We often find ourselves faced with the dilemma of whether or not to accept an apparently non-optimal kidney in a patient who has been on dialysis and wants to have a transplant. The assessment of the “quality” of the kidney remains controversial. The simplest concept is age. Donor age is a factor limiting the survival of the kidney, and although we know that the older the age, the poorer the survival,1 we also know that kidneys from older people can be beneficial for patients when compared with their time on dialysis without a transplant.2,3
In the early 2000s, a concept was developed in the US called expanded criteria donor (ECD), where in addition to age, 3 other clinical variables were included: a history of high blood pressure, a preoperative serum creatinine test, and cause of death (i.e. whether cerebrovascular or otherwise).4 An ECD kidney had a survival between 70% and 168% worse than a kidney from a standard-criteria donor (SCD). For over a decade, everyone has used this distinction, although in Spain it has never reached the point of developing a specific informed consent for this kind of kidney, which in many programmes constitute over half of those available. In our healthcare setting, the use of the ECD-SCD distinction has been limited to scientific issues, with no real effect on clinical care. Interestingly, in the US as well as in Spain, the most common reason for not using a removed kidney is based on the histological study in the pre-implant biopsy, which provides no parameters for the ECD-SCD comparison.5 The correlation between the histological findings, particularly the percentage of glomerulosclerosis and graft and patient survival, is limited and does not justify the widespread use of it for making decisions about the importance of whether or not to accept a kidney for transplantation. The simple fact of variation in the findings between different pathologists examining the biopsy illustrates the significant limitation of these parameters.6
In an attempt to improve the predictive ability of the ECD-SCD classification based on 4 variables, the US system of donation and transplantation has developed the Kidney Donor Risk Index (KDRI), based on 10 variables.7 These variables (all clinical ones) include the 4 above, plus weight, height, race, history of diabetes, hepatitis C virus blood test, and whether the donor's heart stopped. The KDRI is easily obtained, with a readily available calculator.8 As was the case with the concept of ECD, it does not include any clinical parameter of donor-recipient compatibility, nor any laboratory parameter except serum creatinine, or any parameter regarding the kidney, such as macroscopic appearance, arteriosclerosis or histopathology. Major decisions in this area should be made after a more comprehensive analysis.9 The parameters included in the KDRI are only the various clinical characteristics significantly related to graft survival in an analysis of nearly 70,000 donors used between the years 1995 and 2005. Interestingly, an attempt to improve KDRI by adding factors that often are not well known at the time of making the decision to accept or reject the kidney, such as ischaemic time, HLA match or machine perfusion parameters, did not improve the discriminative power.10 The index assigns the value of 1.00 to the median value (50th percentile) of donors from the previous year, thus a value <1.00 indicates the best kidney, and a value >1.00, worse than the median kidney from the previous year. The KDRI value estimates the risk of loss of kidney with respect to the median kidney, therefore a kidney with a KDRI value of 1.40 will have a risk of loss 1.4 times above the median kidney from the previous year in the US.
The Kidney Donor Profile Index (KDPI) is an accumulated extrapolation of the KDRI, such that kidney quality is transferred to a scale from 0% to 100%: a KDPI of 80% assigned to a given kidney means that 80% of the kidneys from the previous year have had better survival than actual kidney. The higher the KDPI, the “worse” is the kidney in terms of estimated survival, and vice versa (Table 1). The KDPI is not compared with any validated standard, but only with kidneys transplanted during the prior year in the US. The KDPI improves the limited discriminative ability of the ECD, by obtaining the information from a Cox model with 10 significant variables instead of 4, and in many cases, continuous and non-dichotomous variables. However, the value of C-statistic (area under the curve) is 0.60,10 which confers a poor discriminative value, considering acceptable only between 0.70 and 0.80.11 The most important variable in the calculation is age: a 20-year-old donor, of 80kg of weight, 180cm tall, white, with no hypertension or diabetes, who died by brain trauma and had a creatinine of 0.9, has a KDPI value of 2%; a donor with the same characteristics but who is 70 years old has a KDPI value of 82%.8 If that same 70-year-old donor has been hypertensive during the last 6 years of his life (which occurs in 70% of the Spanish population of that age), the KDPI value is 90%. Gender (male or female) has not been found to be significant in terms of discriminative value, and has not included in the final calculation.7,8Table 2 illustrates some cases.
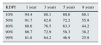
Renal graft survival according to the Kidney Donor Profile Index (KDPI) in the US, with transplants performed between 2004 and 2011.10
| KDPI | 1 year | 3 years | 5 years | 8 years |
|---|---|---|---|---|
| 10% | 94.4 | 88.1 | 80.6 | 68.1 |
| 50% | 91.7 | 82.6 | 72.2 | 55.9 |
| 80% | 88.6 | 76.5 | 63.3 | 44.2 |
| 90% | 86.7 | 72.9 | 58.3 | 38.2 |
| 99% | 81.8 | 64.2 | 46.9 | 25.9 |
Data (%).
Examples of KDPI using the Organ Procurement and Transplantation Network's calculator.8
| Donor | Characteristics | KDPI as a % |
|---|---|---|
| 1 | 20 years, weight 80, height 180, white, no HTN, no diabetes, serum Cr 0.9mg/dL, HCV-negative, death by brain trauma | 2 |
| 2 | 47 years, weight 78, height 173, white, no HTN, no diabetes, serum Cr 1.4mg/dL, HCV-negative, donor in asystole | 61 |
| 3 | 54 years, weight 72, height 166, white, HTN for 6 years, no diabetes, serum Cr 0.9mg/dL, HCV-negative, brain death | 77 |
| 4 | 70 years, weight 80, height 180, white, no HTN, no diabetes, serum Cr 0.9mg/dL, HCV-negative, death by brain trauma | 82 |
| 5 | 70 years, weight 80, height 180, white, HTN for 6 years, no diabetes, serum Cr 0.9mg/dL, HCV-negative, brain death by brain haemorrhage | 94 |
| 6 | 70 years, weight 72, height 166, white, HTN of unknown duration, no DM, serum Cr 0.9mg/dL, HCV-negative, brain death by brain haemorrhage | 97 |
| 7 | 65 years, weight 78, height 173, white, HTN for 1 year, no diabetes, serum Cr 1.4mg/dL, HCV-negative, postinfarct donor in asystole | 97 |
| 8 | 65 years, weight 72, height 166, white, hypertension for 6 years, type II diabetes for 2 years, serum Cr 0.8mg/dL, HCV-negative, brain death by brain haemorrhage | 98 |
| 9 | 72 years, weight 72, height 166, white, hypertension for 6 years, type II diabetes for 2 years, serum Cr 0.8mg/dL, HCV-negative, brain death by brain haemorrhage | 100 |
| 10 | 75 years, weight 78, height 169, white, hypertension for 12 years, no diabetes, serum Cr 1.3mg/dL, HCV-negative, brain death by brain haemorrhage | 100 |
The KDPI, besides being incorporated as a tool to comparatively estimate renal survival, KDPI has been used recently in the US to match kidneys with a KDPI <20% (theoretically the best) to 20% of waitlist recipients with a higher-than-expected survival.12 The expected survival is calculated by the Estimated Post Transplant Survival (EPTS), which also ranges from 0% to 100%: candidates with a lower EPTS presumably will last more years with renal function. For this purpose, another calculator has been developed, which includes 4 clinical variables (age, years on dialysis, diabetes [yes/no] and prior transplant [yes/no]).13 For example, a 48-year-old patient on dialysis for 3 years, with no diabetes or previous transplants, has a EPTS of 21%, so this patient will no longer benefit from receiving a kidney with a KDPI value of <20%, since survival “would not be sufficient” to obtain a kidney of such quality.
Would the KDPI be useful in Spain?The major limitation of the KDPI in its application in settings other than US is evident: it only estimates which percentage of kidneys are removed and implanted in the US during the previous year are worse or better than the specific kidney analysed at a current time. Therefore, it cannot be extrapolated to other countries or transplant programmes where the strategies for the use of organs are not the same and even clinical outcomes are very different.14 In the US only 5% of donors whose kidneys were transplanted in 2014 were over 65, and the percentage was even smaller than during the 10 years earlier.15 In Spain, 32.4% of donors in 2015 were 70 years or older, and only 46.8% were under 60.16 In the US the rate of kidneys removed and rejected is very high, especially among ECD kidneys or with a high KDPI (65% discarded post-extraction if KDPI >90%).17 These percentages have not changed after KDPI has extended the criteria for evaluation.18 Although in Spain this percentage is lower,19 it is likely that the fundamental difference takes place before organ extraction, since the number of ECD donors or with a high KDPI who are considered valid in the US is lower than in Spain, at least for going to and analyse the kidney once removed. It is interesting to note that in the US, more than 30% of recipients in the waiting list that are 65 or older would not accept a kidney with KDPI >85%, when 100% of patients eligible for transplants would have a KDPI of >85% if they were donors. Also, the number of patients in the waiting list is 5 times higher (86,965 candidates) than the number of transplants in 2013 (17,600),20 and the difference between candidates and transplanted continues to grow. The median transplant waiting time in the US is 6.5 years, and waitlist mortality is roughly 8 per cent per year. This means that approximately 50% of candidates die before being transplanted.15 In Spain, almost 60% of patients in the waiting list have a transplant every year.21 For years, there has been applied much wider criteria for acceptance of donors and kidneys.22 Thus transplant performance would not improve by adopting a rating system from such a different scenario.
The question of using KDPI as the main criterion to rule out a transplantable kidney also comes from the consistent demonstration that the kidneys with a high KDPI (even of 91–100%) confers survival benefits compared with waiting for dialysis of a kidney with a lower KDPI23; this is similar to what we have seen with kidneys from elderly patients in our setting.2,3
These radical differences indicate that the direct use of US-based KDPI in Spain would be a non advisable practice. Using US donors as a comparison, even though we do not have reliable Spanish data, the KDPI of Spanish donors can be estimated to be more than 80% in more than half, and close to 100% in more than 30%. It has been recently discussed that the KDPI should be validated in a European population since variables are available in many registries.24 We do not share this view. The, only idea that seems valid would be to find kidney quality index available based on known data on viability and survival. But such data cannot be extrapolated from settings that are so different from ours,25 as this often proves unsuccessful.26 An entirely different issue would be to develop a Spanish Kidney Donor Profile Index (SKDPI), which would necessarily be constructed from Spanish data, combining clinical variables from donors with medium- and long-term outcomes in recipients. Some patient registries accumulate enough data to build indexes of this type, which may be more useful in guiding decisions.
Please cite this article as: Pascual J, Pérez-Sáez MJ. El Kidney Donor Profile Index: ¿se puede extrapolar a nuestro entorno? Nefrologia. 2016;36:465–468.