Aim: To test the feasibility, efficacy and safety of a new two port laparoscopic technique for dialysis catheter placement. Material and methods: From January 2006 to July 2009 51 patients underwent dialysis catheter placing using an original technique. All procedures were finished laparoscopically using two 12 mm-sized ports. Our technique bases on placing Oreopoulos- Zellerman catheter along a straight Guyon´s guide with atraumatic tip, visually guaranting optimal placement. Catheter can be repositioned if desired by reentering the guide. Median follow-up was 25 months. Results: Mean operating time was 32 minutes (range 15-55 minutes). One patient suffered an immediate postoperative catheter obstruction that required surgical repositioning. No other technical intra or early postoperative complications related to technique were reported. Mean time to discharge 1,02 ± 2.2 days. Catheter outflow failure rate was 7.6%. Conversion to haemodialysis due to peritonitis 13%. Peritonitis per patient/year was 0.27. Catheter 6 mo, 1 year and 2 year survival rate was 94%, 87% and 72%. Catheter migration rate was 4%. There was no peritoneal dialysis liquid leakage. Conclusions: The two ports technique described is an easy and rapid procedure, with few complications and early discharge. Due to its reliability, offers good catheter function outcome.
Objetivo: Estudiar la viabilidad, la eficacia y la seguridad de nuestra técnica de dos puertos de colocación de catéter de diálisis peritoneal por laparoscopia. Material y métodos: Desde enero de 2006 a julio de 2009, 51 pacientes fueron sometidos a colocación de catéter de diálisis peritoneal usando una nueva técnica. Todos los procedimientos se completaron laparoscópicamente usando dos puertos de 12 mm. Nuestra técnica se basa en la colocación de un catéter de tipo Oreopoulos-Zellerman sobre una guía de Guyon recta con punta atraumática, y garantiza la óptima colocación del catéter. En caso necesario, éste se puede poner de nuevo mediante la recolocación de la guía. El seguimiento medio ha sido de 25 meses. Resultados: Tiempo quirúrgico medio: 32 minutos (rango 15-55 minutos). Un paciente presentó una obstrucción del catéter en el postoperatorio inmediato, que requirió recolocación quirúrgica. No se han producido otras complicaciones técnicas durante la cirugía o el postoperatorio inmediato. Media de tiempo al alta: 1,02 ± 2,2 días. Tasa de obstrucción del catéter: 7,6%. Tasa de conversión a hemodiálisis secundaria a peritonitis: 13%. Episodios de peritonitis por paciente-año: 0,27. Supervivencia del catéter a los 6 meses, un año y 5 años: 94, 87 y 72%, respectivamente. Tasa de migración de catéter: 4%. No se han comentado casos de fístula de líquido peritoneal. Conclusiones: La técnica de dos puertos descrita es un procedimiento sencillo y rápido, con pocas complicaciones y alta hospitalaria inmediata. Debido a su fiabilidad, ofrece buenos resultados en la función del catéter.
INTRODUCTION
Peritoneal dialysis (PD) is a valid alternative to haemodialysis, which, in comparison, possesses some advantages. With regards to patients, PD allows for improved mobility, more dietary freedom, better haemodynamic control and less technical complexity.1 From an economic point of view, PD has a lower cost compared with haemodialysis. In sum, PD patients have higher satisfaction than patients on haemodialysis.2-8 On the other hand, PD has some disadvantages, most of them related to the catheter, such as catheter infection, obstruction, or migration of the catheter, cuff extrusion, incisional hernias, and fluid leaks.5,9-12
Catheter placement techniques have evolved from open surgery to minimally invasive procedures over the past two decades. In parallel, percutaneous placement of the dialysis catheters through the Seldinger technique has been used.13 At present, catheter placement can be performed through open surgery, percutaneous insertion, or laparoscopic surgery. Open surgery is a simple procedure, which requires a minimal laparotomy, and has been the most widely used option.2,7,14-16 However, open surgery allows a limited view, especially significant in patients with history of abdominal surgery, in which intestinal adhesions can hinder the procedure.17-19 For this reason, the rate of obstruction of catheters placed by open surgery reaches 22%.3,15,16,20
These technical problems with open surgery led to the development of new strategies for PD catheter placement two decades ago. Laparoscopic surgery, performed mostly with three trocars, was developed at this point.21,22 By providing an optimal view of the peritoneal cavity, and thus decreasing catheter obstruction and obstruction-related infections, the laparoscopic approach has gained wide acceptance.23-25 Laparoscopic surgery has a number of clear benefits, especially in the reduction of postoperative pain. Less postoperative pain allows for an earlier discharge and an early normalisation of social life.4,26 Furthermore, skilled laparoscopic surgery offers better cosmetic results. In this study we describe a new surgical technique for PD catheter placement using a laparoscopic approach with two ports. This initial experience examines viability, effectiveness, and safety.
MATERIAL AND METHOD
We prospectively analysed 51 consecutive patients who underwent PD catheter placement at our centre from January 2006 to July 2009. Demographic, clinical, preoperative and postoperative data were collected prospectively.
Demographic data
Patients included 19 women and 32 men, mean age 56 ± 18 years. All procedures were performed under general anaesthesia. The mean body mass index was 24.5 ± 3.5kg/m2. The average anaesthetic risk (ASA) was III (40% ASA II, 48% ASA III, 12% ASA IV).
Surgical technique
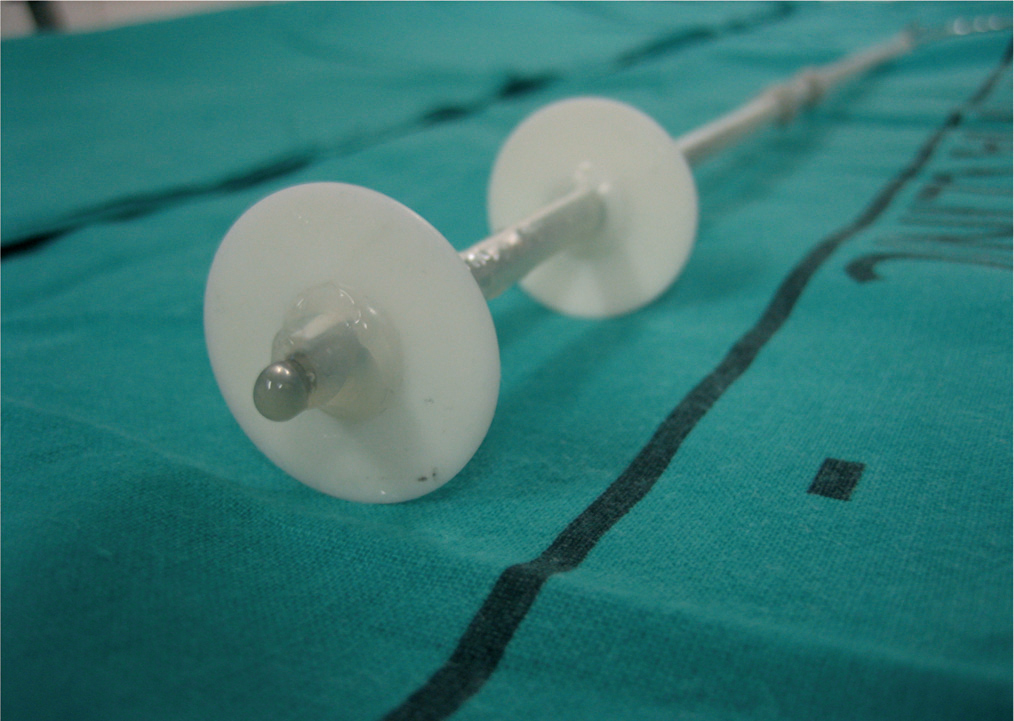
Here we describe a new surgical technique using two 12mm ports for PD catheter placement; for this, a Guyon guide with atraumatic tip was used (Figure 1). After lubricating the Guyon guide, the catheter was placed over it to obtain a rigidly braced catheter. An Oreopoulos-Zellerman catheter was used.
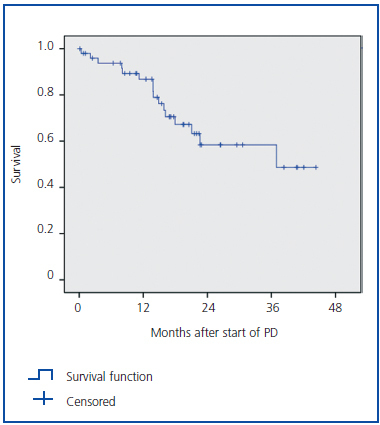
We achieved pneumoperitoneum by minimal periumbilical laparotomy and a 12mm trocar was placed. Under direct visualisation, a left pararectus 12mm trocar was placed. The optics were placed through this trocar and the catheter with the guide was placed through the periumbilical trocar. Then, the tip of the catheter was situated in the pouch of Douglas and the Guyon guide was removed. Proper catheter position was checked visually, after which the two trocars could be removed. A subcutaneous tunnel was created between the two trocars and the catheter is exteriorised through the left pararectus trocar hole (Figure 2).
RESULTS
All procedures were completed laparoscopically with two 12mm ports. Mean operative time was 32 minutes (range: 15-55 minutes). One patient had catheter obstruction in the first 24 hours after placement and required surgical revision and relocation. No other complications occurred during the intraoperative or immediate postoperative period. Mean
follow-up was 25 months. The average stay was 1.02 ± 2.2 days. Approximately twothirds of patients (65%) were discharged on the day of surgery, and up to 80% within the first 24 hours postoperatively. Patients who remained in the hospital after 24 hours of the procedure did so for medical problems unrelated to the procedure.
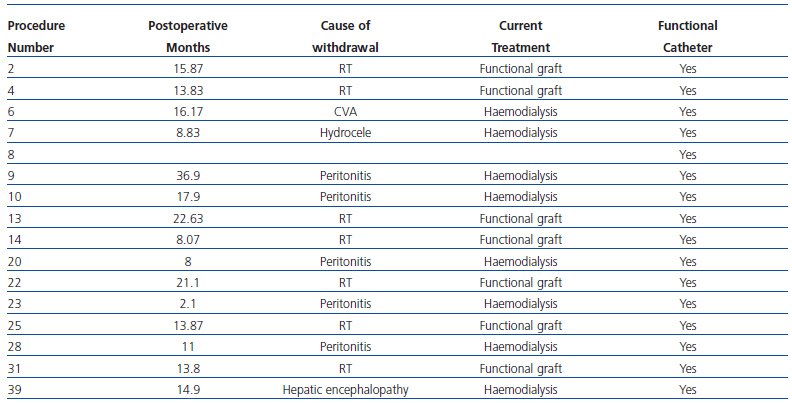
There were no leakages of peritoneal fluid or surgical wound infections during the immediate postoperative period (< 48 h). There were no cuff extrusions or eventrations. The catheter obstruction rate was 7.8%, and catheter migration rate was 4% (2 patients). One of these patients required catheter removal due to severe peritonitis. In the other case, the catheter did not result in obstruction or peritonitis, and worked correctly.
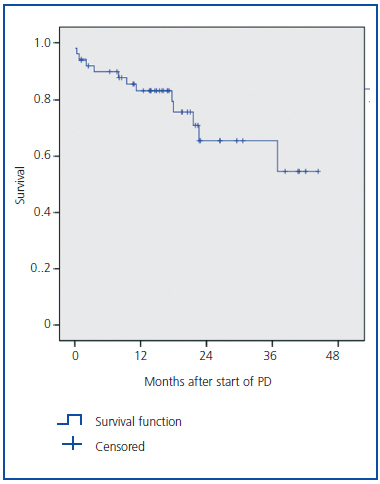
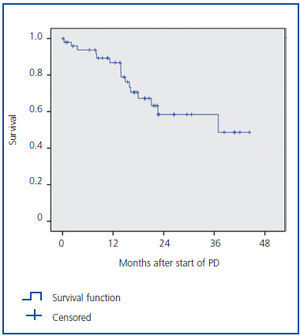
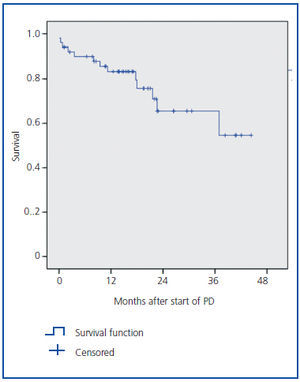
A total of three patients died, an average of 16 months after catheter placement (2.35 deaths per 1,000 patient/month of exposure). The causes of death were cardiovascular complications secondary to end-stage renal disease. Mortality was not related to PD or to the catheter. The survival curves of patients on PD are shown in Figure 3, and the survival curve of the catheters in Figure 4. A total of three catheters (5.9%) had to be removed due to peritonitis, all working properly. According to our experience, we had 0.27 episodes of peritonitis per patient/year.
Two catheters were removed because of technical complications in the postoperative period. In the first case, the patient developed abdominal pain that required exploratory laparotomy and it appeared that the catheter was lying in a loop of intestine. After verifying that the bowel loop was viable, the catheter was removed and a new one placed. The patient is currently in the PD program. The second patient, nine months after surgery, presented with canalisation of a peritoneum-vaginal tract and developed a hydrocele. The patient refused surgical correction and was transferred to the haemodialysis programme.
DISCUSSION
PD is a safe and effective option for patients with end-stage renal disease. Furthermore, there is evidence of better preservation of residual renal function when compared with haemodialysis.27,28 Although open surgery has been the method of choice, the laparoscopic approach has been widely accepted.29-31
Our technique, described above, is a simple procedure through two 12mm trocars. Furthermore, it is a very fast procedure, with a short operative time. Regarding the intraoperative advantages, laparoscopy allows for optimal visualisation and evaluation of the peritoneal cavity, allowing precise catheter placement. Furthermore, laparoscopy allows for release of peritoneal adhesions if necessary.
The use of a Guyon guide has been very helpful for accurate placement of the catheter, as the atraumatic tip and rigidity make it possible to both guide the catheter to the pouch of Douglas and reposition it if necessary. The incidence of catheter obstruction in the literature varies between 10% and 22% in open surgical procedures with blind placement. On the other hand, laparoscopic surgery has much lower obstruction rates of between 4% and 13%. Based on our experience, the obstruction rate was 3.9%. Despite this low rate, we must bear in mind our limited follow-up. Peritoneal leakage rates range from 2.6% to 22%. In our experience, we have not had any leakage. This complication is not only associated with open surgery, but also with the laparoscopic approach. Paramedial placement and the creation of a long subcutaneous tunnel are strategies for attempting to reduce this complication32,33 and may explain the absence of fistula in our series.
In analysing our technique compared to other three-port laparoscopic techniques, our experience is comparable in terms of surgical time, hospitalisation time, and catheter obstruction rate.30,34,35 The rates of peritoneal fluid fistula with three-port techniques vary between 0% and 4.7%. Accepting our limited follow-up, our results are at least equal.25,30 We have had no cases of surgical wound infection. It could be argued that a short operating time is important to limiting wound infections, but other centres with similar surgical times report port infection rates of up to 21%.35
We did not have peritonitis in the early postoperative period (first two weeks) after implantation of the catheter but we did have one episode of peritonitis per patient every 32.4 months (0.27 episodes per patient year), which is lower than suggested in the literature.36 More follow-up is needed to determine the risk of peritonitis associated with our technique.
In short, we believe that our technique is a simple and rapid procedure with few complications and short hospitalisation time, due to its reliability and excellent results in terms of catheter function.
Figure 1. Oreopoulos-Zellerman catheter with Guyon guide with atraumatic tip.
Figure 2. Position of ports. Periumbilical 12mm port for the catheter and left pararectus port with 12mm optics.
Figure 3. KM curve showing the survival of peritoneal dialysis patients.
Figure 4. Catheters removed or replaced due to technical problems (obstruction, peritonitis or migration).
Table 1. Patients excluded from the CAPD programme. Cause of exclusion, time since start, current treatment, and catheter status at time of exclusion