Chronic kidney disease is considered to be a problem of public health problem from the application of Guidelines KDOQI/NKF. Majority patients diagnosed of chronic kidney disease are elderly. In these patients progression of renal disease is slow, being the mortality high to development of renal failure that needs dialysis. The current guidelines must apply with caution in these elders.
La enfermedad renal crónica se considera un problema de salud pública desde la aplicación de las Guías KDOQI/NKF. La mayoría de los pacientes diagnosticados de enfermedad renal crónica son ancianos. En estos pacientes la progresión de la enfermedad renal es lenta, y la mortalidad superior al desarrollo de una insuficiencia renal que requiera el empleo de diálisis. Las guías actuales deben aplicarse con cautela en estos ancianos.
INTRODUCTION
The improvement in health care has contributed to the increase in life expectancy. Along these lines, in the European Union, adults of 60 years of age and older comprise 21% of the population, and it is estimated that this number will rise to 33% by 2050. Therefore, this gradual increase in the geriatric population will have a medical, social and economic impact.1
Chronic kidney disease (CKD) is currently recognised as a major public health problem, and is now considered to be an “epidemic”.2 This acknowledgment has been possible since the application of the conceptual model established by the KDOQI (Kidney Disease Outcomes Quality Initiative) guidelines of the NKF (National Kidney Foundation).3 This classification is defined by the presence of kidney damage (haematuria, proteinuria, changes in imaging tests) or by a glomerular filtration rate (GFR) less than 60ml/min for three or more months, and it is divided into five stages.3,4 The purpose of this classification is to identify the patients with CKD in its earliest stages, set out measures to slow down its progression, reduce morbidity and mortality and prepare patients for dialysis. This classification is considered to be applicable to the entire population.
Outcome of CKD is marked by the following aspects: a) loss of kidney function: development of end-stage renal disease (ESRD) requiring renal replacement therapy (RRT); b) appearance of complications associated with a decrease in the GFR; and c) increase in cardiovascular risk.5
However, outcome implications of CKD in the elderly are rather unclear and less well known6: a) The age entails certain morphological changes in the kidneys and a decrease in renal function (RF),1 which need to be taken into account when diagnosing CKD in the elderly; b) How does CKD progress in the elderly?; c) Is the development of ESRD requiring RRT common?; and d) What is the outcome of CKD concerning mortality in the elderly?
In this review we include the structural and functional changes that take place in the kidneys of the elderly. We also analyse the estimation methods of the GFR in the elderly and its influence on the prevalence of CKD. Finally, we examine the clinical importance and outcome of CKD in this population group.
CHANGES IN THE KIDNEYS OF THE ELDERLY
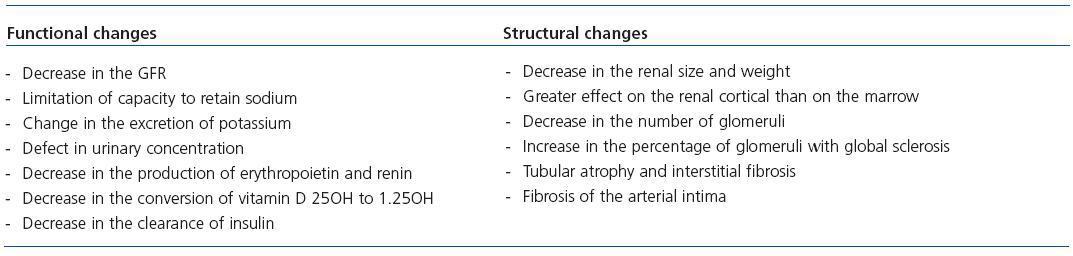
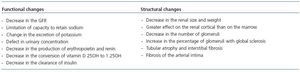
The structural and functional changes in the kidneys of the elderly can be found in Table 1.
Functional changes
The age-related decrease in the GFR is associated with a drop in the renal blood flow, a damage to the renal concentrating capacity, pathological findings of global glomerular sclerosis, vascular sclerosis, tubular atrophy and a decrease in cortical activity and kidney size7,8. The longitudinal Baltimore study showed a decrease in the GFR (estimated by the creatinine clearance rate) at a rate of 0.75ml/min/year among 254 “normal” volunteers in a follow-up carried out from 1958 to 1981, although a third of the subjects maintained a stable creatinine clearance rate (CCr).9 Therefore, the decline in RF with age can be clinically insignificant, unless other acute/chronic diseases that affect the reserve or the RF are overlapped, since in the elderly the presence of other comorbidities associated with CKD, such as arterial hypertension, type 2 diabetes mellitus, congestive heart failure or cognitive impairment, is very common.1
Among the changes in tubular function associated with age, we emphasise the following: a limitation in the capacity to retain sodium, thus the elderly are more susceptible to volume depletion;10 a change in the capacity of excreting potassium, which explains the predisposition of the elderly to develop medicine-related hyperpotassaemia;1 and the ability to concentrate or dilute urine diminishes with age,11 which explains the common nocturia in these patients and the predisposition to dehydration, hypernatraemia and hyponatraemia if an excess in fluids is administered.
Some of the age-related renal changes associated with endocrine function include the decrease in the production of renal erythropoietin, as well as a drop in the production of renin, which reduces the conversion of vitamin D 25OH to 1.25OH and leads to a decrease in the clearance of insulin that is also associated with a drop in RF in the elderly.1
Structural changes
The weight of the kidneys gradually decreases after fifty years of age, with greater effects on the cortex than on renal medulla.12 Similarly, as age increases the number of glomeruli decreases, with an increase in the percentage of glomeruli with global sclerosis. It has been indicated that “pathological” glomerulosclerosis could be brought on when the number of glomeruli with global sclerosis exceeds the number calculated using the following formula: (the patient’s age/2)-10. Tubular atrophy and interstitial fibrosis could be associated with age or could be caused by a chronic inflammation or vascular disease. Furthermore, there is a fibrosis of the intima of interlobular arteries associated with age, which could be aggravated by the presence of arterial hypertension and diabetes mellitus.1
ESTIMATION OF THE GLOMERULAR FILTRATE RATE IN THE ELDERLY
It is established that the GFR is the best marker for RF.13 One of the benefits of knowing the GFR is the correct adjustment of the medicine dose excreted by the kidneys. Another more recent use was to define CKD in its different stages.3
The exact measurement of the GFR, using exogenous markers, such as inulin or iothalamate, is not usually carried out in clinical practice (it is time-consuming and entails high costs).14 On the other hand, endogenous markers, such as serum creatinine or, recently, cystatin C, have been used to estimate the GFR4: serum creatinine has the disadvantage of being a marker of the GFR, of muscle mass and of protein ingestion; cystatin C is a 13-kD protease inhibitor that is produced in all cells, is filtrated by the glomerulus and is catabolised in the tubules with a small urinary excretion.4 Numerous studies have mentioned that the level of cystatin C is the best indicator of adverse effects or of the GFR than serum creatinine, particularly in the elderly.15
The CCr is frequently used to evaluate the GFR in clinical practice through a urine collection within 24 hours. However, its disadvantage is that it slightly overestimates the GFR due to the tubular secretion of creatinine, and in the elderly its collection can be time-consuming (due to incontinence).16
Recently, mathematical formulas are being used, derived from serum creatinine, to obtain the GFR, taking into consideration the classification of CKD according to the KDOQI guidelines.3 The Cockcroft-Gault (CG) equation has been validated versus the CCr as the gold standard and has been the traditional estimation method for the GFR to adjust drug doses.13,16 The Modification of Diet in Renal Disease (MDRD) equation has been developed in a group with altered RF.16,17 However, none of these estimation formulas for the GFR have been validated in the elderly1,18: the use of the MDRD equation in healthy people (without CKD) can underestimate the GFR (healthy people have more muscle mass and a higher protein ingestion and, therefore, generate more creatinine than people with CKD).19 As a result, we could categorise the “healthy” elderly as affected by CKD by obtaining a reduced GFR when using the MDRD equation systematically.
Various studies show significant variations in the grade of the GFR obtained in the same group of patients according to the formula used: in general, the MDRD equation overestimates the GFR compared with the CG equation.13,20,21 The use of the MDRD equation instead of the CG equation for drug adjustment could lead to fewer patients requiring an adjustment and could produce an unforeseen pharmacological toxicity.1,13 Therefore, some studies conclude that the use of the CG equation is preferred for the pharmacological adjustment.13
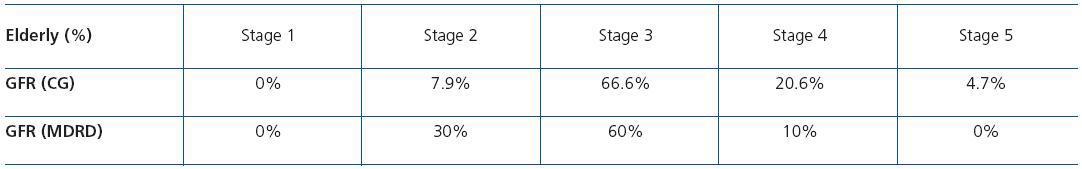
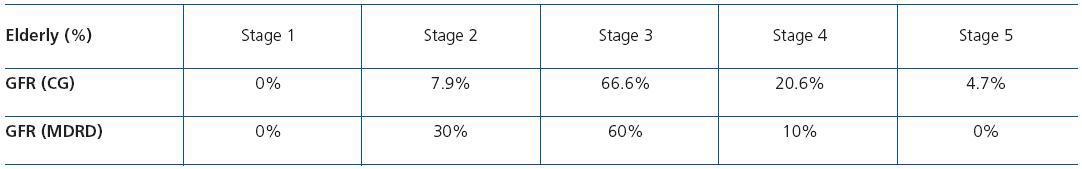
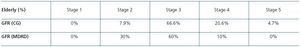
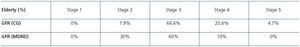
On the other hand, the use of these formulas could give rise to conflicting estimations with the resulting error in the staging of CKD. Gill et al. found that less than 40% of the patients were classified in the same stage according to the formula used.13 The discrepancies that exist in the distribution of the stages of CKD, produced in the study of 80 elderly patients with CKD at the Segovia General Hospital according to the estimation formula used, can be seen in Table 2 22
PREVALENCE OF CHRONIC KIDNEY DISEASE
The presence of a reduced GFR (less than 60ml/min) is sufficient to diagnose a patient suffering from CKD – at least in stage 3 – with the current classification.3 However, age is one of the main factors affecting renal function. Therefore, the prevalence of CKD greatly varies with age. Zhang, Rothenbacher23 carried out a systematic review of 26 studies of different groups in order to understand the prevalence of CKD, with the number of participants in the studies ranging from 237 to 65,181, and reached the following conclusions: a) the average prevalence of CKD is 7.2% in the youngest population, while in the elderly it ranges between 23.4% in the study by Manjunath24 and 35.7% in the study by Hemmelgarn;25 b) the prevalence varies according to the estimation method used for the GFR: in the Finnish study26 the prevalence of CKD based on a GFR less than 60ml/min and calculated using the MDRD equation was 35.8%, whereas this rate increased to 58.5% when the Cockcroft-Gault equation was used in the same patients; and c) the exact detection of CKD in specific groups, particularly the elderly, is insufficient.
OUTCOME IMPLICATIONS OF CHRONIC KIDNEY DISEASE IN THE ELDERLY
The guidelines recommend that the same criteria of the KDOQI classification are used to detect CKD in both young people and the elderly.3,27 Along these lines, all patients, regardless of their age, are considered to present with moderate CKD if they have a GFR less than 60ml/min/1.73m2. However, in the elderly we need to take into account that the decrease in the GFR is very common (associated with age) and that the formulas used to estimate the GFR in this group have not been validated.1,13
The outcome of CKD is marked by a loss in RF requiring RRT.3 The decrease in the rate of RF varies among patients; a rapid progression is defined by a drop in the GFR higher than 4ml/min/year.5 The success and prevalence of RRT has increased in most industrialized countries: one of the main factors has been the success of RRT in the elderly.18 However, according to the data of NANHES III, it is considered that of the 20 million patients suffering from CKD, only approximately 2% receive RRT with dialysis or transplantation.28
Meanwhile, the systematic introduction of the MDRD equation in laboratories to understand the population’s GFR according to the KDOQI guidelines is causing a considerable increase in referrals to nephrologists – particularly in elderly patients with a reduced GFR but no other common symptoms of renal failure (anaemia, proteinuria, etc.)29 – thus giving rise to concern and discussion among health professionals about the advisability of systematically using this classification in the elderly and its outcome importance.30-32
HOW CHRONIC KIDNEY DISEASE PROGRESSES IN THE ELDERLY
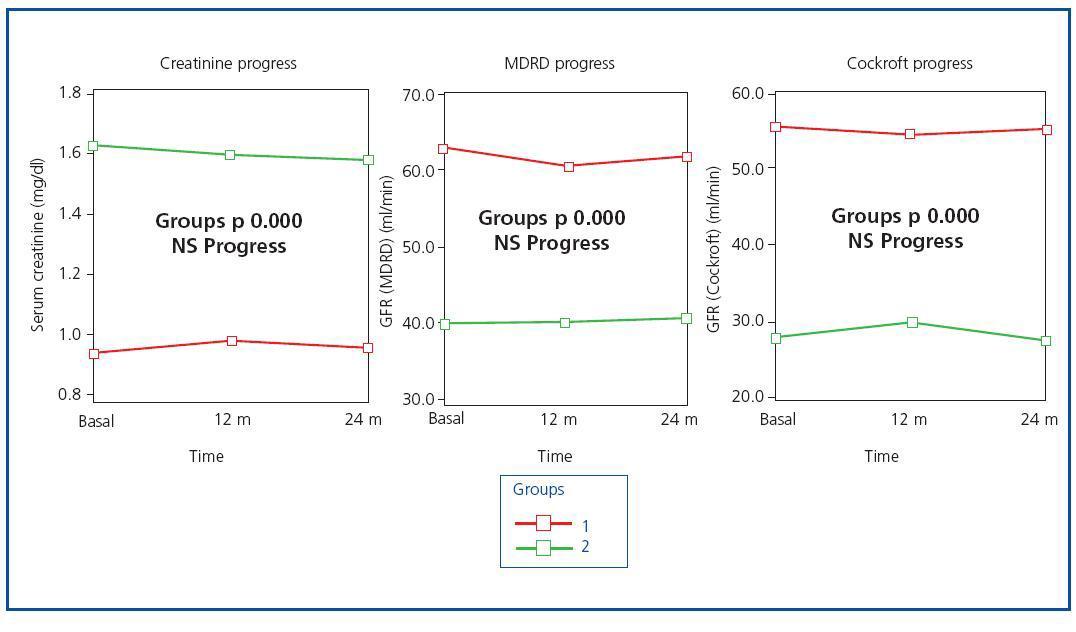
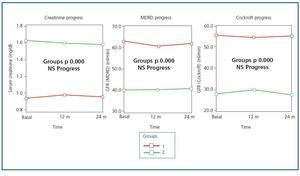
The decrease in the GFR in healthy elderly people is very common9 due to the changes in the renal structure associated with age. Various studies have been carried out in order to understand the prevalence of CKD in the population.23 On the other hand, few studies have analysed the progression rate of kidney disease in the elderly. Hallan et al.33 studied the strategies for the detection of CKD in the general population over 20 years of age, with an eight-year prospective follow-up. By evaluating the natural course of CKD they found that the risk of progression to ESRD is particularly low in patients without diabetes or hypertension (HT), in women and in patients with an age of >70 years or with a GFR between 45 and 59ml/min during the screening. Among the few specific studies carried out in the elderly population, the study by Hemmelgarm et al.25 describes the progression of CKD in the course of a two-year follow-up in a group of patients older than 66 years of age, and it observes that this progression is slow except in diabetic patients and in the cases where the GFR is less than 30ml/min. In accordance with these results, in our study of CKD, carried out in 80 elderly patients at the General Hospital of Segovia, we also detected stability in RF after a 24-month follow-up34 (figure 1).
OUTCOME OF CHRONIC KIDNEY DISEASE: RENAL REPLACEMENT THERAPY AND MORTALITY
In most studies that carry out a prospective follow-up of patients diagnosed with CKD, we found that the development of ESRD requiring RRT is a less common outcome than mortality.28,34,35 The results of the outcomes obtained in various studies can be found in Table 3. O’Hare et al.6 observed a similar pattern in a study carried out in 209,622 American veterans with stages 3 to 5 CKD and with a 3.2-year follow-up, and describe the “modifying age effect” on CKD: among the patients with comparable baseline GFR levels the results showed that as age increased, the patients presented with greater chances of dying than with having ESRD that required RRT compared with the younger patients. In a cohort group of patients diagnosed with stage 4 CKD,
Conway et al. analyzed the predictive factors of mortality and the need for RRT, and found that the survival risk that requires dialysis decreases as age increases, partially due to the low decrease rate of RF in the elderly. They also included the presence of proteinuria, the high decrease rate in the GFR (>4ml/min/year), the low baseline levels of the GFR and the levels of haemoglobin less than 10g/dl as predictive risk factors of RRT.36 Along these lines, the death of patients is also caused by other reasons that arise before renal failure occurs.35,36
Concerning mortality causes, cardiovascular disease is the most common cause in patients in dialysis and with a transplant.37 In a recent study, Roderick et al. showed that in people older than 75 years of age there is an increased mortality risk that is independent of all causes and specifically cardiovascular disease.38 In the study by Keith et al., the patients who passed away presented with a greater prevalence of heart disease, congestive heart failure, diabetes mellitus and anaemia in relation to those who lived.28 In the study of the elderly patients at the General Hospital of Segovia, although the main final cause of death was gradual deterioration, when analysing the presence of previous cardiovascular attacks it was also found that those who passed away had a significantly higher percentage of previous heart failure attacks, ischaemic heart disease and peripheral arteriopathy compared to those who lived.34
Therefore, considering this pattern of high mortality rate in the elderly with CKD, some authors suggest that an intensive approach (prevention and treatment) to reduce cardiovascular risk should be carried out in all patients with CKD, before renal failure requiring dialysis develops.35,39,40 On the other hand, not all elderly patients diagnosed with CKD should receive special “treatment” at nephrology departments in order to try to slow down the progression of kidney disease (in these patients the benefits are fewer than in younger people).25,35
KEY CONCEPTS
1. The presence of a decreased GFR is very common in the “healthy” elderly people associated with the “age effect”.
2. The prevalence of CKD greatly varies with age and with the estimation method of the GFR: prevalence increases when using the Cockroft-Gault equation compared with the MDRD equation.
3. The GFR levels obtained using the MDRD equation are greater than those obtained by the Cockcroft-Gault equation, with an impact on the staging of CKD and when adjusting the medicines in renal failure.
4. The progression of CKD in the elderly without proteinuria is slow.
5. In the elderly there is a higher mortality risk than a “renal failure” risk requiring RRT.
6. Only one small proportion of elderly with CKD will need RRT: elderly with proteinuria, diabetics and with a baseline GFR less than 30ml/min. These patients are those benefiting from the care offered during examinations at nephrology departments.
7. Intensive therapy should be carried out in all elderly patients with CKD to reduce cardiovascular risk.
8. The KDOQI guidelines of the NKF should be used with caution in the elderly.
KDOQI GUIDELINES OF THE NKF ON CHRONIC KIDNEY DISEASE
The fact that the presence of a GFR less than 60ml/min is common in the elderly population,18 as well as the low rate of progression of CKD25,34 with a high mortality risk regarding the development of ESRD requiring RRT,34,36 have led some authors to suggest that these guidelines should be used with caution in the elderly.19,30,34,36,41
To conclude, due to the fact that CKD is very common in the elderly, with a slow decline in RF in most of them, the possibility of having renal failure requiring RRT is much smaller than the risk of dying: the current guidelines should take into account the “age” effect on the outcome of CKD in this population group.
Table 1. Functional and structural changes in the kidneys of the elderly
Table 2. Distribution by stages according to estimation methods of the GFR
Table 3. Outcome: ESRD and mortality
Figure 1. Evolution of renal function at 24 months