La estenosis arterial del injerto renal es una complicación que requiere, en ocasiones, un abordaje terapéutico con cirugía o angioplastia. El objetivo del presente estudio es analizar la evolución de 13 pacientes trasplantados renales con estenosis arterial del injerto tratados mediante angioplastia y colocación de stent. La sospecha clínica se fundamentó en un deterioro de función renal, acompañado de mal control de la presión arterial en algunos casos, con ecografía doppler compatible. Se realizó una arteriografía que confirmó el diagnóstico y en el mismo acto se realizó una angioplastia con colocación de stent. Se objetivó una mejoría progresiva de la función renal durante los 3 primeros meses que permaneció estable durante los dos primeros años. Por otro lado, mejoraron las cifras de presión arterial en los dos primeros años, manteniendo el mismo tratamiento antihipertensivo. En conclusión, la angioplastia con colocación de stent es un procedimiento efectivo y seguro en el tratamiento de la estenosis de la arteria del injerto renal.
Transplant renal artery stenosis is a major complication that requires a therapeutic approach involving surgery or angioplasty. The aim of this study was to analyse the evolution of renal transplant patients with renal allograft artery stenosis treated by angioplasty and stent placement. Thirteen patients were diagnosed with transplant renal artery stenosis. Clinical suspicion was based on deterioration of renal function and/or poorly controlled hypertension with compatible Doppler ultrasound findings. The diagnosis was confirmed by arteriography, performing an angioplasty with stent placement during the same operation. A progressive improvement in renal function was observed during the first 3 months after the angioplasty, and renal function then remained stable over 2 years. In addition, blood pressure improved during the first 2 years, and as a consequence there was no need to increase the average number of anti-hypertensive drugs administered (2.5 drugs per patient). In conclusion, angioplasty with stent placement is a safe and effective procedure for the treatment of transplant renal artery stenosis.
INTRODUCTION
Transplant renal artery stenosis is an important complication that causes arterial hypertension, deteriorating renal function, and even renal graft loss, and has an incidence rate of 1%-23%.1-3 This condition usually arises during the first few years following transplantation.1,2 The diagnosis is suspected based on Doppler ultrasound images while renal arteriography continues to be the gold standard for diagnostic confirmation and treatment, since this procedure facilitates angioplasty and stent placement all in the same intervention.
Until now, no randomised clinical trials have been carried out to establish whether endovascular treatment produces superior results to surgery. On the other hand, there is also debate regarding the effects of medical treatment or angioplasty with stent placement on blood pressure and renal graft function.
The aim of our study was to analyse the evolution of kidney transplant recipients with graft artery stenosis undergoing percutaneous transluminal angioplasty and stent placement.
MATERIAL AND METHOD
We performed a prospective observational study of 13 patients with kidney transplants diagnosed with renal allograft artery stenosis who were treated with angioplasty and stent placement. Mean age was 54 years (range: 29-73 years); 11 patients were men and 2 women.
The mean post-kidney transplant time was 180 months (range: 7-1260 months), 6 patients had early stenosis (<2 weeks following transplantation), 6 patients developed stenosis during the first year following transplantation (range: 54-240 days), and 1 patient had late stenosis (3 and a half years following transplantation). The clinical suspicion of stenosis was based on deteriorated renal function accompanied by elevated blood pressure in some cases, and a Doppler ultrasound analysis of the renal artery compatible with the diagnosis of stenosis. All patients were under immunosuppression treatment with prednisone, tacrolimus, and mycophenolic acid. The stents had a mean length of 17.7mm (range: 12-24mm) and a mean diameter of 5.3mm (range: 5-6mm). After the procedure, patients received follow-up treatment with 100mg of acetyl-salicylic acid indefinitely and 75mg of clopidogrel during the first month.
We evaluated clinical variables (family history, tobacco use, hypertension, diabetes, dyslipidaemia, cardiovascular diseases, aetiology of the chronic kidney disease), reason for arteriography, number and location of lesions observed, and patient evolution following treatment (renal function, blood pressure, number of anti-hypertensive drugs). The results are expressed as mean and standard deviation. We compared means using Student’s t-tests.
RESULTS
Our patients had multiple cardiovascular risk factors (12 arterial hypertension, 6 dyslipidaemia, 4 diabetes, 2 tobacco use) and 4 suffered a cardiovascular event. Arterial stenosis was suspected in light of deteriorating renal function in 11 patients, and due to arterial hypertension in 2.
Doppler ultrasound revealed type 3 waves in 9 patients and type 2 waves in 4 cases. The stenosis was located in the ostium in 8 patients and in the proximal third of the renal artery in 5 patients.
The stenosis was resolved by radiological intervention in all 13 cases, with the only complication being one case of haematoma at the puncture site, which resolved spontaneously.
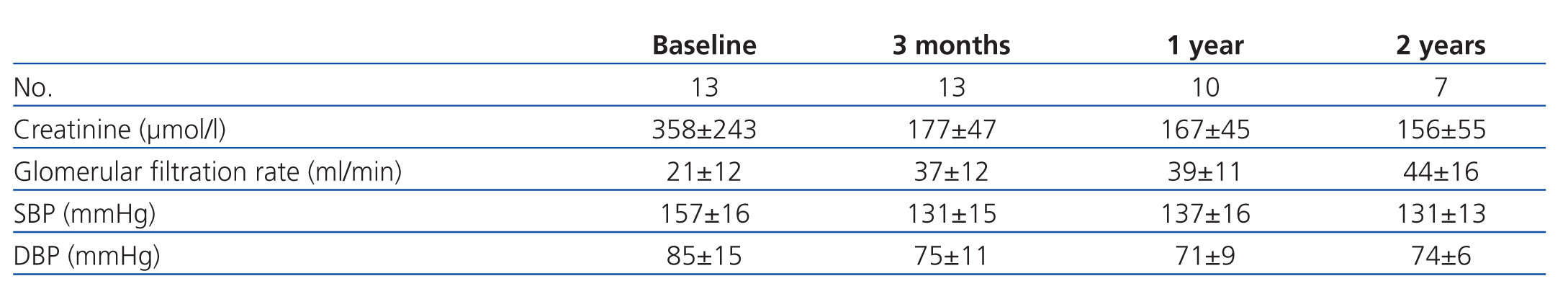
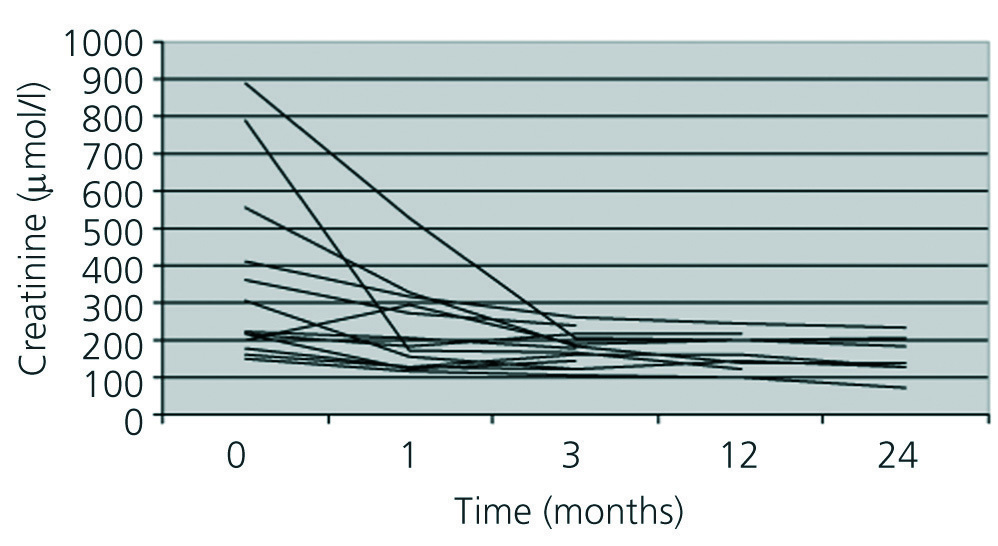
Table 1 shows the overall evolution of patients following the procedure. We observed a progressive improvement in renal function during the first 3 months, which remained stable during the following two years. Blood pressure levels also improved over the two-year period, and the mean number of anti-hypertensive drugs administered also remained stable (2.5 drugs per patient). Figure 1 displays the evolution of renal function for each patient.
There were no long-term complications from the procedure. One patient died 8 months after transplantation due to invasive pulmonary disease caused by cytomegalovirus.
DISCUSSION
The most important finding in this study was the technical and functional success of the procedure, with improved renal function and control of blood pressure following angioplasty and stent placement in transplant renal artery stenosis, with no long-term complications. Almost half of the procedures were carried out within two weeks of transplantation, which has not been reported before in the medical literature.
Post-transplantation vascular complications are rare, but very important, since they may cause allograft dysfunction and loss. The aetiology of stenosis is multifactorial, including reduced vessel diameter and atherosclerosis in the donor artery, trauma in the donor artery during removal of the organ or in the recipient’s artery during surgery, the suturing technique used, and damage to the iliac artery during transplantation.
Our results contrast with those from the ASTRAL study4 of patients with renal artery stenosis in native kidneys. They found no evidence of a clinical benefit following revascularisation in patients with renovascular atherosclerotic disease. In our study, stenoses occurred during the first year following transplantation (within the first 2 weeks in half of all cases) and they were found in the ostium in 8 cases, which suggests that the surgical procedure itself plays a very important role in the aetiology of the condition, both because of the quality of the vessels in expanded criteria donor kidneys and the length of the vessels in living donor kidneys removed by laparoscopy.
Several studies have also shown the benefit of percutaneous interventions in transplant renal artery stenosis.5-7 These studies had small sample sizes, with 10-24 patients and a short follow-up period, and therefore lack statistical consistency. One of these studies demonstrated significantly improved renal function and blood pressure values only one week after the procedure. Recently, a study involving angioplasty without stent placement in 44 patients reported improved allograft survival after 5 years, as compared to patients that underwent surgery or conservative medical treatment.8
On the other hand, a study performed in 43 patients failed to demonstrate any benefits of angioplasty during a 5-year follow-up period,9 and another study involving 18 patients treated with angioplasty showed a decrease in mean blood pressure of 7.3mm Hg, with no improvements in glomerular filtration rates after 6 months. In our study, systolic blood pressure dropped by a mean 20mm Hg and diastolic blood pressure by a mean 14mm Hg one year after the procedure.
The use of transluminal percutaneous angioplasty without stent placement has been associated with re-stenosis rates of 16%-62% according to some studies, while the same procedure with stent placement caused a re-stenosis rate less than 10%.5 In our study, we did not observe any cases of re-stenosis, although we were unable to compare our results with a non-stent control group.
Some studies have described acute complication rates of 5%,11 but only one early complication arose in our study: a haematoma at the puncture site. It was quickly resolved through conservative treatment and caused no long-term complications.
In conclusion, our study suggests that correcting transplant renal artery stenosis using percutaneous transluminal angioplasty and stent placement is an effective and safe procedure, improving glomerular filtration rates and blood pressure values.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Evolution of renal function and blood pressure following angioplasty and stent placement
Figure 1. Progression of individual renal function