Introducción: La eficacia en la práctica diaria de los captores de fósforo (P) está directamente relacionada con el cumplimiento terapéutico (CT) por parte del paciente. El objetivo de este estudio es evaluar el CT de los pacientes con hiperfosfatemia en hemodiálisis y su influencia sobre la fosfatemia durante 6 meses de seguimiento. Métodos: Se analizan 181 pacientes con P inicial >5 mg/dl. Se evaluó el CT con distintos captores, considerando paciente incumplidor aquel que reunía CT < 75 %, SMAQ (Simplified Medication Adherence Questionnaire) de «no cumplidor» (tabla 1) y un P > 5 mg/dl. Los pacientes que eran cumplidores en la visita basal (VB) salían del estudio; el resto continuaba hasta la V5 (6 meses). Se analiza el CT basal y en el seguimiento (V1-V5), los captores utilizados y la evolución de la fosfatemia en función de ellos. Resultados: Se estudian 103 hombres y 78 mujeres, media de edad 59,9 (21-86) años. El 39,2 % (n = 71) fueron cumplidores en la VB. Los pacientes mayores de 60 años eran cumplidores en mayor proporción que los más jóvenes (p = 0,019). En la tabla 6 se especifican las causas de no cumplimiento. El 60,8 % (n = 110), los no cumplidores, continuaron el estudio y una media del 27,2 % de estos se hicieron cumplidores a lo largo de las visitas. En la tabla 7 se muestra la relación de los niveles de P con el CT a lo largo de las visitas. Los niveles de P disminuyen 1,26 mg/dl de media al final del estudio (p < 0,0001). Conclusiones: Entre los pacientes en hemodiálisis con mal control del P existe un cumplimiento terapéutico con los captores de fósforo bajo, del 39,2 %. Con distintas estrategias se consigue mejorar el cumplimiento terapéutico y la fosfatemia. La disminución de P es mayor en los pacientes cumplidores que en los no cumplidores.
Background: The effectiveness of phosphate binders in daily practice is directly related to therapeutic compliance (TC) by the patient. The goal of this study was to analyse the TC of haemodialysis patients with hyperphosphatemia and its influence on serum phosphorus for 6 months follow up. Methods: 181 patients were included, who had mean initial phosphate levels (P) >5mg/dl. TC with different phosphate binders was evaluated, considering non-adherent patients those who had <75% of TC, SMAQ scale score of “non-adherent” (Table 1), and P>5mg/dl. Patients who were adherent at baseline visit (BV) left the study, the rest continued to V5 (6 months). TC at baseline and during the follow up (V1-V5) was analysed. Phosphate binders and the evolution of phosphataemia based on treatment were assessed. Results: 103 male and 78 female patients were evaluated, with a mean age of 59.9 (21-86) years. Of these, 39.2% (n=71) were adherent in the BV. Patients older than 60 years of age were more adherent than younger ones (P=.019).Table 6 specifies the causes of non-compliance. The remaining 60.8% of patients (n=110), were non-adherent and continued through to the end of the study. An average of 27.2% of these patients became adherent during the course of the study. Table 7 shows the relative levels of P with TC over successive visits. At the end of the study, mean P levels had decreased by 1.26mg/dl (P<.0001). Conclusion: Among HD patients with poor P level control, there is a low level of adherence with phosphorus binder treatment, at 39.2%. Compliance and phosphataemia are improved with different strategies. The decrease of P is higher in adherent patients than in non-adherent patients.
INTRODUCTION
Patients with chronic kidney disease (CKD) on haemodialysis (HD) who maintain phosphataemia at normal levels have a better prognosis than those with elevated levels.1-3 In order to control hyperphosphatemia in these patients, the first steps involve ensuring an appropriate dose of dialysis, avoiding elevated doses of vitamin D, and making proper diet recommendations (reduced intake of soft drinks, nuts, milk products, and protein), but in the majority of cases, phosphate binders (PB) are also needed to reduce absorption.
Despite these treatments, many patients on HD have poorly controlled phosphatemia.4 The causes of this difficulty in maintaining proper phosphate levels include dietary transgressions, insufficient dialysis –primarily in the form of duration–, short dialysis sessions with low convective transport, excessive doses of vitamin D –both native and active forms–, and severe secondary hyperparathyroidism.5-7 However, there is also another cause for this poor control, which in our opinion is of great importance and often overlooked, in the form of therapeutic non-compliance with PB treatment.
There is always a certain degree of poor therapeutic compliance (TC) in any type of treatment, but this issue is much more marked in chronic treatments that involve multiple pills and poor digestive tolerance. Such is the case with PB. Studies have situated the rate of poor adherence to PB treatments around 50%.8,9 The typical profile of non-compliant patients with PB prescriptions are young patients with few comorbidities and a greater number of pills prescribed. In the study by Arenas et al.,8 patients who were prescribed PB and did not like taking treatment had worse control of serum phosphorous levels and worse TC. These authors concluded that an awareness of patient preferences towards the medications prescribed could be an essential factor in achieving greater compliance with treatment.
In several studies, adherence to treatment has been discussed rather than TC. The word “adherence” is preferable for many authors, because “compliance” suggests that the patient passively follows the doctor’s orders and the treatment plan is not based on a treatment alliance or contract that is established between the patient and doctor. In our study, we use both terms synonymously.
The objective of our study was to evaluate TC or adherence to treatment with regards to phosphate binders in patients on HD with hyperphosphatemia (serum phosphorous levels >5mg/dl). Our secondary objective was to evaluate improvements in TC among patients who initially had low adherence to treatment, less than 75%, after starting strategies for optimising treatment.
MATERIAL AND METHOD
Study design
Ours was a multi-centre, epidemiological registry of a series of cases with prospective data collection.
Patients
Our study included a total of 181 patients derived from 13 Spanish HD units.
The inclusion criteria used for our study were adult patients, older than 18 years of age, with CKD, on HD, who had hyperphosphatemia (phosphataemia greater than 5mg/dl), and who required treatment with any of the available forms of PB. We collected informed consent from all patients prior to applying the appropriate questionnaires in order to study patient data according to the regulations of the Data Protection Agency.
We only excluded patients who did not give consent or did not have complete data from evaluations made at the baseline visit (BV).
Methodology
During the BV, the following laboratory parameters were assessed: glycaemia, haemoglobin, leukocytes, glutamate-oxaloacetate transaminase [GOT], glutamate-pyruvate-transaminase [GPT], gamma-glutamyl-transferase [GGT], alkaline phosphatase, calcium, phosphorous, parathyroid hormone [PTH], and potassium. We also compiled data on the following demographic and clinical parameters: sex, age, time on HD, aetiology of CKD, body mass index [BMI], abdominal circumference, predialysis systolic and diastolic blood pressure, and inter-dialytic mid-week weight gain. We evaluated biochemical parameters, concomitant medications, and TC with PB every month until reaching 6 months (visit 5) using the following methods: 1) interview with the physician to evaluate the percentage of prescribed pills actually ingested; 2) SMAQ scale (Simplified Medication Adherence Questionnaire) results, and 3) phosphataemia greater than 5mg/dl.
We considered patients to be non-compliant (NCP) if less than 75% of pills prescribed were actually taken, a score on the SMAQ questionnaire that corresponded to “non-compliant”, and that had a phosphataemia level greater than 5mg/dl.
Patients that were compliant with treatment at the BV were then removed from the study; non-compliant patients continued through the 6 months of follow-up.
Strategies used to improve TC were: 1) change of phosphate binder prescribed based on patient preference; 2) education regarding the importance of treatment; 3) insistence and control of treatment, and 4) increased doses of PB.
We also registered on a monthly basis all adverse events and actions taken by the attending physician.
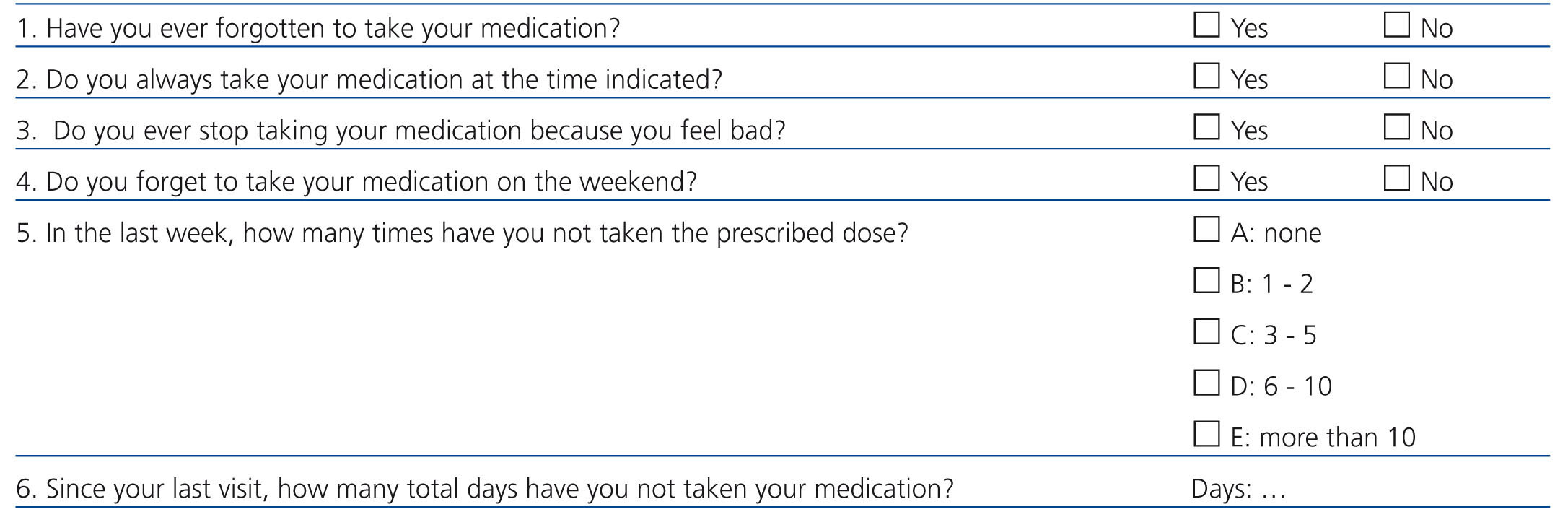
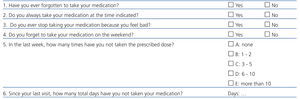
The SMAQ scale is summarised in Table 1. This scale has been validated and tested in patients with AIDS10 and in kidney transplant recipients on treatment with tacrolimus.11 It has also been used to evaluate TC with PB in patients on HD.8,12 The response variables are dichotomic; any response in the sense of non-compliance is considered to be a lack of adherence to treatment. This questionnaire has been shown to provide sufficient internal consistency in previous studies.
Study variables
The primary study variable was the percentage of patients on HD under treatment with PB who reported inadequate TC in a medically unacceptable context, a “non-compliant patient” (NCP).
Secondary study variables included the percentage of patients who, with poor BV adherence, reached good adherence at 4, 8, 12, 16, 20, or 24 weeks after entering the study.
In the patients who remained in the study for the 6-month follow-up period, we measured TC, PB used, type and dose, and evolution of phosphataemia based on what type of PB was used on a monthly basis. We also evaluated calcium, PHT, alkaline phosphatase, serum levels of hepatic enzymes (GOT, GPT, and GGT), dose of vitamin D, and calcimimetics on a monthly basis.
Statistical analysis
We performed a descriptive statistical analysis. Qualitative variables were presented with frequency distributions. Quantitative variables were summarised in the form of mean and standard deviation or median and interquartile range (p25-p75) in the case of asymmetric data distribution.
We evaluated the relationship between qualitative variables using chi-square tests or Fisher’s exact tests, in the event that more than 25% of expected values were less than 5.
We compared quantitative variables using Student’s t-test (in comparisons of single variables with two categories), and medians were compared using non-parametric median tests. In the case of paired samples, we used paired t-tests or non-parametric tests.
In all cases, we evaluated the distribution of the data based on theoretical models, contrasting actual distributions against the hypothesis of homogeneity of variance.
In all cases, the null hypothesis was rejected based on a type I error less than 0.05.
We used SPSS statistical software for Windows, version 18.0, for all analyses.
RESULTS
Baseline visit
Our study included a total of 181 patients. During the BV, 39.2% (n=71) of these were compliant with treatment prescriptions and left the study. The remaining 60.8% (n=110) were non-compliant and continued through to the last visit. Of the NCP, half left the study due to various reasons, such as kidney transplant, transfer to a different centre, hospitalisation, death, or loss of follow-up.
We examined a total of 103 males and 78 females, with a mean age of 59.9 (21-86) years. The causes of CKD were diabetes (21.5%), arterial hypertension/vascular causes (13.8%), glomerulonephritis (13.8%), tubulo-interstitial nephritis (11.6%), adult polycystic kidney disease (6.1%), other causes (12.7%), or unknown. The time spent on HD was a median 29 (12-68) months. Mean BMI was 25.2 (5.2) kg/m2, and median abdominal circumference was 95.5 (70.5-104) cm. In addition, 14.1% of patients were obese. Mean pre-HD systolic blood pressure was 134 (22.3) mm Hg, and mean diastolic blood pressure was 71.3 (12.8) mm Hg. We considered 47% of all patients to be hypertensive. Mean weekly inter-dialytic weight gain was 2.3 (0.97) kg.
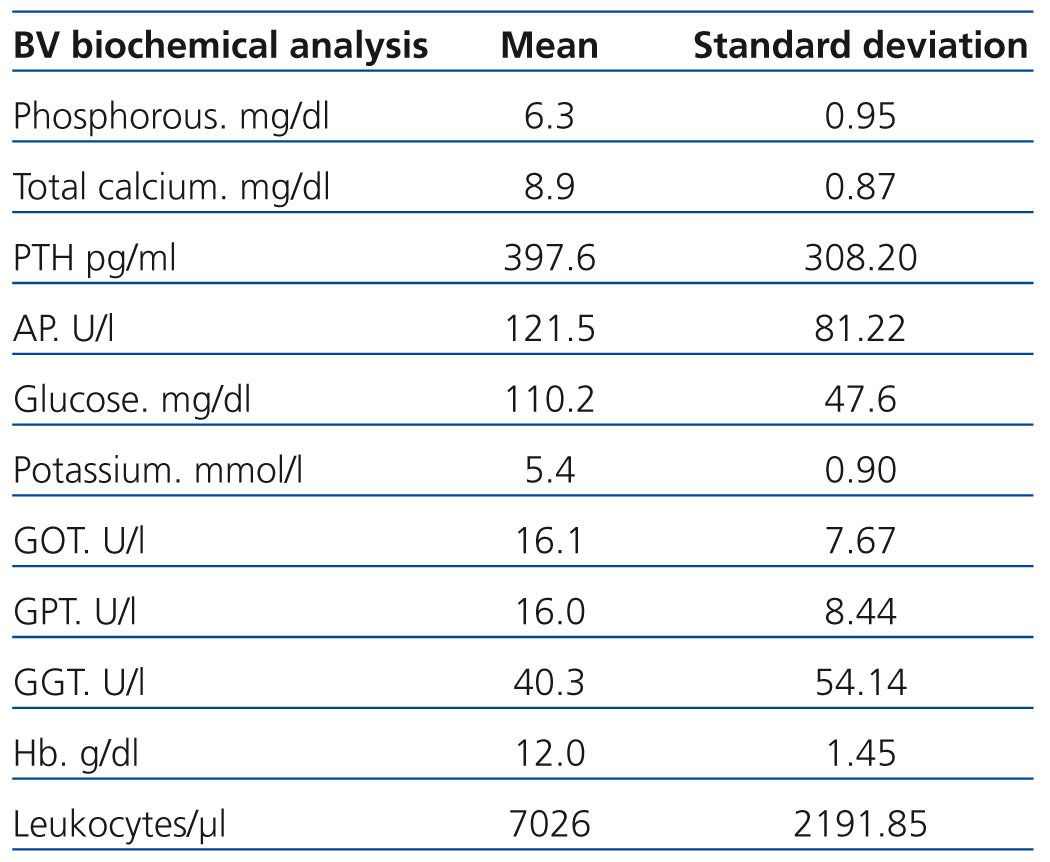
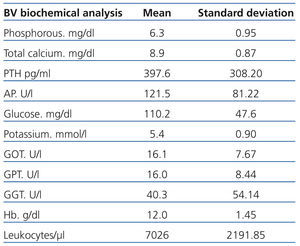
Table 2 describes the results for laboratory tests at BV. Glycaemia was above 125mg/dl in 25% of patients.
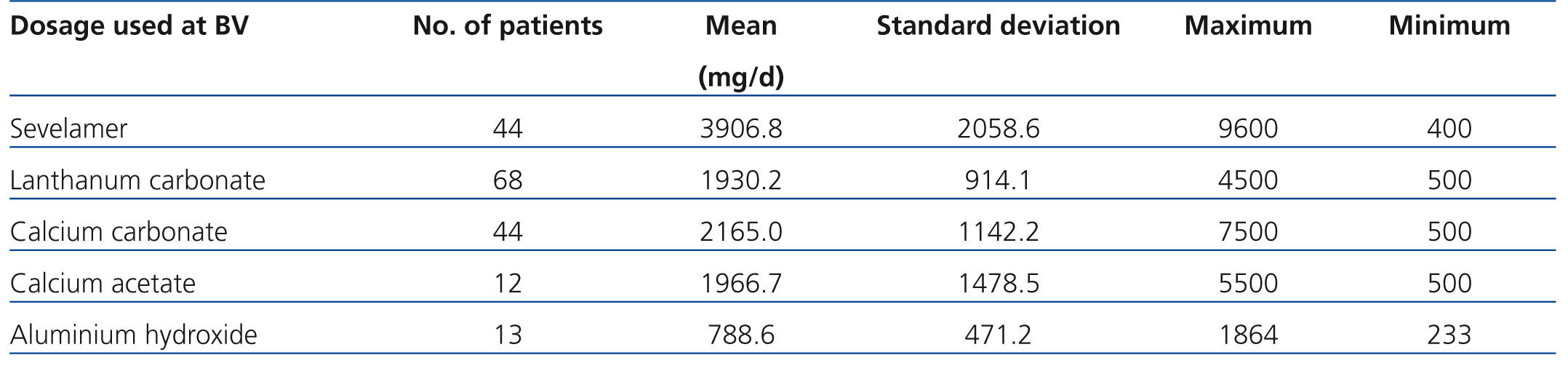
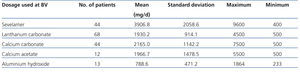
Table 3 summarises the primary phosphate binders used and their doses. Patients were prescribed an average of 3.44 pills per day in the initial PB prescription. The most commonly prescribed binder at the BV was lanthanum carbonate (37.6% of patients). Table 4 describes the most commonly used combinations of PB. At least 2 different types of PB were prescribed in 43.6% of patients, and 7.1% were prescribed 3 types. Of the 181 patients evaluated in the BV, 56 were receiving calcimimetics and 53 were receiving vitamin D.
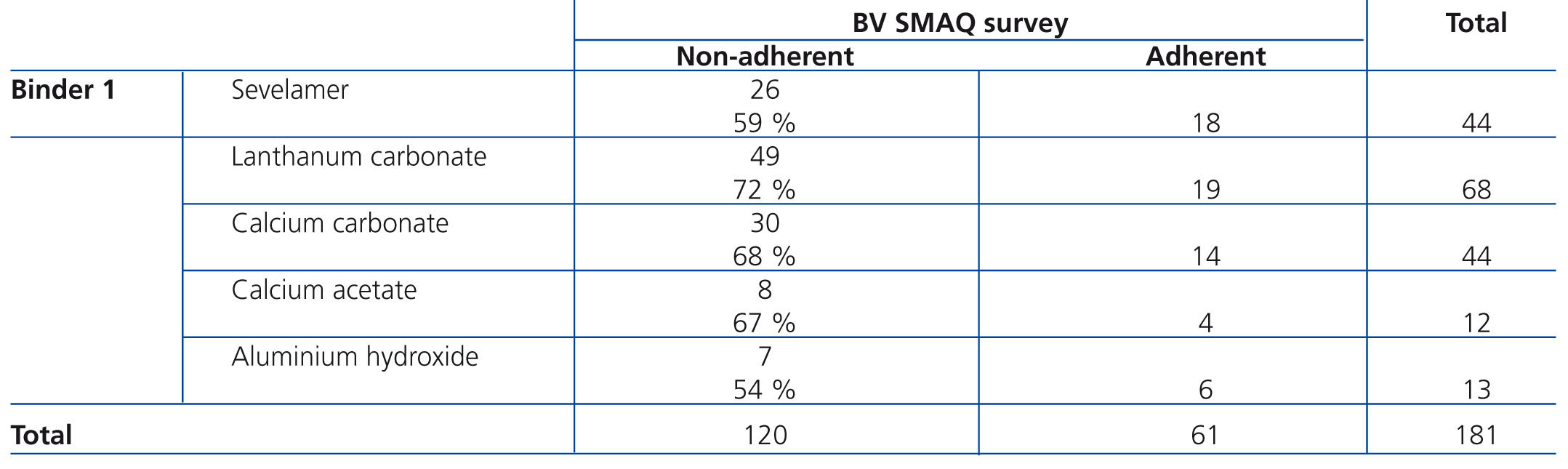
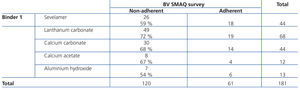
Younger patients were more likely to be NCP than patients older than 60 years of age (χ2: 7.0 P=.019). Non-compliance with treatment was not correlated with sex, education level, aetiology of CKD, BMI, blood pressure, or inter-dialytic weight gain. There were no significant differences in the proportions of compliant and non-compliant patients when comparing between the different PB used. Table 5 summarises the results of the SMAQ questionnaire based on the primary phosphate binder used.
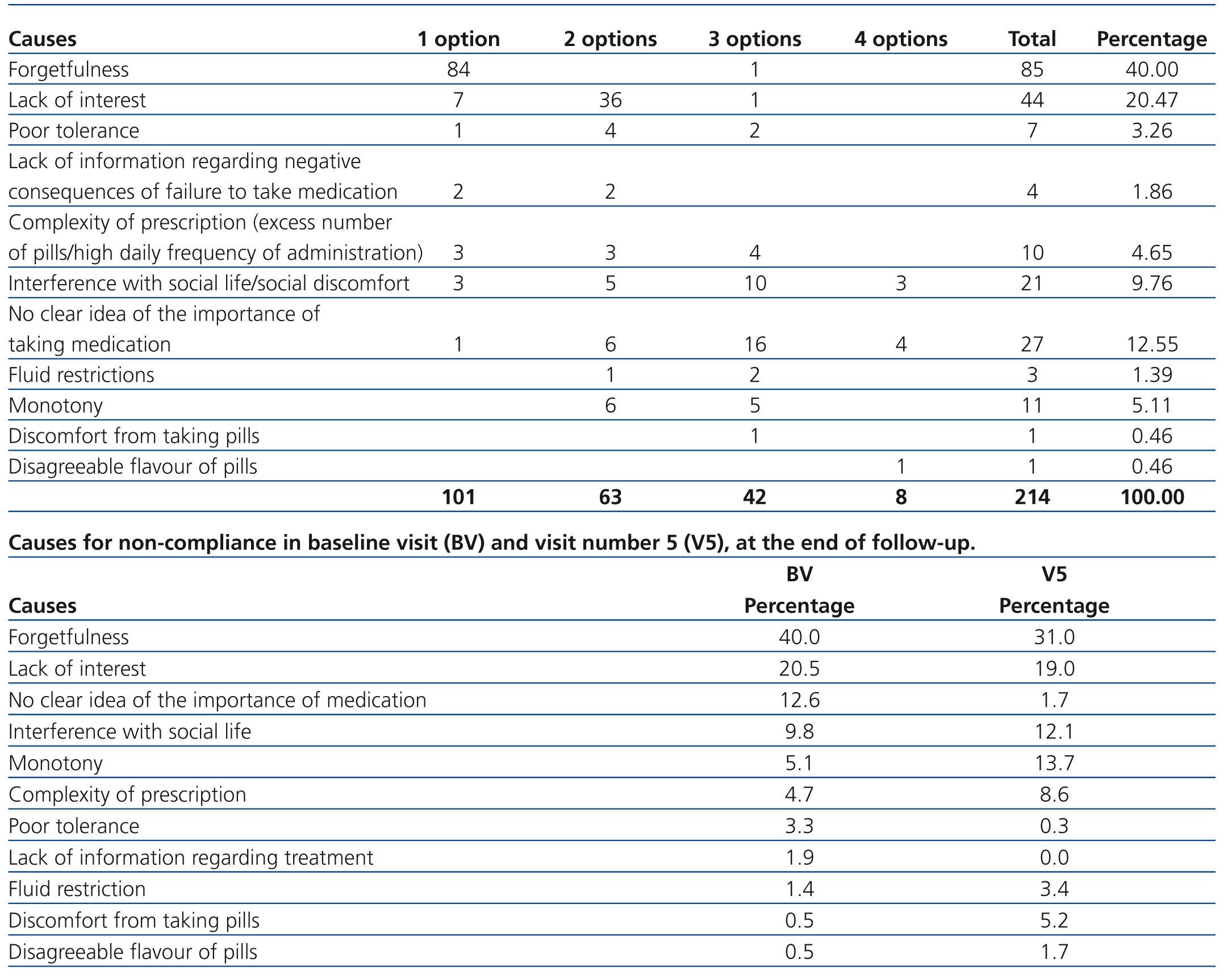
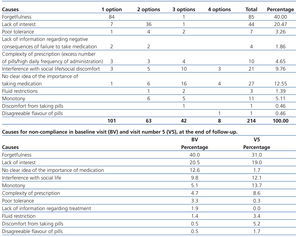
The causes for non-compliance reported by the NCP are compiled in Table 6.
During follow-up, NCP (n=110) continued through the six months of the study. A mean 27.3% of these patients became compliant over the course of the five visits (V1-V5), with 28.8% compliant at the last visit. Table 7 shows phosphorous (P) levels and TC over the course of the 5 visits. P levels decreased by a mean of 1.26mg/dl during the study period (P<.0001). During the 6 months of follow-up, no changes were observed in calcaemia or PTH levels.
During the 6 months of follow-up, 41% of patients switched phosphate binders and 59% remained with the same prescription. Lanthanum carbonate continued to be the most frequently used PB, at 58.5% of patients, followed by sevelamer at 14.6%. During follow-up, the number of pills taken increased from a mean 2.75 per patient at the BV to 3 per patient at visit 5 (V5) in the case of lanthanum carbonate, and from 4.82 to 5.62 in the case of sevelamer. The number of pills taken for the primary PB increased from a mean 3.5 (1.8) to 3.8 (2) per patient, although this difference was not statistically significant.
At the end of the study, the explanations given by NCP for why they did not take PB were somewhat different from those given at the start of the study (Table 6). Forgetfulness had decreased by 9%, a lack of comprehension of the importance of the medication decreased by 10.9%, and lack of interest decreased by 1.5%, whereas monotony increased by 8.6%, complexity of prescriptions increased by 3.9%, and social reasons increased by 2.4%.
DISCUSSION
In our study, the percentage of non-compliant patients was very high, at 60.8%, which was surely related to the selection of the study population, this being composed of patients with poor control of P levels.8,9 This implies that therapeutic non-compliance is a fundamental factor in the poor control of P in patients on HD. The measures taken to improve TC with PB resulted in one-fourth of non-compliant patients reaching compliance after the second month, thus lowering phosphataemia significantly in all patients. This is probably not a dichotomic variable in the sense of compliant/non-compliant in true clinical practice, but rather one of a range of levels of compliance that would influence the final level of control of phosphataemia. In the BV, 100% of patients had poorly controlled P levels, whereas this percentage lowered to 50% in subsequent visits.
In our study, the only factor associated with TC was age. This implies that attitudes concerning life and disease must influence compliance more than any other parameter evaluated here. It also appears that compliance was not associated with other forms of therapeutic non-compliance related to diet, such as sodium and water intake. In this sense, neither inter-dialytic weight gain nor blood pressure was correlated with TC for PB. These two parameters tend to be discussed with the patient during visits both by the attending physician and the nurse. This more frequent interaction undoubtedly plays an important role in TC. In the case of PB, compliance tends to be discussed only when specific analyses are performed, which in the majority of cases occurs less than once per month.
In the USA, patients on HD miss 2.3% of sessions, whereas in Japan and Spain, this value is close to 0%. Also in the USA, there is a correlation between the number of HD session missed, weight gain, and hyperphosphatemia (>7.5mg/dl) and mortality.13,14 As such, there is an important variability between countries in this context, which hinders extrapolation of study results.
We did not observe significant differences in terms of TC between patients that were prescribed different types of PB, as has been reported in other studies.8 We must point out that in our study, many patients were prescribed more than one type of phosphate binder and on occasion three, which impedes an evaluation of TC based on PB. During follow-up, many patients switched to lanthanum carbonate, which coincided with improved P control and better TC, but again, this relationship did not reach statistical significance, probably due to the same reason as before: the combination of multiple PB.
It would seem reasonable that the road to improving TC should start with understanding the causes of non-compliance. The primary causes reported in our study can be grouped into forgetfulness, lack of interest, and lack of information regarding the importance of proper medication. These three causes were blamed for 3 out of 4 cases of non-compliance. Complexity of treatment per se is not the primary factor in the lack of TC.8 NCP could have a greater understanding of the usefulness and importance of these medications.8,12 In the USA, 69% of patients receive more than 11 medications, and 91% of these are well informed. The number of medications and costs of medication are correlated with TC.15 It may be that in Spain, with decreased coverage of drug costs, therapeutic non-compliance may increase.
This gives way to the idea that what is lacking is a better level of concordance between patient behaviour and the recommendations made by the prescribing physician. Based on the concept that the patient has the right to reject treatment, and that lack of compliance does not necessarily put the blame on the patient, an agreement between the physician and patient is needed as well as a system for monitoring compliance with this agreement. If the patient decides not to take the pills, why prescribe them? Clear instructions on how to take PB have proven to be insufficient. When prescribing a treatment based on PB, we must take into account patient expectations, beliefs, and preferences.
With the follow-up carried out in our study, TC and P control improved in these patients, but we must point out that there continued to be an important proportion of NCP. We must also consider the possibility that many of the patients who were initially compliant in the BV and thus excluded from follow-up may have later become non-compliant. As such, we must consider the presence of time periods of non-compliance, rather than referring to NCP as a general category. This reinforces the idea that frequent monitoring and follow-up of treatment plans is key for improving results in TC, and as such, control of P. We must take into account that PB as a group are the most expensive drugs that patients on HD tend to require,4,16 further highlighting the importance of optimising this type of treatment.
Various clinical measures have also been described for improving TC,17-19 which are primarily educational in nature. In our study, we insist on the importance of follow-up of compliance with treatment with patient-doctor contact on at least a monthly basis. In this aspect and in HD in general, the role of the nursing staff could be especially important.
CONCLUSIONS
In patients on HD with poorly controlled P, we observed a low rate of baseline TC for PB, at 39.2%. Forgetfulness and lack of interest are the primary causes of non-compliance. With various strategies, including switching to another binder (primarily lanthanum carbonate) and insistence by medical staff, improvements in TC and phosphataemia can be obtained. Decreases in P are greater in compliant patients than in non-compliant patients.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 6. Reasons given by the patients to explain non-compliance with phosphate binder treatment during the baseline visit and visit number 5
Table 1. SMAQ questionnaire
Table 2. Biochemical parameters in the 181 patients during basal evaluations
Table 3. Primary binders used and doses at baseline visit
Table 5. Results of the SMAQ questionnaire during the baseline visit arranged by the primary binder used
11726_19157_41508_en_table_4.doc
Table 4. Most commonly used 2-binder combinations
11726_19157_41618_en_11726_tabla7.doc
Table 7. Relationship between phosphate levels and compliance with treatment during the 6 months of follow-up (BV V5)