hospital.
For the statistical analysis, we measured the following variables at the end of years 1-6 of the TR follow-up period: renal function (plasma Cr and glomerular filtration rate [MDRD]), standard laboratory measurements, post-transplant de novo diabetes (defined using the American Diabetes Association [ADA] criteria), neoplasia, biopsy-confirmed acute rejection, blood pressure, dyslipidaemia, type of immunosuppression (drugs, doses, and blood levels of CNI, reasons for drug withdrawal if any, and toxicity), concomitant drugs prescribed (anti-hypertensive agents, lipid-lowering drugs, oral anti-diabetic and/or insulin drugs, and erythropoietin), graft loss, and/or death and causes.
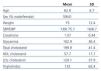
One hundred and twenty-seven of the 133 patients included in the original study reached the first year with a functioning kidney transplant, and 122 of them were included in the present study and monitored in participating hospitals. Their general characteristics are described in the Table. We obtained information regarding patient evolution for all 122 cases, almost all of which were monitored for at least 5 years. At the time this study was completed, only 62 patients had reached six years of follow-up.
STATISTICAL ANALYSES
We used SPSS statistical software, version 11.0, for all descriptive and inferential statistical analyses. Organ and patient survival rates were calculated using Kaplan-Meier survival curves at 1, 2, 3, 4, 5, and 6 years following transplantation. All other variables were expressed as absolute and relative frequencies in the case of qualitative variables, and as mean, standard deviation, median, and interquartile range for quantitative variables. We also analysed changes in immunosuppressant regimens and the combination of immunosuppressants between the follow-up years using Pearson’s chi-square tests for qualitative variables. We established a significance level of P<.05. For all cases in which we compared different variables at two different moments in time (baseline vs 1 year post-transplantation) we used paired two-tailed t-tests.
RESULTS
Over the course of the study, the number of patients maintained within the follow-up programme was: 120 (end of 2nd year), 118 (end of 3rd), 113 (end of 4th), and 102 (end of 5th); only 62 patients were monitored for 6 years. The primary objective of the study, patient and organ survival (adjusted for patient death) 5 years after KT, resulted in 93.1% and 93.8%, respectively (determined from the survival results for all 122 cases starting at the time of the KT). A total of 10 deaths were reported over the course of the study. The most common causes of death were neoplasia (7 of 10 cases); specifically, 2 lymphoma, 2 brain tumours, 2 pulmonary adenocarcinomas, and 1 colon adenocarcinoma. The majority of cancers appeared between the 5th and 6th years following KT. The other causes of death were 2 acute myocardial infarctions (in the 2nd and 3rd years), and one gastrointestinal haemorrhage (in the 3rd year). The primary cause of graft loss was death with a functioning kidney, and all other failures were attributed to chronic allograft nephropathy (6 cases) or unknown cause (2 cases).
The mean creatinine value increased from 1.60±0.50mg/dl in the first year to 1.63±0.70mg/dl at the end of the study (P<.05); mean MDRD score went from 46.28±15.64ml/min/1.73m2 to 45.69±15.44ml/min/1.73m2 (P<.001) (Figure 1). At the fifth year of follow-up, mean Cr was 1.61±0.60mg/dl (P=.068), and MDRD was 45.79±15.25ml/min/1.73m2 (P<.01). In the paired two-tailed t-test for repeated measures, renal function (measured by Cr or MDRD) decreased significantly over time (P<.001), although this was progressive and moderate in absolute terms. These comparisons do not take into account the effect of positive selection in terms of deaths (patients with better initial renal function tend to survive longer). Analysing patients that reached the 6th year of follow-up as a separate group, mean Cr went from 1.49±0.40mg/dl in the first year to 1.69±0.70mg/dl in the 6th year (P<.05); mean MDRD in this group went from 49.40±14.54ml/min/1.73m2 in the first year to 48.62±14.31ml/min/1.73m2 in the sixth year (P<.001). This change, which was quantitatively somewhat higher than in the overall group, is still not very clinically relevant.
Only 2 cases of acute rejection were recorded after the first year of follow-up, both of which were associated with by T-cells and occurred during the second year, with IA and IIA histological classifications (Banff criteria) and a good response to steroid bolus treatment. The level of compliance with the initial immunosuppression scheme was very high, such that, after 5 years, 92% of patients continued treatment with TC and 80% continued with MMF (Figure 2). The most common cause of withdrawal of MMF was an attempt to reduce immunosuppression dosage, followed by gastrointestinal toxicity and haematological toxicity (leucopoenia). The mean TC dose was progressively reduced from 4.09mg/day at the end of the first year to 2.95mg/day at the end of the fifth year, with mean trough blood levels of 7.35ng/ml and 6.2ng/ml, respectively (Figure 3). The mean dose of MMF remained fairly stable from the second year onwards, and was 997mg/day at the fifth year. Steroids were suspended in the second year in 38% of patients, and in the sixth year in 48%. In a small group that constituted 4% of the total at the end of the study, a PSI was also administered. In another small group of 2.4% of patients, azathioprine was started, in the second year in almost all cases, and was maintained until the end of the study (Figure 2).
Throughout the follow-up period, concomitant medication was increased in order to provide better control of the most frequently risk factors in these patients. Anti-hypertensive drugs, which were used by 76% of patients at the end of the first year, were employed in 92.9% of patients at the end of the fifth year; statin use rose from 32.6% to 63% over this same interval, erythropoietin use rose from 8.7% to 18.4%, and oral anti-diabetic and/or insulin drug use rose from 9.8% to 15.7%; all of these differences in drug use were statistically significant. A total of 19 cardiovascular events occurred in 12 patients over the course of the study: 3 acute myocardial infarctions (2 of which caused patient death), 2 strokes, and 14 peripheral arteriopathies. At least one type of cancer was observed in 14.3% of patients (and more than 1 was observed in 4%). Skin cancer was the most common form of neoplasia (50%), while post-transplant lymphoproliferative syndrome accounted for 11% and other solid tumours constituted 39%.
DISCUSSION
The waiting lists for KT programmes show a growing proportion of older patients. At the same time, the mean donor age has increased in recent years, with a consequently higher rate of associated cardiovascular pathology and functional deterioration of the transplant. This has led to an increasing practice of transplanting organs from elderly donors and those with expanded criteria into elderly recipients. The validity of assigning these organs to elderly recipients has been shown in several studies.19,20
Some authors have suggested that the rate of rejection in elderly recipients is lower due to the less active or quiescent immune system in these patients. While the results extracted from large studies of the United Network for Organ Sharing (UNOS) appear to confirm this hypothesis, other authors examining more recent patient groups have not observed a large difference in the rate of acute rejection between young and elderly recipients.21,22 On the other hand, the lower functional reserve inherent to the decreased nephron mass in elderly donors, as well as the reduced capacity for regeneration of the tissues after rejection, makes the case for a more negative impact on graft survival, compared young recipients.23
There is a higher rate of associated comorbidities in elderly patients, such as diverticulosis, urinary tract anomalies, cardiovascular pathology, and diabetes, among others, as well as a higher incidence of cancer.21,24 As such, the risk of suffering severe infections and tumour-related diseases following immunosuppression therapy is higher, and the rate of mortality due to these processes is higher than in young recipients.25 These factors require an adapted immunosuppression regimen for the specific characteristics of the donor and the recipient. This protocol must be sufficiently effective to avoid rejection (because of the lower graft survival rate and the higher risk of infection associated with treatment) but must not lead to over-immunosuppression, which could increase the number of infections and tumours in more susceptible recipients. However, we also lack prospective multi-centre studies with a randomised design that have analysed this issue in large cohorts of patients. In addition, elderly recipients are frequently excluded from trials of new immunosuppressant treatments due to the possibility of secondary side effects associated with altered pharmacokinetics that might impede the interpretation of study results. The need for reducing the nephrotoxicity associated with CNI, whose effects may be exacerbated by ischaemia-reperfusion damage, thus preserving the largest nephron mass possible, makes prescriptions that minimise or fully eliminate CNI of special interest in this group of recipients.21,26
Induction with anti-lymphocyte antibodies or anti-IL-2 is very useful for reducing the prevalence of acute rejection. Given the lower risk of severe infection or cancer associated with their use, IL-2 antibody receptor antagonists may be preferable over thymoglobulin in recipients with a low immunological risk: the rate of acute rejection does not vary by much, but this does provide a better safety profile.26,27
Arbogast et al15 treated patients without CNI using MMF doses adjusted to maintain trough levels of 2-6µg/ml and induction with mono-polyclonal antibodies in recipients and donors of a similar age to our study. They observed a 5-year survival rate of 87.69% and a graft survival rate of 69.8% (adjusted for patient death and non-immunological causes: 86.57%), although this was lower than in our study and involved a much higher rate of acute rejection (23.6%).15 Later publications from this same group observed similar results with even higher rejection rates, which led to 46.3% of patients receiving and added CNI in their treatment regimens. Despite the good survival rates observed in comparison to other studies involving treatment with CNI, the high rates of rejection and cytomegalovirus infection (requiring a reduction of MMF and the introduction of CNI or PSI) place doubts on the validity of immunosuppression regimens without CNI.28,29
In a controlled study (SENIOR), no advantages were observed with a delayed introduction of TC (after 7 days, after complete withdrawal of steroid treatment) as compared to immediate use, in terms of frequency, duration of functional delay, or renal function after 6 months.30 The mean duration of functional delay in the case of donors older than 60 years with a delayed introduction of TC was 19 days, much higher than in our study (7 days, with a median of 4 days); the frequency of early acute rejection was also much higher in this study than in ours. Previous studies also failed to demonstrate an advantage of delayed TC introduction with depletive antibody31 or cyclosporine32 induction in terms of the incidence of delayed function. However, initial CNI doses and levels in these studies were standard and higher than in ours. In all likelihood, the appearance of delayed graft function requiring dialysis is mediated by factors that come into play prior to immunosuppression therapy (donor age, vasculopathy, cause of death, conditions surrounding donor suffering, cold ischaemia, etc.) and cannot be modified by a delayed introduction of CNI. In contrast, lower doses and blood levels (with or without delayed introduction) may be more useful for shortening its duration. The results of the Symphony study33 attest to the efficacy and safety of an immunosuppressant regimen with low initial doses of TC.
In a study involving 72 patients older than 60 years, Solà et al. assessed the results of a treatment regimen based on steroids, MMF, and TC, with the addition of thymoglobulin and a delayed start of TC (at 1mg/kg/day, similar to our study) upon delayed graft function (which occurred in 48.6% of cases). This led to a rapid resolution of delayed graft function cases (mean 3.9 days) and a 12.5% rejection rate. Patient survival after 3 years was 90%, and graft survival was 87% (97% after adjusting for patient death).34
In our experience, the use of this treatment regimen produces very satisfactory results in terms of mid-term patient and organ survival, with even better rates than those observed in other studies.29 As in previous studies, the primary cause of graft loss was patient death, primarily due to cancer. None of the deaths in our study were due to infections. The rate of acute rejection after the first year was low, showing a sufficient level of immunosuppression. Deterioration of renal function was very mild, with excellent Cr and GFR rates at the end of the fifth year. We also observed a very high level of compliance with the prescribed immunosuppression protocol, as most patients remained on the planned MMF/TC regimen. There was a clear tendency for the maintenance of trough TC values at the upper limit of the predicted range during the first years of follow-up, although these values became more moderate over the course of the study. This is probably due to the minimal treatment applied when using a conservative approach, as observed in large studies such as the Symphony study.33
The design of our study had some methodological weaknesses, such as the retrospective nature of the study and the lack of a control group treated with an immunosuppression regimen without delayed introduction and minimal doses of CNI, as we explained in our previous publication. Prospective studies without these limitations and involving a larger number of patients would be needed to establish how appropriate this type of immunosuppression therapy would be for the transplantation of organs from elderly or expanded criteria donors into elderly recipients.
In conclusion, we believe that the treatment regimen used in our study, involving induction with two doses of daclizumab, along with MMF and a late introduction of TC at low doses, is useful and appropriate for elderly donor-recipient pairs, as shown by the good long-term survival results and the maintenance of optimal renal function and acceptable safety profiles.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Patient characteristics after one year
Figure 1. Evolution of renal function
Figure 2. Use of immunosuppressants (% of all patients) in each year following transplantation
Figure 3. Evolution of tacrolimus trough blood levels throughout the study