To the Editor:
The most common complications following late kidney transplantectomy are intra- and postoperative haemorrhages and surgical wound infections. Lesions produced in the iliac vessels have also been described.1
The incidence of pseudoaneurysms in the kidney transplantectomy bed is low, with very few cases reported in the medical literature.2-7 The treatment of these pseudoaneurysms using endovascular procedures is considered to be a relatively novel approach.
We present the case of a 51-year-old patient with hypertension and terminal chronic renal failure due to mesangial IgA glomerulonephritis, who sought emergency care due to diffuse abdominal pain with one week evolution, and which had intensified and focalised in the right iliac fossa during the previous 24 hours, accompanied by sweating, nausea, and vomiting.
The patient had received a heterotopic kidney transplant in the right iliac fossa in 1998. The graft failed due to the development of a non-Hodgkin’s lymphoma, leading to a nephrectomy of the transplanted kidney in 1999, with the patient returning to haemodialysis. Three years later, the patient received a second kidney transplant in the left iliac fossa, for which the immunosuppression regimen consisted of prednisone, mycophenolate mofetil, and sirolimus.
Upon arrival in the emergency department, the patient suffered somnolence and haemodynamic instability. A physical examination revealed a distended abdomen resembling peritonitis, producing intense pain upon palpation in the right iliac fossa.
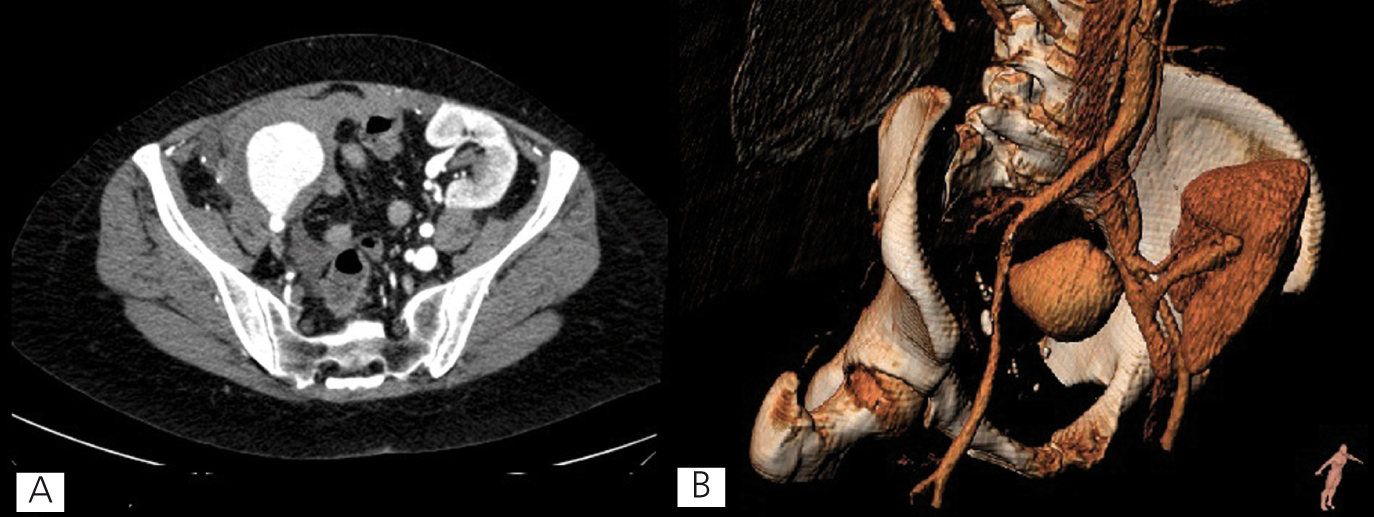
Initial laboratory analyses revealed anaemia at 4 points lower than baseline haemoglobin values. In addition, an abdominal ultrasound revealed haemoperitoneum of an unknown origin. The patient underwent an abdominal computerised tomography using contrast dye. This test revealed the transplanted kidney in the left iliac fossa with a pseudoaneurysm of 4.4x5x5.2cm (transverse, antero-posterior, and craniocaudal diameters) whose neck was dependent to the right external iliac artery and abundant haemoperitoneum around the liver and spleen, both paracolic gutters, and the pelvis, compatible with the signs of a ruptured pseudoaneurysm (Figure 1).
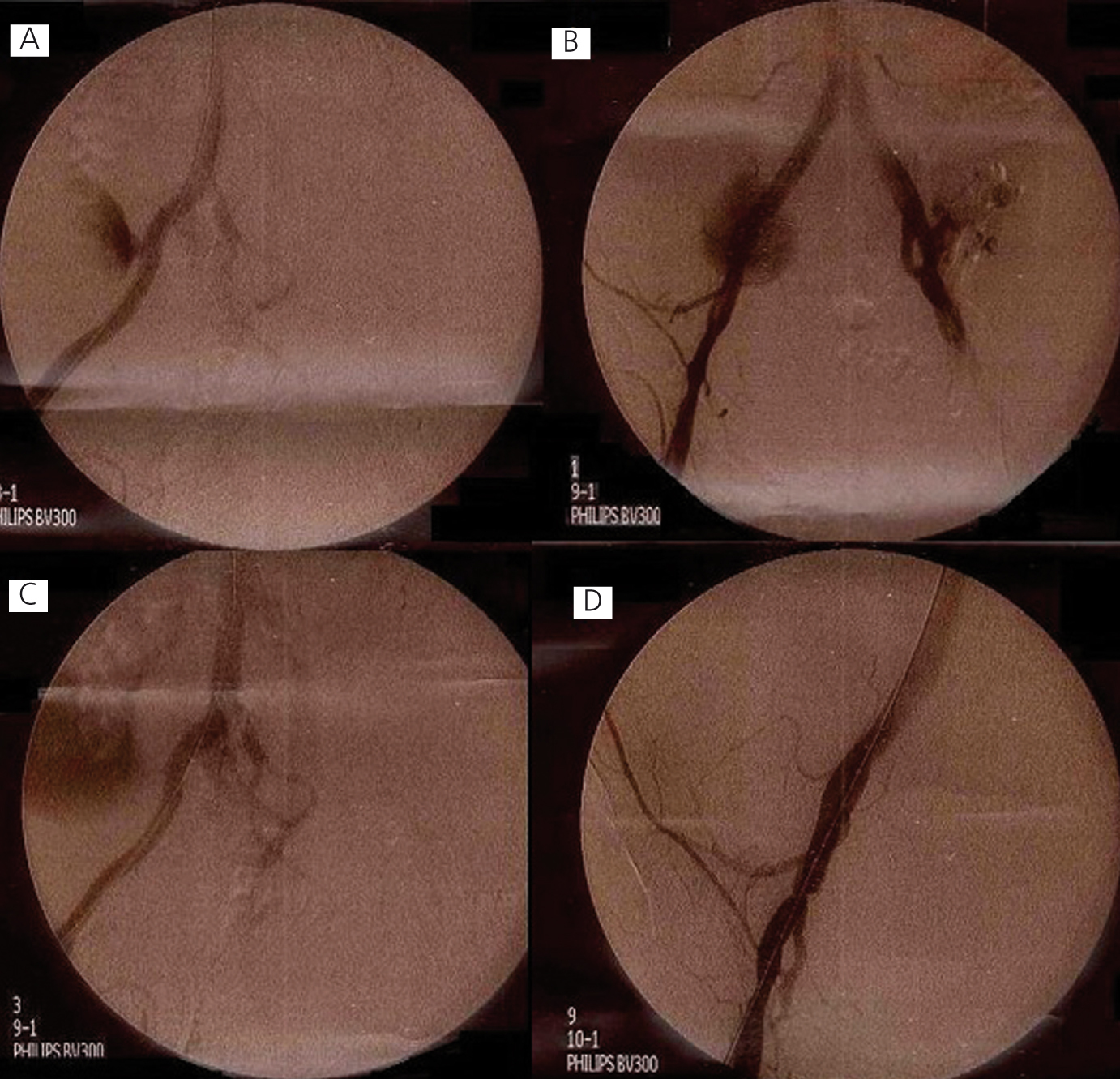
In light of these findings, we decided upon emergency repair of the pseudoaneurysm. Under local anaesthesia and sedation, we implanted a Viabahn® endo-prosthesis in the right common iliac artery, extending it into the external iliac artery. Angiographic control verified exclusion of the pseudoaneurysm with occlusion of the hypogastric artery. The procedure was completed with the placement of a Visi-Pro® stent distally of the endo-prosthesis due to an intimal defect (Figure 2). The patient was discharged from the hospital 8 days later, with no symptoms and recovered baseline renal function.
Discussion
The formation of an iliac pseudoaneurysm in the surgical kidney transplantectomy bed is extremely rare. Very few cases have been published in the medical literature, with an estimated incidence <1%, most commonly in patients with hypertension and dyslipidaemia.8 Several different causes of iliac pseudoaneurysms have been described. In the context of kidney transplantectomy, it has been suggested that the origin lies in chronic rejection of residual blood vessels from the donated kidney that are present in the vascular stump, which degenerate until forming a pseudoaneurysm.5
The clinical manifestations are correlated with the compression of neighbouring structures: neurological or venous compression, obstruction of the large intestine, and ureteral obstruction.9 The natural progression of pseudoaneurysms is rupture, in which case the patient can enter into haemorrhagic shock accompanied by abdominal pain, nausea, vomiting, genital/urinary symptoms, and fever (especially in infectious pseudoaneurysms).
The diagnosis tends to be late due to the location deep within the pelvis, and may not be noticed until rupture. The imaging test of choice is angio-CT scan,10 which allows for visualising the origin of the pseudoaneurysm and the relationship with neighbouring structures as well as evaluating the possibility of endovascular treatment. A Doppler-ultrasound is useful for establishing a diagnosis, and angiography facilitates applying the treatment during the same procedure.
The traditional treatment for an iliac pseudoaneurysm is open surgery through resection and insertion of a prosthesis. The procedure is quite complex due to the location of the iliac arteries deep within the pelvis, producing a 10% mortality rate.4 In ruptured iliac aneurysms that require emergency open surgical repair, higher morbidity rates have been reported due to ureteral lesions, postoperative haemorrhage, and laparostomy.11 Additional technical difficulties are inherent to residual pseudoaneurysms, since the surgeon must dissect a fibrotic surgical field as a result of previous operations, increasing the risk of injury.
Endovascular treatment provides a quick, safe, and effective treatment alternative, given the reduced invasiveness and no need for general anaesthesia, with comparable results to those from traditional surgical approaches.12 Even so, the procedure requires assistance using costly imaging techniques that utilise radiation and contrast dye.
Conclusions
To conclude, in patients with a ruptured iliac pseudoaneurysm as a late complication of a kidney transplantectomy, endovascular repair can be a valid, effective, and safe treatment alternative, even for emergency cases.
Conflicts of interest
The authors have no conflicts of interest to declare.
Figure 1. Abdominal computerised axial tomography
Figure 2. Angiography