Dear Editor,
mTOR inhibitors are immunosuppressors that block proliferation signal and have a lower nephrotoxic potential. However, a series of adverse reactions have been described, especially with sirolimus, among which the most outstanding is pneumonitis.
We present the case of a 70 year old man, suffering from hypertension and dyslipidaemia, who received his first kidney transplant from a deceased donor in March 2009, due to chronic kidney disease secondary to chronic pyelonephritis. Immunosuppressive treatment consisted of basiliximab, mycofenolate, everolimus and steroids. The patient presented good evolution, with creatinine on discharge at 1.7 mg/dl.
The patient is admitted 4 months after transplant surgery with a fever over 10 days, cough and dyspnoea. On physical examination poor general condition is noted with chills, tachycardia, bilateral crepitation and oxygen saturation of 93% (arterial blood gas: pH 7.50, pCO2 26.8, pO2 60, HCO3 20.9 mmol/l). The patient also presented non-pruriginous erithematous exanthema on the back and chest, with lip herpes.
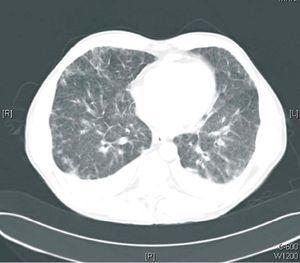
Laboratory findings were 3,980 WBC/µl (eosinophils 29.3%), haemoglobin 12.1 g/dl, platelets 276,000, creatinine 1.79 mg/dl, plasma sodium 138 mEq/l, plasma potassium 3.9 mE/l, and plasma levels of everolimus of 14 ng/ml. On the chest X-ray a bilateral interstitial pattern was seen and the chest CT showed pulmonary nodules and infiltrates with thickening of the bilateral interstitium (Figures 1 and 2). Antigen studies and cultures of cytomegalovirus (CMV) were negative, as also pneumococcal and Legionella antigen studies. A bronchoscopy was performed and signs of chronic bronchopathy were seen with negative BAl and BAS. Empiric treatment with wide spectrum antibiotics and antivirals was begun, without any clinical improvement and with radiological worsening. Therefore, suspecting pneumonitis due to everolimus, we decided to discontinue this drug and introduce tacrolimus. On the day after discontinuing everolimus the patient presented clinical and radiological improvement with resolution of the condition.
To summarise, knowing that pneumonitis may appear with all mTOR inhibitors can lead to rapid discontinuation of the drug, preventing unnecessary diagnostic and therapeutic action in kidney transplant patients.
Figure 1. Chest X-ray
Figure 2. Chest CT