Hypertension is a highly prevalent disorder among patients undergoing haemodialysis. It contributes to greater cardiovascular risk and must be controlled. However, despite dietary measures, haemodialysis regimen optimization and pharmacological treatment, some patients in our units continue to maintain high blood pressure levels. The objective of the study is to demonstrate that reducing calcium in dialysis fluid can help treat hypertension patients undergoing haemodialysis.
Material and methodsWe selected all of the hypertensive patients from our haemodialysis unit. We checked their normovolemic status by means of bioimpedance spectroscopy, decreasing the haemodialysis fluid's calcium concentration to 2.5mEq/L, with a follow-up period of 12 months.
ResultsA total of 24 patients met the non-volume dependent hypertension criteria (age 61±15 years, males 48%, diabetes 43%). A significant systolic and diastolic blood pressure decrease was observed at 6 and 12 months as a result of reducing the dialysis calcium concentration; this was not accompanied by greater hemodynamic instability (baseline systolic blood pressure: 162±14mmHg; at 6 months: 146±18mmHg; at 12 months: 141±21mmHg; p=0.001) (baseline diastolic blood pressure: 76±14mmHg; at 6 months: 70±12mmHg; at 12 months: 65±11mmHg; p=0.005). A non-significant increase in plasma parathyroid hormone levels was also found. No side effects were observed.
ConclusionsAdding 2.5mEq/L of calcium to dialysis fluid is a safe and effective therapeutic alternative to control hard-to-manage hypertension among haemodialysis patients.
La hipertensión arterial es altamente prevalente en los pacientes en hemodiálisis. Implica un mayor riesgo cardiovascular y es fundamental su control. A pesar de medidas dietéticas, optimización de la pauta de hemodiálisis y tratamiento farmacológico, existe un porcentaje de pacientes en nuestras unidades que continúan hipertensos. Es por ello que nos planteamos que la reducción de calcio en el líquido de diálisis puede ayudar al manejo de los pacientes hipertensos en hemodiálisis.
Material y métodosSe seleccionaron todos los pacientes hipertensos de nuestra unidad de hemodiálisis. Se comprobó estado de normovolemia mediante bioimpedancia espectroscópica y se disminuyó la concentración de calcio del líquido de hemodiálisis a 2,5mEq/l, con un seguimiento de 12 meses.
ResultadosCumplieron criterios de hipertensión arterial no volumen-dependiente 24 pacientes (edad 61±15 años, varones el 48%, diabetes el 43%). Se observó una disminución significativa en la tensión arterial sistólica y diastólica a los 6 y 12 meses de la reducción de la concentración del calcio de diálisis, sin acompañarse de mayor inestabilidad hemodinámica (tensión arterial sistólica basal 162±14; a los 6 meses 146±18; a los 12 meses 141±21mmHg; p=0,001) (tensión arterial diastólica basal 76±14; a los 6 meses 70±12; a los 12 meses 65±11mmHg; p=0,005) Existió un aumento de los niveles plasmáticos de PTH de forma no significativa. No se evidenciaron efectos secundarios.
ConclusionesLa hemodiálisis con calcio en el líquido de 2,5mEq/l es una alternativa terapéutica eficaz y segura para el control de hipertensión arterial de difícil manejo en los pacientes de hemodiálisis.
There is a high prevalence of hypertension (HTN) in hemodialysis patients that varies from 56% to 90% depending on the series reported.1–5 Hypertension is an important risk factor for cardiovascular morbidity and mortality and cardiovascular events are the main cause of death in the dialysis population.6,7
The pathogenesis of hypertension in hemodialysis is multifactorial, but it is mainly related to the expansion of extracellular volume (ECV).8–10 Other factors also involved are the activation of the renin-angiotensin system, the sympathetic system activity or the reduced synthesis of nitric oxide.11
The control of volume by means of ultrafiltration and appropriate adjustment of dry weight, the restriction of salt intake and the reduction of sodium concentration in the dialysis bath are the first step for the control of blood pressure (BP) in these patients. Yet, despite the pharmacological treatment, in many in hemodialysis patients the HTN is refractory.
There is no uniformity about the appropriate calcium concentration in the dialysis fluid. The use of a calcium concentration of 2.5mEq/L reduces the calcium balance as compared with the 3mEq/L and may induce an increase in PTH, together with other effects such as a decrease in BP.12,13
Elevated calcium levels have been associated with hypertension, however the mechanisms by which variations in ionic calcium influence the BP independently of extracellular volume and changes in electrolytes are poorly understood. Different mechanisms of action have been postulated, among which are the increased vasoconstriction and myocardial contractility.14–17
The aim of our study is to analyze the effect that changes in the calcium concentration of dialysis fluid exert on BP in normovolemic hemodialysis patients, during a 12-month follow-up.
Material and methosDesignThis is a prospective, interventional study, before–after in a single group.
PatientsFrom a total of 75 prevalent elderly patients of the Hemodialysis Unit of the Gregorio Marañón Hospital, we selected all non-volume-dependent hypertensive patients during a 9-month recruitment period. Hypertension was defined as pre-dialysis BP values greater than 140/90mmHg during the previous month or the need for antihypertensive drugs to control BP independently of the actual values of BP. Patients were informed of the study and written informed consent was obtained. The exclusion criteria were the voluntary refusal to participate in the study and the failure to meet the criteria for HTN. Finally, 24 patients were selected.
All patients were on a regime of 3 weekly sessions of conventional hemodialysis or on-line hemodiafiltration, of 240min duration. The dialysis fluid had a calcium concentration of 3mEq/L and a conductivity of 13.8mS/cm.
Data collectionAll data was collected at baseline, 3, 6 and 12 months. The variables were the BP values, number of antihypertensive drugs, number of episodes of arterial hypotension in each dialysis session, interdialysis weight gain, predialysis plasma levels of calcium, phosphorus and PTH, and treatment for control of calcium and phosphate metabolism. The values of predialysis BP and the interdialysis weight gain were collected as the average of the values obtained during the week prior to collection. The episodes of intradialytic arterial hypotension collected were the symptomatic episodes that required fluid therapy or a decrease in the ultrafiltration rate during the month prior to the data collection.
The blood volume was measured by bioimpedance at baseline, 6 and 12 months, using a spectroscopic bioimpedance monitor (BCM, Fresenius Medical Care, Bad Homburg, Germany). Overhydration (OH) and total body water (TBW) were measured. OH is defined as water not included in lean or fat tissue. Normal hydration is defined as a OH/VEC ratio less than 15% before the hemodialysis session, as previously defined in the literature.18,19 All patients included in the study met the criteria of normal hydration and therefore it was considered that these patients had non-volume-dependent hypertension.
Follow upThe calcium concentration of the dialysis fluid was reduced in all patients to 2.5mEq/L and this concentration were maintained throughout the follow-up. The baseline data was compared with the data collected at 3, 6 and 12 months. The reasons for not completing the study were: kidney transplant, death or need to modify the calcium concentration in the dialysis fluid due to medical criteria, hypocalcemia or development of severe secondary hyperparathyroidism.
Statistic analysisThe data of the quantitative variables are expressed as means±standard deviation or median±Interquartile range depending on the distribution of the variable. Qualitative variables are described as frequencies. The variables were compared using the t-student test and nonparametric tests (Wilcoxon signed rank test and McNemar test), depending on the nature of the variables. A statistically significance was considered if p value was lower than 0.05. The statistical analysis performed using SPSS V. 17.0. (Chicago, IL, USA)
ResultsOf the 75 patients prevalent in the Hemodialysis Unit 24 met the criteria to be included in the study, these represents a 32% of HTN in our Hemodialysis Unit.
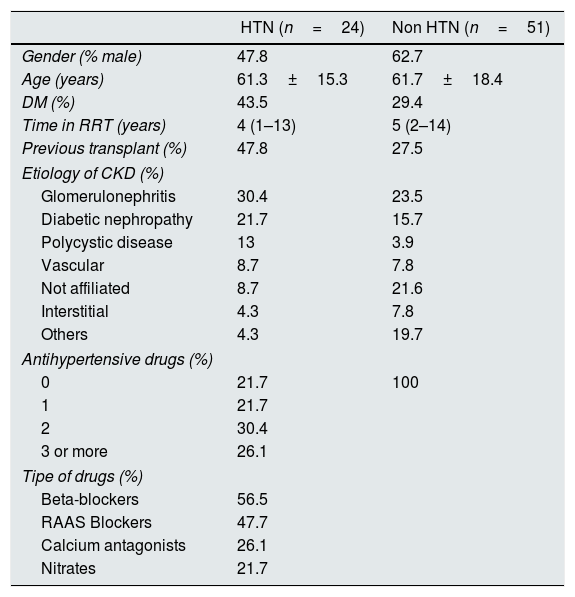
The baseline characteristics of the 24 hypertensive patients and the 51 non-hypertensive patients are described in Table 1.
Baseline characteristics of hypertensive and non-hypertensive patients (values are expressed in percentages, except for time on renal replacement therapy shown as median and interquartile range and age in mean±standard deviation).
| HTN (n=24) | Non HTN (n=51) | |
|---|---|---|
| Gender (% male) | 47.8 | 62.7 |
| Age (years) | 61.3±15.3 | 61.7±18.4 |
| DM (%) | 43.5 | 29.4 |
| Time in RRT (years) | 4 (1–13) | 5 (2–14) |
| Previous transplant (%) | 47.8 | 27.5 |
| Etiology of CKD (%) | ||
| Glomerulonephritis | 30.4 | 23.5 |
| Diabetic nephropathy | 21.7 | 15.7 |
| Polycystic disease | 13 | 3.9 |
| Vascular | 8.7 | 7.8 |
| Not affiliated | 8.7 | 21.6 |
| Interstitial | 4.3 | 7.8 |
| Others | 4.3 | 19.7 |
| Antihypertensive drugs (%) | ||
| 0 | 21.7 | 100 |
| 1 | 21.7 | |
| 2 | 30.4 | |
| 3 or more | 26.1 | |
| Tipe of drugs (%) | ||
| Beta-blockers | 56.5 | |
| RAAS Blockers | 47.7 | |
| Calcium antagonists | 26.1 | |
| Nitrates | 21.7 | |
DM: diabetes mellitus; CKD: chronic kidney disease; RAAS: renin-angiotensin-aldosterone system; RRT: renal replacement therapy.
Throughout the 12 months of follow-up, of the 24 patients included, 23 were studied at 6 months and 18 completed one year follow-up. The causes of exclusion from the study were 3 transplants, one death due to cerebrovascular accident and in 2 patients, the Ca concentration in the dialysis fluid was modified to 3mEq/L by decision of their responsible physician based on the presence of hypocalcemia and marked secondary hyperparathyroidism.
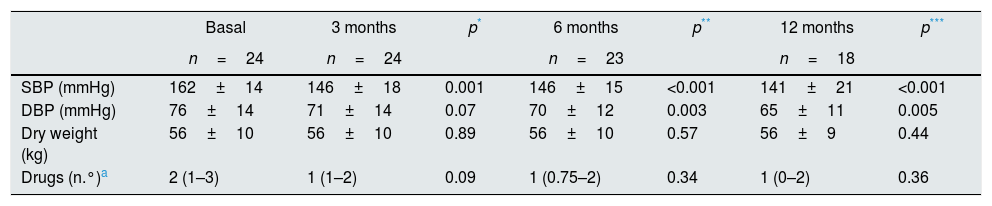
In the HTN group, the initial mean predialysis systolic BP was 162.0±14.9mmHg and the average diastolic BP was 76.7±14.7mmHg. Systolic and diastolic BP decreased significantly at 12 months of follow-up. This occurred while the dry weight was maintained and with a non significant reduction in the number of antihypertensive drugs (Table 2).
Comparison of values of BP, dry weight and antihypertensive drugs at baseline, 3, 6 and 12 months.
| Basal | 3 months | p* | 6 months | p** | 12 months | p*** | |
|---|---|---|---|---|---|---|---|
| n=24 | n=24 | n=23 | n=18 | ||||
| SBP (mmHg) | 162±14 | 146±18 | 0.001 | 146±15 | <0.001 | 141±21 | <0.001 |
| DBP (mmHg) | 76±14 | 71±14 | 0.07 | 70±12 | 0.003 | 65±11 | 0.005 |
| Dry weight (kg) | 56±10 | 56±10 | 0.89 | 56±10 | 0.57 | 56±9 | 0.44 |
| Drugs (n.°)a | 2 (1–3) | 1 (1–2) | 0.09 | 1 (0.75–2) | 0.34 | 1 (0–2) | 0.36 |
BP: blood pressure; DBP: diastolic blood pressure; SBP: systolic blood pressure.
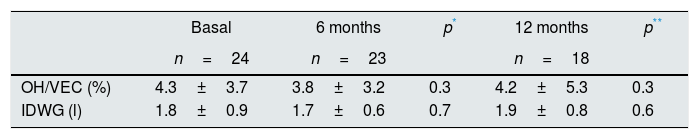
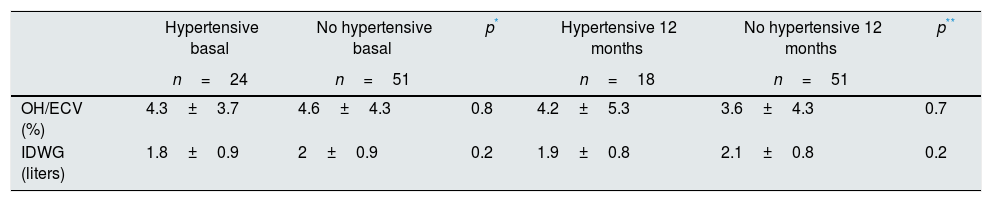
Analysis the data obtained by bioimpedance revealed that all the hypertensive patients included were normovolemic with a mean of the baseline predialysis OH/TBW ratio of 4.3±3.7%. Throughout the study, there were no significant changes in the hydration status or interdialysis weight gain in these hypertensive patients (Table 3). The baseline data of hypertensive patients were compared with the obtained in the 51 non-hypertensive patients and no significant differences were found regarding hydration status or interdialysis weight gain (Table 4).
Comparison of OH/ECV ratio measured by BIS and interdialysis weight gain, at baseline, 6 and 12 months.
| Basal | 6 months | p* | 12 months | p** | |
|---|---|---|---|---|---|
| n=24 | n=23 | n=18 | |||
| OH/VEC (%) | 4.3±3.7 | 3.8±3.2 | 0.3 | 4.2±5.3 | 0.3 |
| IDWG (l) | 1.8±0.9 | 1.7±0.6 | 0.7 | 1.9±0.8 | 0.6 |
IDWG: inter dialysis weight gain; OH/VEC: ratio between overhydration and extracellular volume.
Comparison of the OH/ECV ratio and interdialysis weight gain in hypertensive vs. non-hypertensive patients at baseline and at 12 months.
| Hypertensive basal | No hypertensive basal | p* | Hypertensive 12 months | No hypertensive 12 months | p** | |
|---|---|---|---|---|---|---|
| n=24 | n=51 | n=18 | n=51 | |||
| OH/ECV (%) | 4.3±3.7 | 4.6±4.3 | 0.8 | 4.2±5.3 | 3.6±4.3 | 0.7 |
| IDWG (liters) | 1.8±0.9 | 2±0.9 | 0.2 | 1.9±0.8 | 2.1±0.8 | 0.2 |
IDWG: interdialysis weight gain; OH/ECV: ratio between overhydration and extracellular volume.
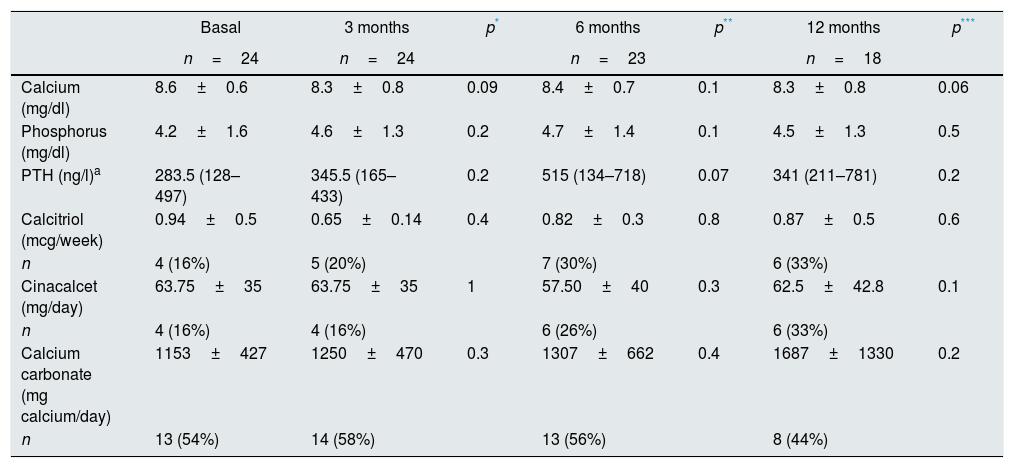
Table 5 shows the data on calcium and phosphate metabolism in hypertensive patients on hemodialysis with a dialysate containing 2.5mEq/L of calcium during 12 months follow up. There were no significant changes in the plasma levels of calcium and phosphorus throughout the study. PTH levels increase at 6 months although the increase was not statistically significant. At baseline, 4 patients (16.7%) were in treatment with calcitriol and the same percentage received cinacalcet; 13 patients (54.2%) required calcium based binders and 10 (41.7%) non-calcium binders. There were no significant differences in calcium intake, or in the doses of calcitriol and cinacalcet throughout the study.
Baseline data of mineral metabolism and the changes in serum levels of calcium, phosphorus and PTH as well as in the treatment for secondary hyperparathyroidism at baseline, 3, 6 and 12 months.
| Basal | 3 months | p* | 6 months | p** | 12 months | p*** | |
|---|---|---|---|---|---|---|---|
| n=24 | n=24 | n=23 | n=18 | ||||
| Calcium (mg/dl) | 8.6±0.6 | 8.3±0.8 | 0.09 | 8.4±0.7 | 0.1 | 8.3±0.8 | 0.06 |
| Phosphorus (mg/dl) | 4.2±1.6 | 4.6±1.3 | 0.2 | 4.7±1.4 | 0.1 | 4.5±1.3 | 0.5 |
| PTH (ng/l)a | 283.5 (128–497) | 345.5 (165–433) | 0.2 | 515 (134–718) | 0.07 | 341 (211–781) | 0.2 |
| Calcitriol (mcg/week) | 0.94±0.5 | 0.65±0.14 | 0.4 | 0.82±0.3 | 0.8 | 0.87±0.5 | 0.6 |
| n | 4 (16%) | 5 (20%) | 7 (30%) | 6 (33%) | |||
| Cinacalcet (mg/day) | 63.75±35 | 63.75±35 | 1 | 57.50±40 | 0.3 | 62.5±42.8 | 0.1 |
| n | 4 (16%) | 4 (16%) | 6 (26%) | 6 (33%) | |||
| Calcium carbonate (mg calcium/day) | 1153±427 | 1250±470 | 0.3 | 1307±662 | 0.4 | 1687±1330 | 0.2 |
| n | 13 (54%) | 14 (58%) | 13 (56%) | 8 (44%) |
a Expressed as median and interquartile range.
Hemodynamic instability intradialysis was not increased by a dialysate calcium of 2.5mEq/L; the percentage or the number of hypotension episodes were not increased (p=1 and p=0.7 respectively). Seven patients (29.2%) had at least one episode of symptomatic hypotension intradialysis during the month being dialyzed with Ca 3mEq/L, in number of 1 (12.5%), 2 (12, 5%) and 3 or more (4.2%). The same percentage also had at least one intradialytic arterial hypotension while being dialyzing with Ca 2.5mEq/L, in number of 1 (16.7%), 2 (8.3%) and 3 or more (4.2%).
Of the 18 patients who complete the study, 10 achieve the goals of predialysis TA less than 140/90mmHg, although most of them still required some antihypertensive drug.
DiscussionIn our study, the decrease in dialysate calcium concentration in hemodialysis patients is able to reduce the BP in patients with non-volume-dependent hypertension without changes in intradialysis hemodynamic stability, although with a non-significant tendency to increase the levels of PTH.
The hypertension is a frequent and relevant clinical problem in hemodialysis patients. It implies a greater cardiovascular risk and it is difficult to manage.6,7 In these patients, hypertension is fundamentally volume-dependent, which is why the first step in the control of BP is the correct adjustment of the dry weight.8–10 For this, in addition to the clinic, we currently have the fundamental aid of bioimpedance, which allows the quantitative determination of hydration status.20,21
It is noteworthy that the initial prevalence of hypertension in our Hemodialysis Unit (32%) is very low as compared to other series showing prevalence of hypertension of 56–90%.1–5 This is probably due to the maintained effort and conviction over the years about the importance of the control of ECV with dietary salt restriction, optimization of ultrafiltration, adequate quantification of the dry weight and individualizing the hemodialysis technique.
The default basal conductivity of our hemodialysis unit is 13.8mS/cm. The decrease or individualization of sodium in the dialysis fluid reduces thirst and the interdialysis weight gain and the BP.22
Despite the dietary advice, the adequate control of dry weight, the maintenance of patients in a normovolemic status and the individualization of the conductivity of the dialysis fluid, there is a percentage of patients who continue to be hypertensive. In this situation, we decided to analyze the effect of reducing the calcium concentration of the dialysis fluid on the BP. Our idea was to provide another tool for the treatment of hypertension in HD patients. With the data obtained from bioimpedance at the beginning of the study, we showed that all patients included in our study were in a situation of normal hydration. Wabel et al.18 established the cut-off threshold for the definition of OH by 15% in relation to the ECV, which represents an approximate excess of ECV of 2.5L. Based on this separation of patients in normally hydrated and overhydrated, a survival study was carried out with 269 prevalent hemodialysis patients and after a follow-up period of 3.5 years, it was found that the hydration status was an independent predictor of mortality in hemodialysis patients.19
After 12 months with a dialysis fluid calcium concentration of 2.5mEq/L, and maintaining the rest of the variables constant, it was observed a significant average reduction of 20.1mmHg in the predialysis systolic BP, which was already evident at the third month of study. However, the reduction of predialysis diastolic BP is more gradual and was significant only at sixth month, and at month 12, the average decrease was 11.7mmHg. These reductions in BP are not the result of better control of the patient hydration status, since the percentage of excess ECV (OH/ECV) or dry weight was not significantly modified throughout the study, neither it was the interdialysis weight gain. In addition to a better blood pressure control, there was a tendency to reduce the number of antihypertensive drugs, although this was not statistically significant.
Regarding the negative effects of hemodialysis with low calcium, it has been observed that the negative calcium balance during dialysis stimulates the secretion of PTH.23,24 Strict control of phosphate and calcium metabolism is important to avoid accelerated progression of secondary hyperparathyroidism in these patients. In our study, plasma phosphate levels remained unchanged, however plasma levels of calcium decreased discretely and PTH levels increased, although not statistically significant. The needs for calcium and phosphate binders were not significantly modified, although there was a tendency to increase the doses of calcium carbonate. It was observed an increase in the number of patients requiring calcitriol and cinacalcet for the control of secondary hyperparathyroidism, so that initially 16% of the patients were on calcitriol treatment and 16% on cinacalcet, and at month12 they were 33% respectively. If patients are dialysed with calcium of 2.5mEq/L, it is important to adjust the treatment correctly to maintain a strict control of plasma levels of calcium, phosphorus and PTH, so that unnecessary increases in PTH are avoided. The consequence may be an increase in the needs of calcium and vitamin D. Among our patients, there was a moderate increase in PTH, which, perhaps, could have been avoided with higher doses of calcium supplements or calcitriol. Other limitations of the study are that we have not confirmed the loss of calcium by convective transport; another limitation is the limited number of patients and a short follow-up period.
The effects of low calcium hemodialysis in terms of decreased myocardial contractility17,25 would be a contraindication for patients with severe heart disease and may result in worse tolerance for intradialytic arterial hypotension. In our study, where patients did not present severe cardiac disease, no greater hemodynamic instability was observed when patients were dialyzed with calcium of 2.5mEq/L compared to their baseline situation (Ca: 3mEq/L). Intradialysis hypotension is associated with an increase in morbidity and mortality.
In summary, hemodialysis with calcium in the dialysis fluid of 2.5mEq/L is an effective and safe therapeutic alternative for the control of non-volume-dependent hypertension in patients on hemodialysis. Its limitations are a stimulation of PTH secretion and a decrease in cardiac contractility, with a risk of a negative evolution of secondary hyperparathyroidism, an increase in calcium or vitamin D requirements, and an increased risk of intradialysis hemodynamic instability. Strict control of phosphate and calcium metabolism is required; the severe secondary hyperparathyroidism, severe heart disease and arrhythmias may contraindicate this treatment.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ampuero Mencía J, Vega A, Abad S, Ruiz Caro C, Verdalles Ú, López Gómez JM. Influencia de la concentración de calcio en el líquido de hemodiálisis sobre el control de la tensión arterial. Nefrologia. 2019;39:44–49.